Woman's hormones
introduction

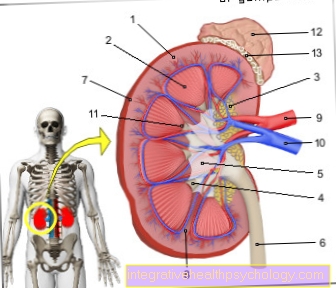
The woman's hormonal system is determined by a control circuit consisting of the hypothalamus, the pituitary gland (pituitary gland) and the ovaries (ovaries). The woman's ovaries are the central organ for the production of the female sex hormones estradiol and progesterone as well as fertility in women. Only a functioning interaction between the ovaries, the hypothalamus, the pituitary gland (pituitary gland) and the uterus (uterus) ensures unimpaired fertility.
The female sex hormones estradiol and progesterone belong to the class of Steroid hormones, from cholesterol getting produced. This class of hormones is able to cross cell membranes and can thus develop its effect by binding to receptors inside the cell. Usually, hormones work by binding to receptors on the cell surface because they are unable to cross cell membranes. Since these steroid hormones are well soluble in fat, but only sparingly soluble in water, they are used for transport in the blood mostly on Egg whites bound. Only 1% of the estrogens and 2% of the progesterone are free, can cross cell membranes and develop their effects. Therefore, the free hormones are also called biologically active.
The proteins to which the steroid hormones are bound include, for example Sex hormone binding globulin (SHBG), albumin and Transcortin (CBG). For the production of female sex hormones, but also other hormones, the hormones from the hypothalamus and pituitary gland are crucial. Stimulating ("releasing") Or inhibitory ("inhibiting“) Hormones are produced in certain areas of the hypothalamus regardless of gender and are responsible for releasing hormones from the hypothalamus Anterior lobe of the pituitary gland, also known as Adenohypophysis. Hormones whose release is influenced by stimulating ("releasing") or inhibiting ("inhibiting") hormones from the hypothalamus are: the Gonadotropins LH (luteinizing hormone) and FSH (follicle-stimulating hormone), Growth hormone (Somatotropin or HGH / GH, from English for Human Growth Hormone / Growth Hormone), PRL (Prolactin), ACTH (adrenocorticotropic hormone) and TSH (thyroid stimulating hormone).
Lastly, prolactin is also made in the anterior lobe of the pituitary gland. Its release is mainly due to a stimulating hormone, Thyrotropin Releasing Hormone (TRH) from the hypothalamus. The biochemical messenger substance Dopamine however, it inhibits the release of prolactin. Dopamine is the most important regulator of prolactin release and is therefore also called Prolactin inhibiting factor designated. Two other hormones are produced directly in the hypothalamus and in the Posterior lobe of the pituitary gland, also known as Neurohypophysis, transported. These include the hormones ADH (antidiuretic hormone), which is responsible for regulating the water balance and Oxytocin, which in pregnant women for the Labor, the milk weft and the Milk release responsible is. After being transported to the posterior lobe of the pituitary gland, the two hormones are stored there and released when needed.
In the following, the hormones that play a special role in the female organism are discussed in detail. It should be noted that all of these hormones are also present in the male organism and also play a specific role.
Gonadotropin releasing hormone (GnRH)
GnRH is released in a pulsatile, i.e. rhythmic manner, every 60-120 minutes from the hypothalamus and causes the production and release of LH and FSH from the anterior lobe of the pituitary gland. Because of this mechanism, GnRH is one of the stimulating ("releasing“) Hormones of the Hypothalamus. The measurement of the gonadotropin-releasing hormone (GnRH) is normally of no clinical relevance, since only in the connecting veins (Portal veins) there are sustained amounts between the hypothalamus and the pituitary gland.
Gonadotropins (LH and FSH)
The control hormones are also pulsatile from the anterior lobe of the pituitary gland LH (luteinizing hormone) and FSH (follicle-stimulating hormone) secreted (released) when stimulated by GnRH. Because of their primary effect on the Gonads, i.e. the sex glands, they are also called Gonadotropins designated. The release of LH and FSH begins from the puberty, since here the release of the stimulating ("releasing“) Hormone (GnRH) from the hypothalamus starts. The two hormones LH and FSH from the anterior lobe of the pituitary gland stimulate the ovaries and thus stimulate the production of female sex hormones.
A so-called exists between the gonadotropins LH and FSH and the level of the female sex hormones negative feedback. This means that both with a high level of estrogen and a high level of progesterone, LH and FSH are released from the pituitary gland reduced. At a low Levels of estrogen and progesterone in the blood increases the release of LH and FSH, with the aim of increasing the level of female sex hormones again. In this case one speaks of one positive feedback. In the middle of the female cycle, there is a rapid increase in estrogen levels, which in turn triggers a peak in LH release. This large distribution from LH, also known as "LH peak“Is known is responsible for the Entry (ovulation).
In the Menopause the release of LH and FSH is no longer slowed down as usual by the actual sex hormones, since the production of estrogens and progesterone is steadily decreasing. It happens because of Feedback mechanisms a significant increase in LH and FSH levels in the blood. After the menopause, the control hormones of the pituitary gland also decrease again, but remain elevated compared to the time before the menopause. In contrast to the GnRH level, the FSH level can be determined without problems in the blood.
The normal values depend on the stage of life in which the woman is. During puberty, an FSH level of 2-3 mIU / ml is considered normal. In sexual maturity, a distinction must be made between which Cycle phase the blood was drawn. In the Follicular phase (the time between the onset of menstruation and ovulation) values of 2-10 mIU / ml are considered normal in the Ovulation phase, i.e. the time around ovulation, a level of 8-20 mIU / ml is normal and in the Luteal phase (the time between ovulation and the start of the next menstruation) of 2-8 mIU / ml. In the Post menopause FSH levels of> 20 mIU / ml and LH concentrations in the blood between 20 and 100 mIU / ml are found.
Male sex hormones (androgens)
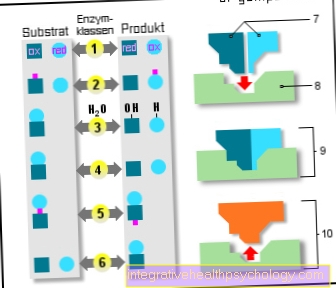
The control hormone LH from the anterior lobe of the pituitary gland stimulates the production of Androgens (male sex hormones). These are produced under the influence of another control hormone from the anterior lobe of the pituitary gland, the follicle-stimulating hormone (FSH), in Estrogens, i.e. female sex hormones. Responsible for this transformation is a enzyme called Aromatase. Put simply, an enzyme is a substance that can carry out biochemical reactions.
Androgens, like all steroid hormones, also mediate their effect via receptors that are located inside the cell, to be more precise, in the cell nucleus. Also male sex hormones, such as testosterone or Dihydrotestosterone are present in the female organism and have biological effects. The main effects of male sex hormones in a woman's body include:
- stimulation of the development of armpit hair and pubic hair
- The development of the large labia (Labia majora) and des Clitoris (clitoris) and
- the increase in libido.
The level of male sex hormones also decreases in the postmenopause and also causes a further drop in the estrogen level, since fewer male sex hormones are available for conversion into estrogens. Male sex hormones can also be determined in the blood without any problems. When determining the testosterone level, it is also crucial in which phase of the cycle the blood was drawn. In the Follicular phase Values of <0.4 ng / ml are considered to be normal in the Ovulation phase a level of <0.5-0.6 ng / ml is normal and in the Luteal phase of <0.5 ng / ml. In the menopause testosterone levels of <0.8 ng / ml are encountered. In addition to the testosterone level, the level of two other androgens can also be measured. Also includes Androstenedionewhere a level of 1.0-4.4 ng / ml is to be regarded as physiological and Dehydroepiandrosterone sulfate (DHEAS), with a level normally between 0.3-4.3 μg / ml.
Estrogens
To the Estrogensthat belong to the class of female sex hormones are counted Oestrone (E1), Estradiol (E2) and Estriol (E3). These three estrogens differ in terms of their biological activity. Oestrone (E1) has about 30% and estriol (E3) only about 10% of the biological activity of estradiol. So is Estradiol (E2) that major estrogenic hormone. In addition to the formation of estrogens in the ovaries, the fatty tissue is also an essential place for estrogen production. And that is here Androstenedione, which belongs to the group of male sex hormones, by the enzyme Aromatase converted into an estrogen.
Estrogens are able to penetrate the cell itself through the cell membrane and thus their effect through two types of estrogen receptors, ER-alpha and ER-beta trigger. In addition, estrogens also have effects that are not mediated via the estrogen receptors; one speaks of so-called non-receptor-mediated effects. However, if an estrogen binds to an estrogen receptor inside the cell, the subsequent effect depends on the type of receptor. Put simply, the ER-alpha receptor type ensures proliferation, i.e. the growth and multiplication of cells, and the ER-beta receptor type has the opposite effect, i.e. it has antiproliferative effects.
It depends on the organ which type of the two estrogen receptors predominates. in the Breast tissue and in the uterus (uterus) both ER-alpha and ER-beta receptors can be found, whereas im brain and in Vascular system the estrogen receptor type ER-beta is found almost exclusively. Estrogens ensure the development and maturation of the female genital organs as well as the secondary sexual characteristics. So they condition the growth of the uterus, the Fallopian tubes, the vagina (vagina), of female shame (vulva), as well as the Mammary glands (Mammae). In addition, estrogens stimulate certain bone cells (Osteoblasts) and thus protect the female organism from you Bone loss. If the estrogen level falls, as is the case for example with increasing age in women, this also increases Risk of osteoporosisbecause the protective effects of estrogens are missing.
In addition, estrogens protect against premature hardening of the arteries (Atherosclerosis) in fertile age and ensure the typically high timbre of the female voice. With menopause, i.e. the last menstrual period, the production of the female sex hormone estrogen dries up due to an increasing functional weakness of the ovaries. Most of the symptoms complained of by women going through menopause can be explained by the rapidly falling levels of estrogen. At the center of the complaints are
- episodic hot flashes
- Sweats
- a headache
- forgetfulness and
- mental symptoms, how
- depressions
- Anxiety
- nervousness
- insomnia and
- Mood swings.
- Also Arrhythmia
- Joint- and muscle pain
- a Loss of libido and a Drop in performance
can occur. If the estrogens in the blood are determined, the following values for estradiol are regarded as normal:
- puberty 30 pg / ml
- Follicular phase up to 350 pg / ml
- Luteal phase 150 pg / ml or more
- Post menopause 15-20 pg / ml.
For estrogens with lower biological activity, such as estrone (E1) and estriol (E3), separate standard values apply.
progesterone
After ovulation, which is caused by a rapid increase in LH, the so-called "LH peak"Is triggered, is from Corpus luteum (Corpus luteum) progesterone produced. The corpus luteum arises from the ovulation Ovarian follicle.
In non-pregnant women, progesterone is used differently from estrogens produced exclusively in the ovaries.
In the pregnancy gets progesterone in much higher amounts from the placenta educated. Like estrogens, progesterone is able to penetrate the cells and mediate its effect via receptors located inside the cell. In the case of progesterone receptors, too, a distinction is made between the PR-A and PR-B receptor types. The following effects are mediated via the progesterone receptor PR-B:
- the maintenance of an already established pregnancy by preventing menstruation and relaxing the muscle layer of the uterus (Myometrium)
- the secretory transformation of the Uterine lining (Endometrium) in the second half of the woman's cycle
- one Increase in body temperaturer at about 0.5 ° C also in the second half of the cycle
- and finally, progesterone also inhibits the formation of estrogen receptors, so that progesterone limits the effect of estradiol.
Before the last menstrual bleeding (menopause) progesterone production decreases in the second half of the cycle (luteal phase) until it finally stops. The drop in progesterone levels makes it difficult to conceive (Conception ability), which means that the probability of a pregnancy becoming less and less due to the low progesterone level. Menstrual cycle disorders with irregular bleeding can also be explained by the reduced progesterone level. If this is to be determined in the blood, the blood must be taken in the second half of the cycle. The decreased progesterone level can, as well as the lack of estrogen, cause menopausal symptoms such as irritability or sleep disorders to care. The following values are considered normal for progesterone:
- Puberty 0-2 ng / ml
- Follicular phase <1 ng / ml
- Luteal phase> 12 ng / ml
- and in the postmenopause <1 ng / ml
In the first trimester of pregnancy, values between 10 and 50 ng / ml are found, in the second trimester the progesterone level is usually between 20 and 130 ng / ml and in the last trimester of pregnancy it rises to 130-260 ng / ml.
Inhibin
Inhibin belongs to the class of Proteohormones, that means it has a protein structure (protein = egg white). In women it is found in certain cells in the ovaries called Granulosa cells and with the man in the Testicles educated. Inhibin is responsible for inhibiting the release of FSH from the anterior lobe of the pituitary gland, but without affecting the release of the second gonadotropin, namely the LH. Inhibin, together with estradiol, is responsible for the peak of LH release. As already described, the LH peak again triggers the jump. In addition, the inhibin plays an important role in the Gender differentiation in the womb too. The secretion of the hormone inhibin also decreases with increasing age. The inhibin level is not determined in the blood because no normal values of inhibin are known.
Oxytocin

The hormone oxytocin is formed in the hypothalamus and, after its transport to the posterior lobe of the pituitary gland, is stored there and released when required. The release of oxytocin, which is sometimes also called "Cuddle hormone"Is called, is stimulated by any kind of comfortable skin contact. Mechanical stimuli on the nipple, such as when breastfeeding, on the vagina and on the uterus, cause oxytocin to be released. This is ascribed an important role in the birthing process. It causes the muscular layer of the uterus (myometrium) to contract, thereby triggering labor.
Because of this effect, it is also available in obstetrics as a drug to stimulate labor. Oxytocin is also responsible for the after-labor pains, which on the one hand are intended to prevent rebleeding after birth and cause the uterus to regress (involution). The emptying of the mammary gland vesicles, which leads to the release of milk during breastfeeding (milk ejection), is caused by oxytocin. In addition, oxytocin also has an impact on the interaction between mother and child and between sexual partners and also on further social behavior.
A good example of influencing mother-child interaction is the time after birth. Oxytocin ensures pleasant, pleasurable feelings here, which are intended to deepen the mother's emotional bond with her newborn. A large number of other physiological effects of the hormone oxytocin are already known or are still being investigated. The oxytocin level can also be measured in the blood. The normal values for oxytocin depend on whether the woman is currently breastfeeding a newborn. In non-pregnant and pregnant women, the normal value is 1-2 mIU / ml, while breastfeeding the oxytocin level is significantly higher at 5-15 mIU / ml.
More about this topic can be found: Oxytocin deficiency
Prolactin
Prolactin is made in cells of the anterior lobe of the pituitary gland. During pregnancy, prolactin prepares the female mammary gland for the approaching milk production. During this time, together with the estrogens and the progesterone, it stimulates the differentiation of the mammary gland tissue. However, the high concentrations of estrogens and progesterone that are present during pregnancy prevent milk from being bound too early. After birth there is a drop in estrogen and progesterone concentrations, so that prolactin, together with other factors, is responsible for the formation of the Breast milk can trigger.
Normal values for prolactin are between 100 and 600 µU / ml. Values that require control are between 600 and 1000 µU / ml, values> 1000 µU / ml are clearly too high. It should be noted that various drugs can increase the prolactin level. This includes, for example Metoclopramidewhat at nausea and Vomit is used. When taking metoclopramide, prolactin levels of> 2000 µU / ml can occur. It is also important that the blood for determining the prolactin values may be drawn at the earliest 1-2 hours after getting up, otherwise the prolactin values may become too high due to the increased secretion during the night.