The anatomy and function of the synovial membrane
definition
The synovial membrane (synovial nerve and synovial membrane) lines the joint capsule, tendon sheaths and bursa from the inside.

Their primary function is the production of synovial fluid, which nourishes the cartilage and is supposed to reduce friction.
In addition, some of the cells of the synovial membrane have a phagocytic effect, which means that these cells can take up tissue debris and microorganisms and dissolve them using enzymes.
anatomy
The anatomy of the synovium differs from the other internal body cavities, which are continuously covered with either endothelium, epithelium or mesothelium, which originate from all three germ layers of embryonic development.
This is different with the synovial membrane or synovial membrane. She is called by so-called Synoviocytesthat are not epithelial cells and arise from the mesenchymal connective tissue, i.e. embryonic connective tissue, are lined.
The mesenchyme comes from the mesodermal cotyledon. The mesenchyme develops in all of the connective tissue that the body has. Therefore it is also the origin for joint capsules and their inner lining.
The synovial membrane consists of two layers:
The Intima and the vascularized Subintima.
Intima
The intima consists of the synoviocytes and an amorphous extracellular matrix. The synoviocytes do not have a continuous basement membrane, which is only formed in pieces, and are divided into type A and type B. The cells of type A have a phagocytic function, they take up and break down cell and tissue debris. It is assumed that they come from mononuclear cells of the blood and are local macrophages, comparable to the Kupffer cells of the liver.
The synoviocytes of the Type B are the producing cells that produce a mix of hyaluronan, collagen and fibronectin and release it into the environment and the joint cavity. so you are producer of synovia ("joint fluid")which nourishes the cartilage and reduces friction in the joint. In order to be able to fulfill this task, which requires the production of many proteins, type B synoviocytes have a particularly large number of rough endoplasmic reticulum, which is very important for the production of secretory proteins.
In general, the synoviocytes have a very polymorphic appearance and can appear flattened, cubic, spindle-shaped or macrophage-like.
Subintima
Below this intimal layer, which consists of a few cell layers, there is the so-called subintima. This consists of loose connective tissue, which is very well supplied with blood. It contains other cells such as fat cells, macrophages and fibroblasts. This layer forms a kind of buffer layer between the intimal synoviocytes and the tight and relatively hard connective tissue of the joint capsule.
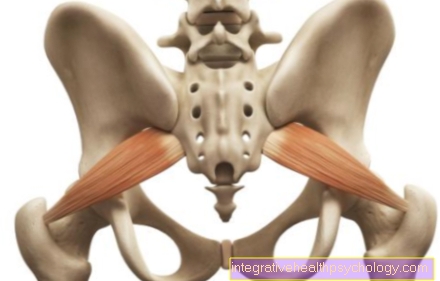
It should also be noted here that a synovial membrane is also in Bursa and Tendon sheaths is formed and here too, although with a slightly different anatomical structure, is responsible for the production of synovial fluid.
function
The joint is surrounded by a joint capsule that divides the joint cavity and the surrounding tissue into two compartments. The joint cavity is thus isolated and bacteria and other stimuli cannot penetrate; on the other hand, the synovial fluid cannot “seep” into other tissue. This is also necessary because the quality of the synovial fluid must be preserved.
The primary function the joint mucosa, or synovialis, is the Production of synovial fluid and the Assurance of goodness this. For this purpose, the blood serum is filtered to a certain extent and thus provides the necessary fluid. The synoviocytes then add hyaluronan and other mucus-forming substances to this, so that an increased viscosity is created. In addition, the synovia also serves the Nutrition of the metabolically slow cartilage.
To ensure the quality of the synovial fluid, the synovial membrane has cells that have a phagocytic function. They can absorb and break down cell and tissue debris. You can also fight bacteria and, if necessary, cause an inflammatory reaction.
Synovial fluid
The joint fluid, also called synovia or colloquially "synovial fluid", is formed by the synoviocytes and is in Joint cavities, Tendon sheaths and Bursa available.
It usually has a clear, slightly yellowish color and is of a viscous consistency. In trauma, for example meniscus tears, it can also appear bloody. In the case of bacterial infections, it becomes purulent and yellowish.
Your primary functions on the one hand are the Reduction of friction in the joint or in the tendon sheath. Due to its jelly-like consistency, it prevents the joint surfaces from rubbing against each other too much and thus wearing out.
Your second important function consists in the Articular cartilage nutrition. This is not permeated with vessels and is therefore cut off from the blood supply. Both nutrients and oxygen only get into the cartilage through diffusion and thus to the cartilage-forming cells. This is only possible because the cartilage has a very slow metabolism, which is also known as bradytroph.
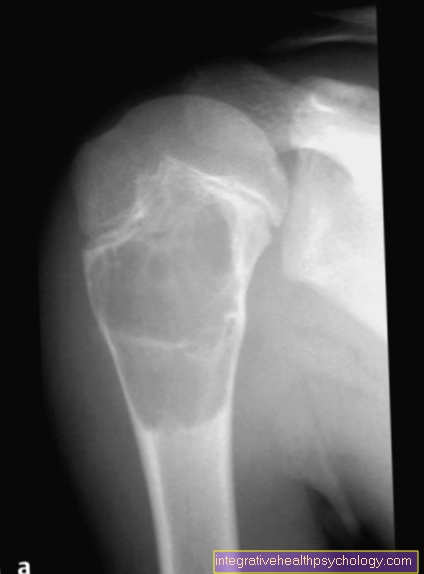
If too much synovial fluid forms in the joint cavity, which cannot be reabsorbed quickly enough, a Joint effusion which can be painful and impair the function of the joint.
Synovial inflammation
The Synovial inflammation, also Synovitis called, refers to a painful and swelling reaction of the body in the area of the synovial membrane (synonyms: synovium or synovial membrane).
It can become a Redness and Overheating of the joint come. In addition, fluid can also build up and lead to joint effusion. The function of the joint can be impaired and a Stiffness of the affected joint can occur.
An inflammation of the synovial membrane can have a variety of causes. Fall under it Trauma, autoimmune and metabolic diseases, Infections and wear-related inflammation.
Traumas, i.e. physical damage caused by a fall or impact, for example, can trigger the inflammation. Likewise, an advanced arthrosis cause the cartilage and bones to rub, causing inflammation.
Involvement of a joint by one bacterial or viral pathogens also triggers an immunological response, whereby both the pathogen itself and the resulting reaction can cause lasting damage to the joint.
Autoimmune diseases like that Rheumatoid arthritis or the Psoriatic arthritis also attack the joints and trigger inflammation there. Metabolic diseases like that too gout lead to inflammation and destruction of the affected joint by depositing crystals there, which then activate the immune system.
Therapy should be anti-inflammatory and address the cause.
It is important to note that synovial inflammation of any kind can destroy a joint as the immune response releases enzymes and recruits cells that can also destroy healthy tissue.
Read more about the topic here: Synovitis
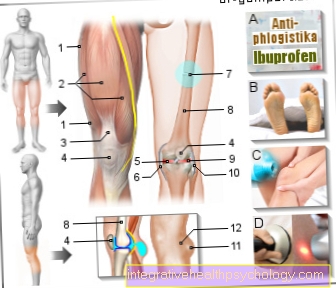
Inflammation of the synovial membrane in the knee
The synovial inflammation in the knee can have a variety of causes.
A distinction is made between acute and chronic synovitis.
In the case of chronic inflammation of the synovial membrane, it makes sense to find out the cause and to combat it. Acute synovitis, for example due to trauma, usually subside by itself.
In general, cooling and elevation are useful in order to reduce the pain and also to reduce the joint effusion. If there are symptoms of the joint effusion, a puncture may be useful. Simple pain medication usually helps against the pain.
Synovectomy
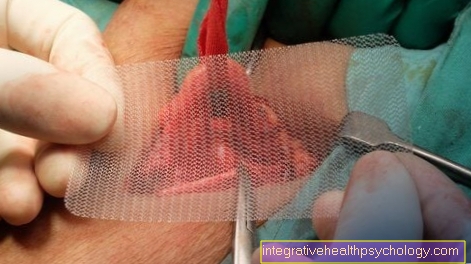
If necessary, the Synovial membrane removed from a joint be to the To improve the patient's symptoms or a more extensive one Prevent destruction of the joint from an inflammatory reaction.
The most common reason for a synovectomy is for treatment rheumatoid arthritis either preventive or reconstructive, if damage is already present. It should be noted that early, preventive synovectomies, if the cartilage and bone have not yet been destroyed, achieve better results.
The purpose of the removal is to remove the inflamed tissue so that the inflammatory reaction subsides. If you let this run free, healthy cartilage, bone and connective tissue would be destroyed, as these components are also attacked.
The procedure itself can ultimately do both open as well as arthroscopic occur. In the open variant, an incision is made and the joint capsule is opened. The arthroscopic method is minimally invasive and does not open the entire joint cavity.
Radiosynoviorthesis
The radiosynoviorthesis is used in chronic inflammatory joint disease applied, such as the rheumatoid arthritis, Psoriatic arthritis or one activate osteoarthritis. Radioactive beta emitters are inserted into the joint by the doctor, which then inhibits growth and causes scarring of the synovial membrane.
This serves the Prevention of further destruction and the Reduction of pain.











.jpg)