Diagnosis of a heart attack
Diagnosis of myocardial infarction
The pillars of heart attack diagnosis consist in the survey:
- the angina pectoris symptoms (pressure and tightness in the chest) of the patient
- in typical EKG changes and
- the detection of myocardial infarction markers in the blood (proteins troponin I and T).
This three-part diagnostic scheme is used to confirm an existing myocardial infarction.
The World Health Organization (WHO) defines the presence of a heart attack in the event that the patient has at least two of the three criteria mentioned above.

What diagnostic measures are taken in the event of a heart attack?
Blood lipid levels, heart disease (coronary artery disease, atherosclerosis), previous heart attacks, age, heart disease in the family
-
Medical history (asking the patient about symptoms)
-
Pain, stinging in the region of the heart
-
Radiating pain in the stomach, upper abdomen, left arm, back, between the shoulder blades, etc.
-
Sensation of pressure, tightness in the chest
-
Nausea, vomiting
-
shortness of breath
-
Loss of performance, low resilience, fatigue
-
Dizziness, fainting spells
-
Heavy sweating
-
Risk profile:
-
- EKG
- blood values
- LDH
- Troponin T
- CK-MB
- Myoglobin
Read more about: Troponin test
EKG
Cardiac guidelines differ slightly from the WHO definition. You assume a heart attack if there are typical changes in the EKG, a so-called
ST segment elevations, are present and the patient has symptoms of insufficient oxygen supply Heart muscle cells (Myocardial ischemia) in the form of chest pain.
Once these two clinical signs have been identified, the patient can promptly and without delay Revascularization measure (Re-opening closed or narrowed Coronary arteries) to correct the oxygen deficiency (ischemia) of the heart.
The result of the Blood test In this case there is no need to wait for the heart attack marker to legitimize revascularization.
At the beginning of the diagnosis, the patient's medical history (anamnesis) is taken, with a focus on the acute symptoms, and the patient is physically examined.
In the acute phase of the heart attack, most of those affected complain very much Strength Chest pain, they are cold sweaty, frightened and restless.
The echocardiogram (EKG) is used as a second diagnostic step to determine a heart attack. The EKG makes the electrical conduction processes of the heart muscle action visible, which are the same and unmistakable in every healthy person. By changing the typical, healthy EKG image, different, pathological conditions of the heart can be recognized, including a heart attack. With its help, the extent of the heart attack, its location and the age of the heart attack can be determined. It results in 80% of heart attack cases Changes in the course of the ECG curve. One speaks of one ST elevation (S and T are typical points of an EKG cardiac lead), which is caused by the death of the heart muscle cells.
Inconspicuous EKG and yet heart attack!
The ECG result can be negative (normal) within the first 24 hours after the onset of the infarction, which is why the determination of myocardial infarction markers (laboratory values) in the blood can confirm the suspected diagnosis even if the ECG is normal.
Diagnosing a silent heart attack
As with the diagnosis of any disease is also with the silent heart attack first the anamnese (i.e. questioning the patient) pointing the way for recognizing the infarct. The symptoms felt by the patient play a major role here dizziness, nausea, Sweats and Fainting spells a role. Characteristic for a silent heart attack that is Absence of chest pain.
At a Suspicion on a silent heart attack should subsequently immediately a EKG to be written. Electrodes are attached to various places on the chest wall (sometimes arms and legs) so that the electrical currents in the heart can be measured. In contrast to the normal case there is special characteristicswhich the EKG only shows in the event of a heart attack.
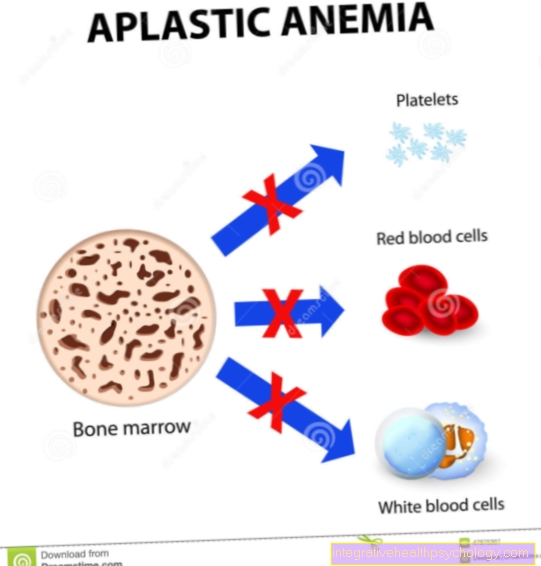
Furthermore you can Blood tests be consulted. Above all, one plays a role Increase in the troponin T value a major role. There are also other blood values that can also indicate a silent heart attack. Myoglobin and CK-MB play an important role in this. The Myoglobin is a protein found in muscles.
In the case of a silent heart attack heart muscle cells die. This releases the substances contained in the cells into the blood. CK-MB (Creatine kinase of the type MB) especially in the heart muscle before and when its cells die, it also gets into the blood poured out.
Laboratory values
The determination of troponin in the blood is therefore the third pillar of heart attack diagnosis. Troponin T and I are proteins in the heart muscle cells that play an important role in the contraction of the heart muscle cells. If heart muscle cells die in the course of the infarct, they end up in the blood, where their concentration does not increase until three hours after the start of the infarction at the earliest. The maximum concentration in the blood is reached after 20 hours and one to two weeks after the infarction, the troponin values have normalized again.
The markers are used to make the diagnosis, especially for patients who suffer from chest pain but do not show any changes in the ECG:
If the amount of troponins in the blood is above a certain value, there is a very high probability of a myocardial infarction with cell death and an intervention to reopen the blood vessels is indicated. If the troponin determination is negative, i.e. if the marker values are below a certain limit, a heart attack can almost be ruled out and the diagnosis "unstable angina pectoris" made.
The enzyme CK-MB (creatine kinase of the heart muscle) is also determined as part of heart attack diagnostics. In an extensive heart attack, many muscle cells die, so that a large number of this enzyme is released into the bloodstream. Together with the clinical signs of chest pain, the CK-MB concentration in the blood sample can provide a clear diagnostic indication of a heart attack.
The concentration in the blood increases approx. 4-8 hours after the onset of the infarction, which means that the CK-MB concentration is a slow marker of myocardial infarction, in contrast to the troponins. The CK-MB determination serves more to confirm the diagnosis than to collect it.
As rapid diagnosis and rapid initiation of therapy should be achieved in order to protect additional myocardial tissue from destruction, troponins are the gold standard (currently the best and most efficient method for determining the disease) in enzyme diagnostics (blood tests) in the event of a suspected heart attack.
Troponin
Troponin is a special enzyme in the heart muscle. When heart muscle cells die or are destroyed, they release their ingredients. Typically, if a heart attack is suspected, the troponin T in the blood is determined. It can be measured in higher concentrations especially 3-8 hours after a heart attack. In addition, it is still detectable in the blood with an increased level for up to two weeks after the infarction.
However, troponin T can also be incorrectly elevated (if it has nothing to do with a heart attack). This is the case when the kidneys are no longer fully functional because too little troponin is excreted and it is therefore present in higher amounts in the blood. Even when the skeletal muscles are exposed to extreme loads, as is the case, for example, with marathon runners, the troponin T value increases.
Read more about this under our topics:
- Troponin test
- Troponin
Echocardiography
The Echocardiography, an ultrasound examination of the heart (heart echo), is used to examine the shape and shape of the heart as well as functional diagnostics (wall movement disorders of the heart due to tissue destruction can be detected).
It is a non-invasive examination and can be carried out quickly.
The echo examination makes it possible to assess the movement of the heart wall, which is of great diagnostic relevance, since disturbances of the movement of the heart wall indicate an infarct zone or scar during the contraction of the heart. In recent myocardial infarction, wall movement disorders occur before the heart muscle-specific enzymes rise. In the absence of such movement disorders, a heart attack can be ruled out with a 95% probability.
In addition, echocardiography enables the size of the heart to be recorded and any cardiac dilation (dilatation) that may have occurred after an infarction, the pumping capacity of the heart and the function of the heart valves.
Infarcts mostly affect the left ventricle and their localization can be recognized by the various supply areas of the coronary vessels. However, due to the inter-individual anatomical differences in the course of the coronary arteries and the lack of knowledge about the type of cardiac supply (vascular supply to nourish the myocardial cells), no precise statement can be made about which vessel is occluded. This requires an angiographic examination of the coronary arteries using a catheter and administration of contrast medium (Cardiac catheter).
General information about ultrasound can be found under our topic: Ultrasonic
Cardiac catheter
The Left heart catheter examination (Cardiac catheter) is the gold standard of imaging methods in heart attack diagnostics, as it enables the closed coronary vessels to be identified precisely. This procedure is also called Percutaneous Transluminal Coronary Angioplasty (PTCA):
After an arterial vessel has been punctured, a catheter (a type of thin tube) is advanced to the left side of the heart. One looks for the outlets of the coronary arteries (coronaries) from the main artery (aorta) and applies an X-ray contrast medium via the catheter. This is used to represent the coronaries in the X-ray image (Coronary angiography). The made X-rays provide the exact localization of the cause of the heart attack in the event of a narrowing or obstruction of the coronary arteries and make targeted therapy possible.
In the early phase of acute coronary syndrome, the diagnostic procedure can be performed with a revascularizing surgery be linked:
A balloon is inserted into the vascular system via the catheter, which is pushed through the left heart to the coronary arteries. This is stretched at the narrowed vascular site (Balloon dilatation) and the vessel expands and thus made it passable again. Often one is used Stent (tubular grid) to keep the vessel permanently open.
Another measure to visualize the infarct is a magnetic resonance imaging examination (MRI) from heartwhich makes it possible to localize an infarct at an early stage.