hepatitis
Synonyms in the broadest sense
Liver inflammation, liver parenchymal inflammation, viral hepatitis, autoimmune hepatitis, toxic hepatitis
definition
The doctor understands hepatitis to be inflammation of the liver, which can be caused by a variety of factors that damage the liver, such as viruses, poisons (toxins), autoimmune processes, drugs and physical causes.
The various types of hepatitis cause liver cell destruction and the migration of inflammatory cells into the liver.

Characteristic symptoms can include an enlarged liver (see also: swollen liver) with pain in the capsule of the liver and the development of jaundice (icterus). The severity of the symptoms varies from mild, almost symptom-free disease states to fulminant liver failure.
Read more on this topic at: chronic disease
Classification of hepatitis
Hepatitis can be divided in several ways:
- First, you can divide them up according to the course:
Acute hepatitis shows itself in a short course (<6 months).
Chronic hepatitis shows itself over a long course (> 6 months) and by definition shows connective tissue (fibrous) scarring of the liver tissue in the fine tissue examination (histology).
- Classification according to the cause (etiology, pathogenesis):
Infectious hepatitis: viral (hepatitis A, B, C etc.), bacterial, parasitic
Toxic hepatitis: alcohol-toxic, drug-toxic, drug-induced hepatitis and hepatitis in the case of poisoning
Autoimmune hepatitis: AIH (autoimmune hepatitis), PSC (primary sclerosing cholangitis), PBC (primary cheap cirrhosis)
Hereditary, congenital hepatitis: hemochromatosis, Wilson's disease, α1-trypsin deficiency, granulomatous inflammation (sarcoid)
Physical hepatitis: hepatitis after radiation, hepatitis after liver injury
Extrahepatic diseases: congestive hepatitis in heart failure, hepatitis in fatty liver (steatohepatitis), biliary tract inflammation (cholangitis)
- Classification according to the tissue (histological) criteria:
In acute hepatitis there is an increase in Kupffer cells,
Single cell necrosis, bloated hepatocytes and infiltration of inflammatory cells are present.
In chronic hepatitis, fibrous scarring and a loss of the typical liver structure can be seen.
In fulminant hepatitis, so-called bridging (confluent) Necrosis (dead liver tissue).
The hepatitis virus
Virology, the science of viruses, differentiates between several pathogens that cause hepatitis. These are named after the alphabet from A to E and have different properties:
- Hepatitis A (HAV): Faecal-oral transmission through contaminated food / water, mainly in developing countries, Mediterranean regions and the tropics; no chronification
- Hepaititis B (HBV): transmission through sexual intercourse, needlestick injuries, during childbirth from mother to newborn; chronic course possible in 5% of infections
- Hepatitis C (HCV): route of transmission unknown in 40% of cases, transmission through needlestick injuries, split injection needles in drug addicts, during childbirth, during sexual intercourse; Chronification in 50-85% of cases; Course of infection often without symptoms
- Hepatitis D (HDV): transmission through sexual intercourse, needlestick injury, during childbirth; Infection only possible in connection with a hepatitis B infection
- Hepatitis E (HEV): Faecal-oral transmission, through contaminated food / water; Serious courses can occur much more frequently in pregnant women and can be life-threatening for mother and child; Chronification possible after organ transplantation
How long is the incubation period for the hepatitis viruses?
The incubation period is defined as the time between the penetration of a pathogen into the body and the onset of a corresponding disease with its first symptoms. The incubation period of a hepatitis A infection is between 14 and 50 days, depending on the source. The incubation period of hepatitis E is comparable and is 14 to 70 days. As already mentioned above, these two liver inflammations show a similar transmission route and also the same viral properties, which ultimately results in the comparable incubation time. Hepatitis B can show an incubation period of 1 to 6 months, as can the associated hepatitis D. Hepatitis C has an incubation period of approximately 8 weeks.
Hepatitis A
Hepatitis A is an inflammation of the liver caused by the hepatitis A virus. It is the most common form of "acute hepatitis" - acute means that it heals after a few weeks, in a few cases after a few months, and does not become chronic in all those affected.
Most holidaymakers in southern countries with inadequate hygienic conditions develop hepatitis A after ingesting the virus through contaminated water or contaminated food. Before planning a trip, vacationers should therefore find out from a family doctor whether a hepatitis A vaccination is recommended for the destination country.
Read more on the topic: Causes of hepatitis A.
Typically, hepatitis A begins during or shortly after the stay abroad with symptoms reminiscent of flu and / or gastrointestinal complaints. Symptoms of hepatitis A include fatigue, aching limbs, often combined with loss of appetite, nausea, or pain in the liver. These symptoms usually last for about 1 week and can be mistakenly misinterpreted by the doctor and the patient as a simple cold, flu or gastrointestinal infection.
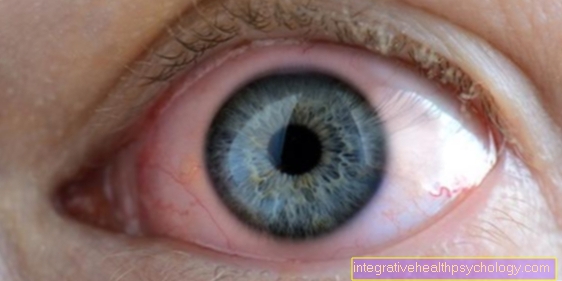
In the course of the disease, the typical yellowing of the eyes or skin can occur, whereby the discoloration of the eyes is usually noticeable first.
In addition, the urine often turns dark and the skin becomes itchy.
For many people, especially children, hepatitis A does not cause any symptoms and can therefore go completely unnoticed. Hepatitis A is only very rarely severe. Usually it is harmless and heals without consequences after a short period of illness. It leaves you with a lifetime of immunity.
Read more on the topic: Hepatitis A
Hepatitis B.
Hepatitis B is caused by the hepatitis B virus. It manifests itself mainly as symptoms caused by damage to the liver, but it can also affect other organs such as the skin or joints.
Hepatitis B is usually transmitted through sexual contact in countries with high levels of population contamination, but it can also be transmitted through direct uptake of the virus into the blood. Drug addicts, in particular, are at risk from using dirty needles. Transmission from mother to child before or during birth is also possible.
Read more on the topic Hepatitis B causes and transmission of hepatitis B
The virus is most widespread in Central Africa and China. Hepatitis B is the most common hepatitis in the world. After infection with the virus, the disease usually breaks out within a few weeks - but in exceptional cases it can take six months before the first symptoms appear.
In 2/3 of those infected, however, the hepatitis B virus does not cause any symptoms and goes completely unnoticed. The virus is eliminated from the body and can no longer trigger the disease. If symptoms of hepatitis B occur, the disease usually begins like any hepatitis caused by viruses with flu-like symptoms such as fatigue and tiredness or symptoms that resemble a gastrointestinal infection, such as nausea, diarrhea and loss of appetite. As is typical for many liver diseases, the skin and eyes may then turn yellow. Often this yellow coloration is accompanied by itching all over the skin and darkening of the urine.
In a small proportion of people who show symptoms, the immune system is unable to clear the virus from the body. This is known as virus persistence. Virus persistence can go unnoticed and without symptoms. Those affected are outwardly healthy. In about 1/3 of the cases, however, it triggers and sustains a permanent inflammation of the liver that varies from person to person. The latter is known as chronic hepatitis B. This leads to cirrhosis of the liver after years. Liver tissue is destroyed, replaced by connective tissue and the liver loses its function. On average, after 10 years, cirrhosis of the liver can be detected in every fifth patient. In addition, liver cancer can develop in the diseased liver after years.
A causal therapy that attacks the virus is usually only used if the virus causes chronic hepatitis B. On the one hand, drugs are used that activate the own immune system, on the other hand, drugs are used that suppress and fight the virus itself. They are usually administered for at least six months, and in some patients longer. In most cases, chronic hepatitis cannot be completely cured with the drugs available today. However, the virus can be suppressed so strongly that secondary diseases - liver cirrhosis and liver cancer - can be prevented. A hepatitis B vaccination is recommended for every child in Germany these days. When responding, it protects very reliably against infection.
Read more on the topic Hepatitis B therapy
Hepatitis C.
Hepatitis C is the inflammation of the liver after transmission and infection with the hepatitis C virus. In western countries, the virus mostly enters the body through “needle-sharing”. This is the repeated use and sharing of a needle to inject drugs into a vein. The virus is passed on sexually via the mucous membranes much less frequently. Transmission from mother to child before or during birth also plays a role. The virus is most widespread in parts of Africa. In Europe, up to 2% of all people are carriers of the hepatitis C virus.
Read more on the topic Causes of hepatitis C.
Hepatitis C is insidious because it does not cause any direct symptoms such as tiredness, liver pain or yellowing of the eyes or skin in the majority of those affected. Those affected often do not notice the disease for a long time. However, in those patients who do not initially develop symptoms, 80% of the time the virus remains in the body, causing chronic infection of the liver. This is known as "chronic hepatitis C" and can lead to liver cirrhosis after years without treatment. In some patients, this leads to complete liver failure, which currently can only be treated with liver transplantation. Another danger of the disease is the frequent occurrence of liver cancer. Sufferers should therefore be examined regularly with the help of ultrasound of the liver and a blood sample in order to find liver cancer in its early stages and thus be able to treat it much better.
In some cases, so-called autoimmune diseases occur with hepatitis C. Under the influence of the virus, the immune system reacts to components of its own cells and can cause very different symptoms. Frequent examples are inflammation of the kidneys or the thyroid gland and destruction of the blood cells resulting in anemia.
The therapy for hepatitis C has changed dramatically in recent years. While it was rarely curable 20 years ago, it is now possible to completely cure the disease in almost everyone affected. In addition, the drugs used today are much better tolerated.
What drugs are used and how long they are given depends on the subtype of the virus. Treatment can usually be completed within 6 months.
In contrast to vaccinations for hepatitis A and B, a vaccination against hepatitis C is unfortunately not yet available. However, various means are being tested, which is why this could change in the next few years.
Read more on the topic: Hepatitis C, drugs for hepatitis C.
Hepatitis D
An infection with the hepatitis D virus can only occur simultaneously with a hepatitis B infection (simultaneous infection) or in people who already carry the hepatitis B virus. The hepatitis D virus cannot reproduce without parts of the hepatitis B virus. This means that a successful vaccination against hepatitis B also protects against hepatitis D. Similar to the hepatitis C virus, the virus is usually transmitted via venous injections of drugs with dirty needles.
If a person becomes infected with both viruses at the same time, the resulting hepatitis is often severe. Those affected feel very weak, the liver is severely inflamed.
Often the eyes and skin become yellow.
In 95% of the cases, however, the disease is only brief and then heals completely. If people with hepatitis B are also infected with the hepatitis D virus, the liver is often damaged more quickly. Without the right therapy, this can lead to cirrhosis of the liver after a few years.
Read more about this under: Hepatitis D
Hepatitis E.
Like hepatitis A, hepatitis E is an inflammation of the liver that lasts a few weeks. It is transmitted by the hepatitis E virus. The pathogens are mostly ingested by tourists in Asia, the Middle East or Central and North Africa through contaminated drinking water. In the countries mentioned, however, the virus can also enter the body after contact with animals such as pigs and sheep or through the consumption of raw meat from these animals.
Like hepatitis A, the disease typically begins with symptoms such as flu-like and / or gastrointestinal complaints. Followed by severe fatigue and yellowing of the eyes and skin. Usually it heals without consequences.
Pregnant women who develop hepatitis E are a special case. In up to 20% of cases, the disease is severe and can be life-threatening despite good treatment in hospital.
Therefore, pregnant vacationers are advised to consult a doctor as soon as possible if the symptoms mentioned above.
Read more about this under:
- Hepatitis E.
and - Symptoms of hepatitis E
What other forms of hepatitis are there besides A, B, C, D, E?
The causes of hepatitis discussed so far in this article are not the only triggers. In addition to the directly infectious hepatitis, triggered by hepatitis viruses A, B, C, D and E, so-called accompanying hepatitis (accompanying liver inflammation) can also occur .
These can then also be caused by viruses, but also by parasites or bacteria. Parasitic pathogens that can cause hepatitis are, for example, the malaria pathogens, plasmodia. Salmonella, for example, could be mentioned as a bacterial pathogen accompanying hepatitis.
In addition to these causes, there are other forms of hepatitis, such as toxic hepatitis after long-term alcohol abuse, ingestion of poison such as snake venom or after consuming poisonous mushrooms. Even drugs in toxic overdoses can lead to hepatitis, paracetamol as an example.
In addition to these forms of hepatitis, the autoimmune hepatitis should also be mentioned, which lead to inflammation of the liver due to the body's own processes. The body develops autoimmune antibodies that are directed against the liver cells. However, this autoimmune hepatitis is considered a relatively rare disease.
Alcohol hepatitis

As mentioned above, toxic causes can also lead to hepatitis. In addition to toxic substances in mushrooms, snake venom or drugs in overdose, hepatitis can also develop due to alcohol. This leads to the death of liver tissue and thus to the loss of function of the liver. In the end, if you continue to consume alcohol, what is known as fatty liver develops, and ultimately liver cirrhosis, which can lead to liver failure. In western countries in particular, excessive alcohol consumption is very often responsible for cirrhosis of the liver.
Symptoms of hepatitis
The symptoms of hepatitis are very variable in their severity. They range from complete freedom from symptoms, in which the diagnosis is made solely via abnormal liver blood tests, to fulminant liver failure.
The symptoms of hepatitis can be described as follows:
In the beginning, the patient complains of general malaise such as:
- fatigue
- Exhaustion
- a headache
- Muscle and joint discomfort.
- Loss of appetite
- nausea
- Vomiting and
- Weight loss.
A feeling of pressure in the right upper abdomen can indicate an enlarged liver. If the cause of hepatitis is infectious, a fever can also occur.
Read more on the topic: Enlarged liver
Jaundice (jaundice) and its accompanying symptoms can later develop. The billirubin (bile pigment) can no longer be excreted into the bile ducts by the affected liver cells (hepatocytes).
A typical symptom complex of jaundice develops:
Yellowing of the skin and the color of the eyes (dermis, sclera) are the most obvious symptoms of jaundice. Tormenting itching, caused by deposited bile salts in the skin, is particularly unpleasant for the patient. There is also a clay-like discoloration of the stool due to the lack of bile pigment in the stool and a dark coloration of the urine, as the kidneys take over the excretion of the bile pigments. The lack of bile acids in the small intestine makes it harder to digest fats, which can lead to intolerance to high-fat meals and fatty stools (steatorrhea).
Rash as a symptom
Liver diseases typically show changes in the skin, which are then referred to by name as liver skin signs. This includes jaundice (jaundice) in the first place. The bile pigment bilirubin is deposited under the skin and on the one hand causes yellowing of the skin and also a certain itchiness. Further liver skin signs only appear after long-term damage to the liver, such as in the context of liver cirrhosis and are expressed in certain vascular drawings in the abdominal area, lacquer lips and lacquer tongue, cloudy or whitish discoloration of the fingernails and toenails and a parchment-like change in the skin.
What can be signs of hepatitis?
Basically, the various inflammations of the liver do not differ significantly in their initial symptoms. This is because unspecific signs such as tiredness and exhaustion, abdominal pain, nausea and vomiting as well as flu-like signs with a slight fever often appear. The suspicion of hepatitis is then often confirmed after the skin has turned yellow, known as jaundice. This yellowing often begins in the area of the eyes, when the sclera (leather skin of the eye) changes color.
The first signs of certain hepatitis viruses may also be absent. With hepatitis B, for example, symptoms are absent in two thirds of cases and only one third has an acute course with jaundice. Hepatitis A also usually manifests itself in children without symptoms. The older the affected person is, the more serious the course of a hepatitis A infection will occur, especially if another hepatitis infection or another liver disease is already present. The main signs of hepatitis C are jaundice.
How do I get hepatitis?
The possibility of infection is more dangerous for certain groups of people than for others. As already mentioned, there are different ways of transmission of the individual viral diseases. For example, hepatitis A and hepatitis E can mainly be transmitted through contaminated food such as food or water. This is most likely to happen in tropical or developing countries, but sewer workers can also become infected. In this context, faecal-oral means that poor hand hygiene can lead to infection, or if food is not properly cleaned or water is not boiled.
Other hepatitis viruses, such as the hepatitis B or C virus, can be transmitted via needlestick injuries in the healthcare sector or from drug addicts who share syringes. Even during natural vaginal delivery, there is a high probability that the virus will be transmitted from mother to child, which in most cases means that the child becomes chronic.
In the past, it was also possible, for example, to get hepatitis C through blood products. Before 1992, blood donations were not tested for this virus in series, so it was possible to develop hepatitis C through a blood transfusion. Nowadays there is still a risk of transmission, which at 1: 1,000,000 is very, very low.
Can You Get Hepatitis From Kissing?
The routes of transmission of the hepatitis viruses already described can essentially be summarized in a few. Once the transmission through food and water, then the needlestick injury, transmission through sexual intercourse and finally the transmission from mother to child at birth. The virus concentration (also referred to as the viral load) plays a role in all infection routes. This is directly greater during sexual intercourse or with needle stick injuries than when kissing. A certain viral load can also be detected in the saliva. Infection through kissing is therefore possible in principle, but is rated as very low.
Diagnosis of hepatitis

In the patient interview (anamnesis), pioneering symptoms and causes of hepatitis can often already be ascertained. enclose. Targeted questions about alcohol and drug consumption and vaccinations against hepatitis A and hepatitis B can help narrow down the possible causes of hepatitis.
Questions about medication intake close up (drug-toxic hepatitis?), Stays abroad (infectious hepatitis?) etc.
Physical examination often reveals painful pressure in the right upper abdomen and palpable enlargement of the liver in acute hepatitis.
Blood count / liver values
Changes in the blood count are almost always present in hepatitis. The liver enzymes (transaminases or "liver values") GOT (glutamate oxaloacetate transferase or ASAT = aspartate aminotransferase) and GPT (glutamate pyruvate transferase or ALAT = alanine aminotransferase) are proteins produced by the liver that are in a liver cell are located in different cell structures.
For more information, please also read our page Liver values.
In the event of liver cell destruction, e.g. in the course of inflammation, they are released from the liver cells and are therefore detectable in increased concentrations in the blood.
Depending on the constellation of the enzymes, the extent of the liver cell damage can be traced. In the case of slight liver cell damage, the enzymes GPT and LDH (lactate dehydrogenase) initially increase because they can quickly diffuse through the membrane of the broken cell. In the event of severe cell death, the enzymes GOT and GLDH (glutamate dehydrogenase), which are located in the mitochondria (cell organelles) of the cells, are also increasingly released.
Bilirubin, gamma-glutamyl transferase (γ-GT) and alkaline phosphatase (AP) can also be increased in the event of biliary congestion.
In viral hepatitis, antibodies against virus components or the DNA of the virus can be detected in the blood.
You might also be interested in this topic: Ferritin
Sonography / ultrasound
During an ultrasound examination, the abdominal organs are visualized with the help of ultrasound waves. The transducer emits ultrasound waves that are absorbed or reflected by the various tissues it encounters. The transducer receives the reflected waves, which are converted into electrical impulses and displayed on a screen in different shades of gray.
In acute hepatitis, the liver is enlarged and a little less hypoechoic (i.e. darker) due to a build-up of fluid in the liver (edema). Chronic hepatitis often shows a liver-like structure that appears more echogenic and offers an almost smooth transition to the signs of cirrhosis of the liver.
Read more on the topic: Ultrasound of the abdomen
Liver puncture / liver biopsy
In most cases, the liver puncture allows a reliable diagnosis through the histological examination of the tissue under the microscope. There are several ways in which liver tissue can be obtained:
The simplest type is a liver blind puncture, in which, as the name suggests, the liver is punctured “blindly” with a hollow needle without the support of an imaging method. A tissue cylinder is removed, which is examined by the pathologist.
The targeted puncture of the liver is carried out with the help of an imaging procedure, such as sonography or computed tomography. The needle is pushed into the liver, so to speak, under visual control, in order to avoid complications such as bleeding as much as possible. The targeted puncture of the liver must be carried out especially in diseases that only affect part of the liver, such as tumors (liver cancer), cysts and other unclear liver nodules (e.g. metastases).
Finally, when diagnosing hepatitis, the liver can also be biopsied during a laparoscopy. During this procedure, which is performed under general anesthesia, the liver is examined in a minimally invasive manner. The surface of the liver can be inspected through small incisions in the abdominal skin by introducing a rod camera and a piece of tissue can be removed from the organ.
Read more on the subject at: Liver biopsy
therapy
The therapy of the individual hepatitis is very different (see subchapter on hepatitis).
The most important thing in therapy is to eliminate the cause responsible for the hepatitis. In the case of alcoholic hepatitis, this means absolute abstinence from alcohol. The toxin must also be avoided in the case of drugs and other toxic hepatitis.
Antiviral therapy is possible for some viral hepatitis.
Autoimmune hepatitis is treated with immunosuppressants (drugs that suppress the immune system).
In cases of fulminant liver failure, congenital hepatitis and chronic hepatitis that has progressed to liver cirrhosis, liver transplantation is often the only option as the last option.
Read more on the topic: Medicines for hepatitis C.
Which hepatitis is curable?
The therapy options are constantly evolving and in recent years have achieved a very positive prognosis for sick people, especially those infected with hepatitis C. Here, new drugs lead to a cure rate of over 90%, which means a drastic improvement compared to the past.
Hepatitis B infected people get chronic hepatitis in about 30% and are at risk of developing liver cirrhosis in a fifth of cases. On the other hand, there is a high probability of self-healing, especially for those infected with hepatitis B, so that direct therapy directed against the virus is often not recommended, unless a serious course becomes apparent.
An infection with hepatitis A is generally not considered to be chronic, so that a cure is very likely. Nevertheless, people with a weak immune system, for example, can go through brilliant processes that can be life-threatening.
What vaccinations are there against hepatitis?
Vaccinations against hepatitis A and hepatitis B are currently available, as well as combination vaccines of both. These are dead vaccines, consisting of parts of dead pathogens or complete dead pathogens.
The vaccination for basic immunization against hepatitis B is recommended by the Standing Vaccination Commission (STIKO) from the second month of life. The vaccination against hepatitis A is only recommended for people at risk who are in risk areas, as well as for medical staff, people who work in the food industry or as sewer workers. Vaccinations against hepatitis C or E are not available. A hepatitis D infection is only possible in connection with a hepatitis B infection, so one has sufficient protection with existing hepatitis B immunity.
Vaccination against hepatitis A
As mentioned above, the STIKO promises to recommend vaccination against hepatitis A for people at risk as necessary. This also includes travelers who are staying in subtropical or tropical countries that have high rates of hepatitis A infections. The vaccination consists of two injections that are given 6-12 months apart. The vaccination protection then exists for at least ten years, but can also be checked at any time with a blood test. After ten years or inadequate vaccination protection, a booster can take place.
Read more on this topic at: Vaccination against hepatitis A
Vaccination against hepatitis B
As already mentioned, the hepatitis B vaccination is recommended by the STIKO from the second month of life and takes place in combination with other vaccinations. These are administered once in the second, once in the third and once in the fourth month of life as a 6-fold vaccination. Between the eleventh and fourteenth months, the last injection of the 6-fold vaccine required for basic immunization takes place. The success of the vaccination is then checked four to eight weeks after the last dose of the primary vaccination course. If the values are sufficiently good, no refreshing is usually necessary.
Read more about this under: Vaccination against hepatitis B
What side effects can a hepatitis vaccination have?
Like any drug, any vaccination can cause different side effects. Basically, the vaccinations against hepatitis A and hepatitis B are dead vaccinations and are not contagious. In general, it can be said that headache, fatigue, pain and redness at the injection site are very common. This should usually not last for more than three days. Very often here means that one or more than one in ten vaccinated people may have these symptoms.
In addition, diarrhea or nausea can often occur, i.e. one in ten people vaccinated. Swelling, bruising or itching at the injection site are also common. One in one hundred vaccinated people may develop dizziness, vomiting and abdominal pain or a slight infection of the upper respiratory tract with a fever of 37.5 ° C or more.
There are also a number of side effects, but they only occur rarely or very rarely. The manufacturers of these vaccine preparations list these side effects in the package insert, which were found in large-scale studies. Of course, this does not mean that side effects have to occur.
What is the hepatitis titer?
After a vaccination, a blood test can be used to check the success of immunity against a certain disease. For this purpose, the so-called titer determination is used, in which one determines how many effective antibodies are dissolved in the blood serum that are just sufficient to be effective against the virus. Through the vaccinations, in this case possible against hepatitis A and B, the body produces so-called antibodies. When they come into contact with the virus, they can dock onto it, i.e. mark it so that other cells of the immune system can render it harmless. The STIKO (Standing Vaccination Commission of the Robert Koch Institute) recommends, for example, vaccination against hepatitis B from the second month of life after birth in a 6-fold vaccination. After the basic immunization is completed after 4 doses and about a year, the immunity is checked with a titer determination. This is necessary because experience has shown that there are people who react less strongly to the production of the above-mentioned antibodies. They then need another vaccination.
Complications
In the case of fulminant liver failure, the liver functions can no longer be maintained. As a result, the formation of coagulation factors is severely impaired, so that there is a tendency to bleed. If the detoxification capacity of the liver is impaired, toxic metabolic products accumulate in the blood, which lead to damage to the brain (hepatic encephalopathy). In the final stage, this leads to hepatic coma (coma hepaticum).
In addition, severe impairments of the kidneys (hepatorenal syndrome) and the hormonal balance (endocrine disorders) can occur. Chronic hepatitis can lead to cirrhosis of the liver, which in turn can develop into a liver tumor.
Can hepatitis be fatal?
Here, too, a distinction must be made between the various causes of hepatitis, because not all forms become chronic or have to be fatal. First and foremost, the age of the sick person as well as his physical constitution but also previous illnesses are decisive. The liver is a very important and complex metabolic organ and therefore urgently needs therapy in the event of severe inflammation. Nevertheless, hepatitis can be fatal after a long course of the disease.
What are the consequences of hepatitis?
The long-term consequences of hepatitis vary depending on the pathogen and cause. A hepatitis A infection usually heals completely, i.e. it does not become chronic and in acute form only rarely leads to liver failure.
A hepatitis B infection leads to a chronic course in 30%. Of these chronic courses, cirrhosis of the liver can develop in about a fifth of cases within ten years.
In the case of a hepatitis C infection without therapy, about 85% of the cases become chronic. Here especially in cases that run without symptoms. Of these chronically infected courses, around a fifth will develop cirrhosis of the liver within 20 years. The consequences of cirrhosis of the liver are a scarred remodeling of the liver tissue with a loss of cells to carry out their original task. Loss of the liver is incompatible with life, meaning that those affected can depend on a liver donation.
Hepatitis combined with HIV
The HIV virus does not generally attack the liver cells.But if infectious hepatitis occurs, the therapy must be adapted to each other. This is important because some drugs that are used in HIV infection can be toxic to the liver. The combination of both diseases is usually associated with drug abuse, which can promote both infections by sharing syringes.
It can still be stated that an HIV infection together with a hepatitis C infection has a higher virus concentration overall in the various transmission routes, so that there may be an increased probability of transmission. This is particularly the case in the transmission from a pregnant woman to the unborn child.
Hepatitis in pregnancy
A hepatitis infection during pregnancy should always be clarified as a precaution. This means that mothers from vulnerable areas or living conditions should be screened for possible infection. In the case of hepatitis B and D, this plays an important role, because here it is particularly important in the case of an existing infection to keep the virus concentration as low as possible through drug therapy in order to avoid transmission to the child during birth. As a prophylaxis, the child is also vaccinated directly after birth.
A hepatitis A infection can be prevented in advance with a vaccination. In addition, certain nutritional information should be observed, such as not consuming raw animal foods and only drinking water in endangered areas after it has been sufficiently boiled ("Cook it, peel it or leave it!") . Prevention of a hepatitis A infection is particularly important, as infections of this type can take a particularly serious course in pregnancy in up to 20% of cases, which can be life-threatening for mother and child.
A hepatitis C infection usually shows only a low risk of transmission to the child, so that no change to a delivery strategy has to be made. Breastfeeding does not have to be omitted either, because here too the transmission is to be regarded as unlikely.