Coronary artery disease therapy
Forms of therapy
Causal therapeutic approaches serve primary (measures to prevent CHD) and secondary prevention (measures to prevent the progression and deterioration of CHD).
This is fundamental for both forms of prevention Eliminating risk factorsthat can be influenced and favor the development of coronary heart disease (CHD), i.e.:
- Body weight reduction
- Nicotine abstinence (quitting smoking)
- optimal control of diabetes mellitus / increased blood lipids (especially hypercholesterolemia) / high blood pressure (hypertension)
- physical training (especially endurance training) and
- Diet change.
Angina pectoris
The symptomatic therapy of an acute, stable angina pectoris attack consists in the administration of a short-acting Nitro preparationssuch as glycerol trinitrate as a spray or bite capsule. This drug causes better blood flow to the inner layer of the heart and lowers the need for oxygen Heart muscle (Myocardium).
Medication
Long-term drug therapy, which serves as secondary prevention, is intended to lead to better heart muscle supply and closure of the Coronary arteries (Coronaries) prevent blood clots (thrombi). It consists of the following drug groups:
- Nitrates are not only used for acute or emergency therapy, but also for long-term therapy. Long-acting nitrates such as isosorbide mononitrate or isosorbide dinitrate and molsidomine are used here, which widen the coronary arteries and thus improve the oxygen supply to the heart.
- The heart rate, the number of heartbeats per minute and the blood pressure are measured with the help of Beta-blockers decreased, which leads to the reduced oxygen demand of the heart under stress. The mortality (lethality) decreases in acute myocardial infarction patients as well as patients with previous myocardial infarction through the use of beta blockers. The use of this group of drugs should be considered asthma-Patients and Diabetics done carefully, as bronchial system narrowing can occur and the signs of a Hypoglycaemia may be masked by the effects of the medication.
- If the administration of beta receptor blockers is not possible due to contraindications that the patient has Calcium channel blockers be administered as reserve medication, whereby care must be taken to use long-acting calcium channel blockers, as the clinical picture of the patient would be negatively influenced by short-acting medication.
- Clopidogrel or aspirin become to Anticoagulant inserted so that vasoconstricting Thrombosis (more venous Vascular occlusion) or Embolisms (arterial Vascular occlusion) can be avoided. It is necessary to monitor this effect as well as potential side effects of the medication through regular checks.
- Cholesterol synthesis inhibitors (e.g. Simvastatin) serve to lower the cholesterol level in the blood, which is a risk factor for the development of CHD.
- Of course, the circulatory disorder can also be treated with homeopathic medicines. Please read on: Homeopathy for circulatory disorders.
- Coronary heart disease can also be treated with homeopathic remedies. Please read on: Homeopathy for coronary heart disease.
Invasive Therapy
Invasive therapeutic options for revascularization in coronary heart disease (CHD) are catheter interventions with vasodilation or bypass surgery.
Both procedures aim to restore the patency of the narrowed or blocked coronary artery (Revascularization).
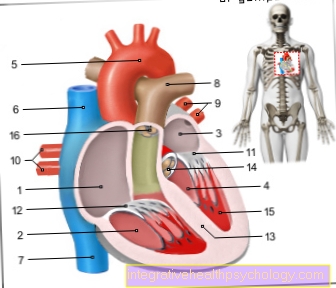
Cardiac catheter
Expansion of the coronary arteries as part of a cardiac catheter examination
The percutaneous transluminal coronary angioplasty (PTCA) can be used as a standard method, i.e. can be used as the sole balloon expansion of the vessel (balloon dilatation), or in combination with a stent insert to keep the vessel open mechanically. This form of therapy is used when there is a one- to three-vessel disease with significant vascular narrowing of over 70% and the patient is more stable or unstable Angina pectoris suffers. The objective of this procedure is that Coronary blood flow to ensure again.
A successful vasodilation with subsequent freedom from symptoms occurs in approx. 90% of the cases. Approx. After 6 months, 30% of the patients show a renewed narrowing of the coronary artery with anginal symptoms (chest cage); If a stent was implanted during the PTCA, this value drops to approx. 15-20%. With stent implantation, a grid-like tube is inserted into the constriction of the coronary artery after the expansion in order to keep it open permanently.
Most patients with residual narrowing of the vessel can receive another PTCA to reopen the vessel without increased risk.
The procedure is as follows possible complications:
The manipulation of the vessels using catheter wire can lead to a Dissectioni.e. an injury to the vessel wall with subsequent bleeding between the layers of the vessel wall. If this occurs, a stent is used to close the detachment of the layers of the vessel wall. If this is unsuccessful, an emergency bypass operation must be performed.
The PTCA procedure has a mortality rate of 1%.
If the main trunk of the left coronary artery is narrowed (stenosis), no catheter intervention is performed, but a bypass operation.
Bypass surgery
The bypass operation is the recognized surgical procedure for reopening closed coronary arteries and is also known in technical terms as a coronary artery bypass graft (CABG).
The bypass operation is performed if the main trunk constriction of the left coronary artery is present, a symptomatic three-vessel disease with various constrictions is present, or a two-vessel disease with narrowing close to the trunk causes symptoms. Narrows that are close to the vascular trunk are unfavorable for the blood flow and carry the risk of making one (in the case of the right coronary artery) or two important (in the case of the left coronary artery) supplying vessels impermeable.
Furthermore, the indication for surgery is made if a Angina pectoris could not be successfully treated by drug therapy or catheter intervention.
The Requirements for an operation are:
- the presence of a significant narrowing of over 50% of the vessel cross-section
- Coronaries, which are continuous in the distal (in the narrow downstream) part
- a functioning heart muscle behind the vascular narrowing
- a coronary artery at least 2mm in diameter so that a bypass vessel can be connected to it
During the operation, the chest is opened and the heart is applied Life-support-machine shut down so that it no longer pumps itself, but the circulatory function is ensured by the extracorporeal (outside the body) circulation via the machine.
The coronary artery stenosis is bridged by means of a bypass vessel so that the blood flow can bypass the constriction and the downstream heart muscle tissue can be supplied again.
More than 80% of the patients are symptom-free after the operation.
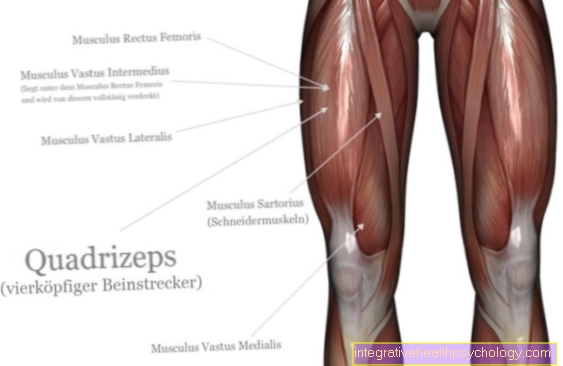
The right or left thoracic artery (internal thoracic artery) can be used as a bridging vessel, as can the radial artery of the hand or a femoral vein (great saphenous vein). The two vessels mentioned last are dissected intraoperatively (during the operation) from their original anatomical position and used as an intermediate piece (interposal) to bridge the coronary arteries.
The radial artery (radial artery) can only be used as a bypass if the ulnar artery (ulnar artery) alone ensures the supply of the hand.
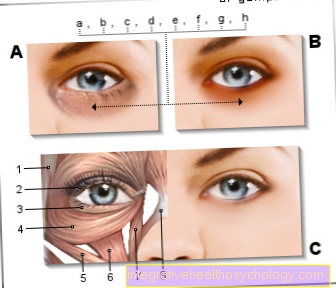
Of the Allen test is used to check the blood flow situation in the hand: In the run-up to the operation, the examiner squeezes the vessels on the right and left side of the wrist where pulses can be felt. If the hand is discolored whitish after a few seconds, it relieves the ulnar side of the wrist, the side of the wrist facing the little finger and continues to exert pressure on the radial artery. If the hand turns rosy again, the blood flow to the hand through the artery on the elbow side is ensured and the radial artery can be used for bypass surgery.
Was a venous bypass, i.e. If the coronary artery has been bridged with the help of the femoral vein, the probability of occlusion in the first 5 years after the operation is 20-30%. The arterial bypass closes again in less than 10% after 10 years.
The risk of the operation carries a mortality of 1%, suffering a heart attack during the operation in 5 - 10% of the cases.
Follow-up treatment of the operated patients is carried out with platelet aggregation inhibitors (aspirin, Clopidogrel) that inhibit blood clotting.







.jpg)