Claw hand
What is a claw hand?
The claw hand (or claw hand) is the main symptom of damage to the ulnar nerve (ulnar nerve). The elliptical nerve arises from the brachial plexus, a plexus of nerves at the level of the cervical spine, and runs downwards on the back of the upper arm. Near the elbow, the ulnar nerve runs to the forearm and on to the hand. Many are familiar with the uncomfortable feeling of bumping the "funny bones or nerves". The ulnar nerve is affected and triggers the pain and sensory disturbances in the arm and hand.
In the hand, the nerve supplies the little and ring fingers, as well as the palm and parts of the back of the hand underneath, sensitively (with tactile sensation). It also controls various muscles of the forearm and hand that enable the hand to flex and move the fingers (spreading, bending, etc.). Due to its relatively superficial course on the elbow and forearm, it is particularly often affected by injuries. The ulnar nerve paralysis is therefore the most common nerve paralysis of the extremities.

Concomitant symptoms
In addition to the claw hand, depending on the level of damage, sensory disturbances in the hand can also occur. These affect the ring and little fingers as well as the adjacent half of the hand on the palm and back of the hand. The higher the damage, the more extensive the failures. This can be numbness, tingling, temperature changes, burning or pain. If the paralysis lasts for some time, visible muscle wasting of the hand occurs.
Find out more about the topic: Nerve damage
Pain
The damage to a nerve can manifest itself in many ways. Pain also occurs. Sometimes immediately after the damage, possibly after a while. These are typically spasmodic and can feel burning, stabbing, or dull. This so-called nerve pain (neuropathic pain) can be extremely stressful. Treatment is different from other types of pain. Antidepressants, drugs against epilepsy (anticonvulsants), opioids, or local anesthetics (lidocaine, capsaicin) are used. Physiotherapy or occupational therapy are also helpful.
Find out more about the topic: Nerve pain
deafness
The described discomforts can manifest themselves in very different ways. Those affected often complain of a feeling of numbness. Many people know this feeling when you hit your elbow and with it the “funny bone or nerve”. This can be accompanied by pain, temperature abnormalities or the feeling that the arm and hand have "fallen asleep".
Read more on the topic: deafness
Cause nerve damage to the ulnar nerve
In the case of damage to the ulnar nerve, a distinction is made between three locations: elbow, wrist and palm. The elbow can be damaged by broken bones, incorrect positioning during an operation, inflammation or age-related tissue deterioration. Cuts on the wrist and prolonged pressure in the palm of the hand (e.g. from tools or cycling) are the most common causes.
The earlier the nerve is damaged in the course, the more pronounced the overall extent of the failure symptoms. However, there is always an image of a clawed hand. This posture arises from the failure of the muscles supplied by the ulnar nerve and the now predominant pull of their opponents. The base joints of the fingers are hyperextended, the middle and end joints are bent. This is most clearly visible on the ring and little fingers. If there is damage at the level of the elbow, the thumb can no longer be pulled sideways to the ring finger and sensory disturbances (numbness, tingling) occur on the half of the hand on the part of the ring and little finger.
In the case of injuries at the wrist level, accompanying, albeit less pronounced, sensory disturbances also occur. If the location of the damage is in the palm, on the other hand, only the claw hand appears.
Clawed hand after a stroke
In the event of a stroke, blood clots or bleeding in the brain lead to a lack of oxygen and cell death. Descending nerve fibers are tightly bundled here, so that a stroke causes extensive symptoms of failure (abnormal sensations, paralysis). It is unlikely that only a single nerve is affected.
The affected nerves and the muscles they supply can, however, be impaired to different degrees and regain their functionality to a greater or lesser extent. If the paralysis continues, it goes from flaccid to cramped (spastic). Persistent muscle cramps (spasticity) can also lead to the appearance of the clawed hand.
Find out more about the topic: Spasticity
diagnosis
The targeted examination of muscle functions and changes in posture is groundbreaking for diagnosis. With severe paralysis, the patient is no longer able to hold a sheet of paper between thumb and forefinger without bending the thumb in the wrist (Fromment's sign). In addition, the thumb is often hyperextended in the base joint (Jeanne's sign). The patient is asked to bend the wrist on the ring and little finger side and the metacarpophalangeal joints against resistance, to spread the long fingers and to make snapping movements with the thumb and forefinger against the flat hand of the examiner. Weaknesses here suggest paralysis.
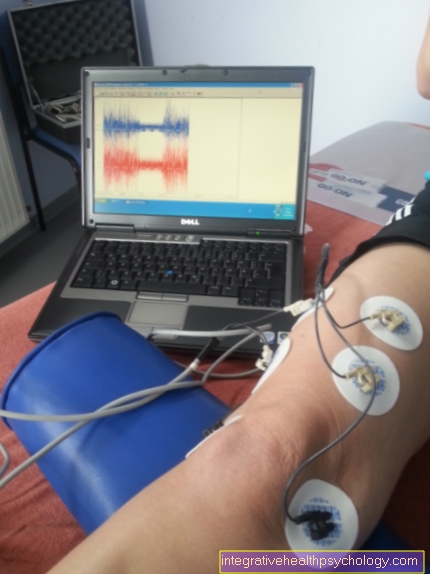
Electronurography (NLG)
Electronurography should be used for a reliable diagnosis. You set an electrical stimulus and divert the electrical potential of the nerve. This is how you test the nerve conduction speed, among other things. A decrease suggests damage. This diagnostic method is very sensitive, but does not allow any statement about the cause of the damage.
Read more on the topic: Electroneurography
Treatment / therapy
The therapy consists primarily of protecting the elbow region (e.g. do not put the bent elbow down). A splint or padding can be used as a support. If the symptoms get worse, the possibility of surgical relief should be considered. There are two different approaches: One possibility is to relocate the nerve from the bone groove on the elbow to the elbow, where it is more protected.
In another, gentler method, the tissue surrounding the nerve on the elbow is cut. In the course of healing, there is scarring, stretching and thus pressure relief. The minimally invasive endoscopic operation is new (only 2-3 cm instead of 10-12 cm long incision). However, it is not yet very widespread as it requires specialized instruments.
Occupational therapy
Paralysis or muscle weakness can be treated through targeted training as part of occupational therapy. The aim is to regain strength and fine motor skills. It is important that the affected muscles are exercised regularly and continuously through special exercises.
Duration
Acute pain or tingling often improve quickly. However, depending on the extent of the damage, numbness, tingling sensations, and muscle weakness may take some time to resolve completely. Complete regeneration can take more than 12 months.
What are the chances of recovery?
If therapy is started early, the chances of recovery are good. Consistent relief of the nerve is important. The use of rest, occupational therapy and physiotherapy and, if necessary, surgical relief usually allow a good prognosis. Of course, always depending on the extent of the damage. As a rule, muscle function and sensation in the affected areas are regained.