Inflammation of the pancreas
Synonyms: Pancreatitis; Pancreatitis
introduction

The Inflammation of the pancreas can be divided clinically into two different forms, the acute and chronic form.
In the case of a acute inflammation the pancreas feel the affected patient severe pain in the upper abdomen which start suddenly and without warning.
In addition, the presence of acute inflammation of the pancreas is evident in most cases nausea, Vomit, Constipation and high fever. Acute inflammation of the pancreas is treated with intravenous fluids and pain relievers (analgesics).
A chronic inflammation the pancreas, however, is characterized by recurring (recurrent) Upper abdominal pain. Even with chronic inflammation of the pancreas it can nausea and Vomit come. However, the affected patients also notice one steady weight loss.
Regardless of the course of the inflammation of the pancreas in the respective patient, should immediately consulted a specialist and appropriate drug treatment initiated.
Acute inflammation of the pancreas
Acute inflammation of the pancreas is characterized by self-digestion (Autodigestion) of the organ. The affected patients will be different Digestive enzymes (for example: trypsinogen and Phospholipase A) already activated inside the pancreas. In this context, the digestive enzyme trypsinogen plays a crucial role in the development of acute inflammation of the pancreas. This enzyme is a substance that usually only reaches the duodenum (Duodenum) into its active form (Trypsin) is disassembled. If this activation happens too early, i.e. already within the pancreas, it happens proteolytic and lipolytic Events. It comes to a self-digestion of the organ and the development of pronounced inflammatory processes.
Acute inflammation of the pancreas is a potentially life-threatening condition that requires urgent medical intervention. On average, there are around five to ten new cases per 100,000 inhabitants per year in Germany.
causes
The acute form of inflammation of the pancreas can have different causes.
Gallstones (Choledocholithiasis) represent the most common cause of acute inflammation of the pancreas in this context. After these gallstones have been flushed out of the Gallbladder they can be found in the mouth of the bile duct into the Duodenum fix. Since this mouth is also the exit point of the pancreatic duct (Papilla vateri) becomes a Reflux of the synthesized secretions triggered. As a result, the bile acid causes damage to the pancreatic tissue.
In addition, the regular excessive consumption of alcoholic beverages One of the main causes for the development of an acute inflammation of the pancreas. Chronic alcohol abuse leads to an increase in the permeability of the duct system inside the pancreas and, as a result, to relevant changes in the secretion and composition of the bile. In addition, various closure systems of the biliary and pancreatic duct systems are negatively affected by regular consumption of alcoholic beverages.
In about 15% of patients affected by acute inflammation of the pancreas, however, the cause can be found despite extensive searches no direct justification for the development of the clinical picture. In these cases one speaks of a so-called "idiopathic acute inflammation of the pancreas“.
Other causes of acute pancreatitis are:
- viral infections (mumps, hepatitis, HIV, Cytomegaly)
- increased blood calcium levels Overactive parathyroid glands
- severely increased blood lipid levels (hypertriglyceridaemia)
- Tumors
- Genetically (for example with Cystic fibrosis)
- Autoimmune diseases
- traumatic
- Drug-associated
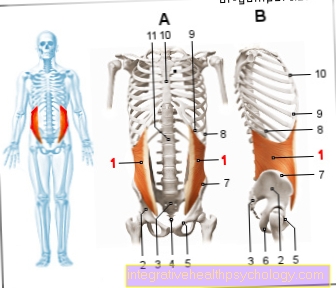
Symptoms
When the inflammation of the pancreas is acute, the symptoms appear suddenly and without warning on. Most of the affected patients feel violent at the beginning Pain in the upper abdomen (so-called epigastrium). In most cases, this pain radiates into the lower back in a belt shape. During the physical examination, significant pain phenomena can be provoked by exerting pressure on the abdomen. In addition, the so-called "Rubber belly“That through severe flatulence and a pronounced defensive tension is evoked, to the typical symptoms of acute inflammation of the pancreas.
In addition, some of the affected patients report Pain in the lower thoracic spine which should steadily increase in intensity.
Further symptoms that occur in the presence of the acute form of the inflammation of the pancreas nausea and Vomit.
In addition, many of the patients suffer from severe constipation and general symptoms like fever and chills.
In severe cases of acute inflammation of the pancreas occur Jaundice (Jaundice), Water retention in the abdomen (Ascites), Pleural effusions and Shock situations on.
Furthermore, the affected patient can be examined during the physical examination blue-green discoloration in the area of the navel (Cullen sign) or in the Flanks (Gray Turner sign) Find.
diagnosis
Even questioning the patient regarding the pain he has felt provides a decisive indication of the presence of an acute inflammation of the pancreas. If further signs are found during the clinical examinations, a laboratory examination should be initiated immediately. Laboratory diagnostics can detect elevated serum concentrations of the pancreatic enzymes trypsin, amylase and pancreatic lipase in patients suffering from acute inflammation of the pancreas. In general, one can assume that the level of these pancreatic enzymes that can be detected in the blood serum reflects the degree of inflammatory processes within the organ.
In addition, the normal values for magnesium, sodium and potassium, as well as the concentrations of bicarbonate, sugar and fats in patients suffering from acute inflammation of the pancreas, are clearly increased. In contrast, the calcium concentration in the blood serum is reduced in many cases.
Complications
Acute inflammation of the pancreas can result in failure of timely extensive treatment serious complications to lead. One of the most common problems observed in the course of this disease is tryptic digestion of neighboring organs and structures.
The formation of so-called "Pseudocysts“And the emergence of Blood clots within the portal vein are among the most common complications of acute inflammation of the pancreas.
In addition to possible damage to organs, acute pancreatitis can also occur Impairments to the cardiovascular system to lead. Affected patients often develop in the course of the disease Dehydration, one sharp drop in blood pressure or one life-threatening shock.
In addition, poorly treated acute inflammation of the pancreas can develop Heart, lung or Kidney failure come.
therapy
Therapy should be started as soon as possible if there is an acute inflammation of the pancreas. As soon as there is a suspicion that inflammatory processes in the pancreas must be present immediately with an intravenous fluid (infusion) can be started. This measure can prevent the development of a life-threatening volume deficiency shock.
In addition, an adjustment of the eating habits represents a decisive step in the treatment of the acute inflammation of the pancreas. In the case of severe forms, a special Nasal and small intestine probe be inserted.
Pain therapy in particular represents an important step in the treatment of acute inflammation of the pancreas.
If the pancreatitis is caused by obstruction of the bile ducts, the gallstone must be removed.
If an infection is suspected, antibiotic therapy must be started.
Chronic inflammation of the pancreasIn the chronic form Inflammation of the pancreas is a disease with persistent inflammatory processes within the tissue of the organ. Affected patients show severe pain in the abdomen and / or one permanent dysfunction of the pancreas on.
The incidence of chronic inflammation of the pancreas is currently 10 / 100,000. In most cases, those affected are men between the ages of 30 and 60. The gender ratio in the acute form of inflammation of the pancreas is about 9: 1 (men compared to women).
causes
The most common cause for the development of chronic inflammation of the pancreas is an over a long period of time persistent alcohol abuse (about 80% of known cases). The alcohol consumption necessary to trigger inflammatory processes in the pancreas is average more than 80g over a period of six to twelve years. Regular consumption of alcoholic beverages alone does not, however, represent a risk factor for the development of chronic pancreatitis. Rather, it is one crucial cofactorbecause only 10 percent of heavy alcoholics will develop chronic inflammation of the pancreas in their lifetime.
In addition, regular consumption of nicotine as a risk factor for the development of chronic inflammation of the pancreas.
Is it an affected patient? child, it can be a so-called "hereditary autosomal dominant pancreatitis“Act. This form of inflammation of the pancreas carries over repeated flare-ups (acute inflammation of the pancreas) with self-digesting necrosis to the chronic form. The direct cause in these cases is a mutation in the gene coding for the synthesis of the pancreatic enzyme trypsinogen (PRSS1) or in the gene of the Serine protease inhibitor SPINK1. Triggered by these two crucial mutations, there is an auto-activation of trypsinogen to trypsin and an associated one within the pancreas Autodigestion of the pancreatic tissue.
The so-called "autoimmune chronic inflammation of the pancreas“Is also through a genetic malfunction triggered.
Other causes for the development of chronic inflammation of the pancreas:
- idiopathic (with no known cause)
- Drug-associated (Diuretics, Beta blockers, ACE inhibitors, Cytostatics, Antibiotics, Anti-epileptic drugs, etc.)
- Persistent hypercalcaemia Overactive parathyroid gland
- Hyperlipidemia
- Chronic renal failure
- Tumors
- Narrowing of the pancreas and bile ducts
- Genetic factors
Symptoms

Steady recurring pain that are not colicky and over hours to days can persist, are considered the main symptom of chronic inflammation of the pancreas. Typically, the pain is localized on the affected patient Upper abdomen.
Even with chronic inflammation of the pancreas, the pain felt by the patient can radiate to the flanks and lower back.
While the pain can be very severe at the beginning of the disease, the symptoms often decrease in the later course. Many patients are even perfect with advanced chronic inflammation of the pancreas painless.
In addition, those affected often have a pronounced Food intolerance observe. It is still unclear whether this food intolerance is caused by the inflammatory processes themselves or simply by the fear of pain after eating.
It also causes chronic inflammation of the pancreas frequently nausea and Vomit. The affected patients increasingly lose weight as the disease progresses. Due to the restricted function of the pancreas, fewer digestive enzymes are in the Small intestine released. As a result, various food components can no longer be digested. It comes to the creation of Fatty stools, Diarrhea and Flatulence.
In addition, due to the limited release of insulin a secondary Diabetes mellitus arise.
Complications
An untreated chronic inflammation of the pancreas can serious complications entail. The most common problems that arise in the course of chronic pancreatitis include Pseudocysts within the tissues of the pancreas and Abscesses.
Furthermore, it can lead to thrombosis of spleen- and Portal vein system and an accompanying one portal hypertension come.
Many of the affected patients develop additionally Stenoses in the area of the bile duct system. The consequence of this constriction is a backflow of the bile, which is more visible Yellowing of the sclera and skin (Jaundice).
The development of malignant changes in the pancreatic tissue is regarded as a late complication, especially in hereditary forms of chronic inflammation of the pancreas (Pancreatic cancer).
diagnosis
Already the Interviewing the affected patients can provide an initial indication of the presence of chronic inflammation of the pancreas.
Clinically, patients typically show one pronounced emaciation (Cachexia). The abdomen of a person with chronic pancreatitis usually appears distended and inflated resilient. In medical terminology, this phenomenon is called "Rubber belly“.
In addition, the intestinal noises are often weakened due to the reduced function of the pancreas. When palpating the abdomen, a Tenderness be provoked.
If there is persistent suspicion of chronic inflammation of the pancreas, the Blood test often certainty. The pancreatic enzymes (amylase and lipase) in serum blood are usually markedly increased. Decreased chymotrypsin and elastase concentrations can be detected in the stool of the affected patient.
To prove that the exocrine part of the pancreas is not functioning properly, the so-called "Secretin pancreozymin test" be performed. The suspect patient is given an intravenous injection of the hormone secretin for this purpose. The secretion secreted by the pancreas is then collected by a small intestinal probe and the concentrations of bicarbonate, chymotrypsin, amylase and lipase are determined.
Calcifications that arise in the course of chronic inflammation of the pancreas can in most cases be means Ultrasound examination be detected. Other diagnostic methods are the Computed Tomography and the Magnetic resonance imaging.
therapy
Patients suffering from chronic inflammation of the pancreas should urgently Avoid consumption of alcoholic beverages and nicotine. It also provides an adequate Pain therapy represent an important step in the treatment of chronic inflammatory changes in the pancreas. In this context, above all non-steroidal anti-inflammatory drugs (short: NSAID) and Opioids to use.
In addition, they often need different Enzymes supplied to the pancreas.
Patients who have a secondary disease due to chronic inflammation of the pancreas Diabetes mellitus develop additionally through the gift of insulin treated.