The pancreas
Synonyms
Medical: pancreas
English: pancreas
anatomy
The pancreas is a gland weighing around 80g and 14 to 18 cm long and is located in the upper abdomen between the small intestine and the spleen. It is actually not inside the abdominal cavity, but very far back in front of the spine. It is therefore not like many other organs of the gastrointestinal tract with which the skin lining the abdominal cavity (peritoneum) is covered.
Due to its appearance, the entire gland is divided into the head (caput), body (corpus) and tail (cauda).

Illustration of the pancreas

- Body of
Pancreas -
Corpus pancreatis - Tail of
Pancreas -
Cauda pancreatisauda - Pancreatic duct
( execution course) -
Pancreatic duct - Duodenum lower part -
Duodenum, inferior pars - Head of the pancreas -
Caput pancreatis - Additional
Pancreatic duct -
Pancreatic duct
accessorius - bile duct -
Common bile duct - Gallbladder - Vesica biliaris
- Right kidney - Ren dexter
- Liver - Hepar
- Stomach - Guest
- Diaphragm - Diaphragm
- Spleen - Sink
- Jejunum - Jejunum
- Small intestine -
Intestine tenue - Colon, ascending part -
Ascending colon - Pericardium - Pericardium
You can find an overview of all Dr-Gumpert images at: medical illustrations
Location of the pancreas
The pancreas (pancreas) lies across the upper abdomen.
During embryonic development, it is completely covered by the peritoneum (intraperitoneal location), but changes its position during adolescence and can be moved behind the peritoneum after birth (peritoneum) Find (secondary retroperitoneal location).
The pancreas is therefore in the so-called Retroperitoneal space and is on the right side by the liver, on the left side by the spleen and forward (lat. Ventral) limited by the stomach. In addition, there are close relationships with the aorta, the inferior vena cava and the duodenum (Duodenum).
The C-shaped loop of the duodenum frames the head of the pancreas (Caput pancreatis).
The remaining sections of the gland also have close anatomical relationships with specific structures in the abdomen.
The great body of the pancreas runs through (Corpus) the upper abdomen and crosses the spine in the area of the second lumbar vertebra.
The tail of the pancreas extends so far into the left upper abdomen that it is adjacent to the left kidney and spleen.
A small protrusion of the pancreas (uncinate process) is found between the head and the body and is in a positional relationship to the most important vessels for the supply of the intestinal tract (arteria and vena mesenterica superior).
Function of the pancreas
The main job of the pancreas is the production of digestive enzymes and digestive hormones.
Here you can find everything on the topic: Pancreatic enzymes
The hormones of the pancreas are released directly into the blood (so-called endocrine secretion).
Enzymes are proteins that are actively able to break down food and prepare it for food intake through the intestinal mucous membrane.
Read more on the topic:
- Function of the pancreas
- Functions of the liver
- Functions of the pancreas

The enzymes reach their place of action in the small intestine via a special outlet duct running lengthways through the entire gland, the pancreatic duct (lat. Ductus pancreaticus). Since the enzymes formed are used to break up food components, they are very aggressive substances. The pancreas therefore has effective protective mechanisms against self-digestion: protein-splitting enzymes (peptidases) such as trypsin and chymotrypsin are formed in the form of inactive precursors. The conversion into "biologically active scissors" takes place in the small intestine (by means of an enzyme called enterokinase, which cuts off small fragments of the trypsin precursor trypsinogen, so that functional trypsin is produced. This is also the activator for the other hormones. The pancreas also produces starch-splitting enzymes (Amylases), fat-splitting enzymes (lipases) and nucleic acid-splitting enzymes (ribonucleinases; these are used to digest cell nucleus components).
However, all of the enzymes mentioned only function optimally if the acid content in their environment is not too high (= pH 8). Since the food comes from the stomach, which is pre-digested with hydrochloric acid, the stomach acid must be neutralized (neutralized) beforehand. To do this, the enzymes are released into the small intestine with 1-2 liters of an aqueous, bicarbonate-rich (= neutralizing) liquid, the pancreas.
Most of the pancreas is responsible for this so-called exocrine function. The exocrine function is the production of enzymes for the digestive tract.
The entire tissue of the pancreas is - like many other glands, e.g. the thyroid gland - divided into lobes separated from each other by connective tissue. The vessels, nerves and lymph vessels that supply the pancreas with blood are located within the connective tissue arteries.
Specialized cells, the glandular end pieces (acini), are responsible for enzyme production. These release the enzymes into ducts running within the pancreas, which ultimately all lead to a large, common duct, the ductus pancreaticus (see above).
What is special about these many small outlets is that they also have another function: They are responsible for neutralizing stomach acid by forming the pancreas.
In contrast, the hormone-producing (endocrine) part of the pancreas is only small. It is also known as the island organ: the arrangement of these cells in groups, which are found diffusely scattered throughout the gland, is reminiscent of islands under the microscope. The most common are the 1 million or so islands in the rear part (called the tail). The most important (and with a share of over 80% also the most formed) hormone is insulin. Its task is to enable the body cells to absorb sugar (glucose; breakdown product of food rich in carbohydrates) and in this way to lower the blood sugar level. If this hormone is absent or deficient, it leads to diabetes mellitus: the blood becomes oversaturated with unused sugar.
The cells that produce insulin are called B cells. A cells, on the other hand, produce an opposing hormone, glucagon. If the last meal was a long time ago, it ensures that sugar is released from the liver's stores. This ensures that the internal organs are adequately supplied at all times (especially from the brain, which is dependent on sugar and cannot rely on other food components).
Only a very small proportion of the hormone formation is accounted for by those messenger substances that are produced specifically for the regulation of the pancreas itself: the hormone of the D cells, which has an inhibitory effect on insulin and glucagon production, somatostatin, and the pancreatic part that inhibits the digestive enzymes (exocrine) Polypeptide (PP).
The hormones specially formed for this purpose and the autonomic nervous system are also responsible for regulating the release of enzymes. (This part of the nervous system is also referred to as the autonomous, i.e. independent nervous system, as it controls the unconscious processes taking place in the body.
Together, the part of the autonomic nervous system called the parasympathetic nervous system and the hormone cholecystokinin (CCK for short) stimulate enzyme production. As a hormone, secretin also stimulates the release (= secretion) of water and bicarbonate by the cells of the pancreatic ducts.
Both secretin and cholecystokinin are produced by specialized cells called S cells and I cells. These are scattered between the surface cells in the entire gastrointestinal tract (especially in the small intestine) and are collectively referred to as enteroendocrine cells (= large enteron = intestine, corresponding to the main organ of action of these hormones).
Through this complex interaction of various regulatory mechanisms, the entire digestion and the sugar balance of the body are regulated by self-regulating mechanisms. This principle can be found in different parts of the body, e.g. in the thyroid.
Normal values / blood values of the pancreas

A number of values that can be detected in the blood and / or urine can be used to assess pancreatic function.
For this reason, knowledge of the normal values is all the more essential for the treating doctor.
Pancreatic amylase (alpha-amylase), an enzyme used to digest carbohydrates, can be found in blood serum, 24-hour urine, and even in the fluid from ascites.
The normal values for a woman are around 120 U per liter (U / L) in blood serum and around 600 U / L in urine. The same standard values apply to men.
Further information on this topic can be found at: Alpha amylase
In addition, bilirubin (or urobilinogen) can be detected in blood serum, plasma and urine. The norm in the adult blood serum is between 0.1 and 1.2 milligrams per deciliter (mg / dl). The urine should normally not contain any bilirubin components. In relation to diseases of the pancreas, an increased bilirubin value indicates the presence of a cyst with a narrowing of the drainage paths of the gallbladder.
The number of white blood cells (Leukocytes) in whole blood or urine can be used as a parameter. The normal value of a healthy adult in whole blood is between at least 4000 and at most 10,000 leukocytes per microliter. In healthy people, no white blood cells should be detectable in the urine, because the excretion of leukocytes with the urine always indicates a pathological process. In most cases, an increased number of leukocytes is caused by an inflammation within the organism.
In addition, a decrease in the calcium concentration in blood serum and / or urine suggests inflammation of the pancreas (normal value: 8.8-10.4 mg / dl).
The enzyme chymotrypsin can be determined in the stool; in healthy people the normal value is around 6 U / g, a decrease can indicate a decrease in the function of the pancreas.
A decrease in the pancreatic lipase concentration also indicates a decrease in function (normal value: 190 U / L).
Read more on the subject at:
- Lipase level
and - Lipase increased
Other relevant values:
- LDH (lactate dehydrogenase)
- Sample: blood serum, blood plasma
- Normal value: 120-240 U / l
- Creatinine
- Sample: blood serum, urine
- Normal value:
Serum: approx. 1.0 mg / dl
Urine: 28-218 mg / dl
Further information also under our topic: Creatinine
- insulin
- Sample: blood plasma, blood serum
- Normal value: 6- 25 mU / l (fasting)
- Elastase 1
- Sample: blood serum, stool
- Normal value:
Serum: approx. 3.5 ng / l
Stool: 175-2500 mg / g
Further information also under our topic: Elastase
Symptoms that can come from the pancreas
The most common disease of the pancreas in the broadest sense is the inadequate supply of vital insulin. The resulting disease, also known as diabetes mellitus, is very common in western countries. Since it usually does not initially cause any acute symptoms, diabetes is usually only diagnosed through routine examinations.
Pancreatitis is much more painful. It is usually caused by excessive alcohol consumption and can be either chronic or acute. Characteristic are mostly pulling or dull, belt-like pains that originate between the stomach and belly button and can then pull back around the back. The pain is described as extremely uncomfortable and excruciating. Most of the time, the patients are also in a poor general condition, which can also be accompanied by a pale complexion, pronounced weakness or a high fever. In addition to acute and chronic alcohol consumption, diagnostic measures such as the so-called ERCP (an examination in which a contrast agent is injected into the biliary and pancreatic ducts) lead to inflammation of the pancreas. Diagnostically, a tender upper abdomen, back pain and a noticeable blood count (increased lipase levels and inflammation levels) indicate inflammation of the pancreas.
In the ultrasound one can often see a swollen organ with inflammatory fluid often washed around it. The medical questioning and, above all, the exact documentation of alcohol consumption can provide further important information as to whether or not it is a pancreatitis.
Once the diagnosis of inflammation of the pancreas has been made, treatment must be started immediately, as further waiting can lead to a situation that is sometimes life-threatening. As a rule, patients have to take a 24-hour nutritional abstinence after the diagnosis. Then the slow diet can be started again.
It is important that the patient does not drink alcohol. In addition to these abstinent measures, immediate antibiotic treatment should be started and carried out consistently. In some cases it may also be necessary to give the antibiotic to the patient as an infusion.
Other diseases that are a little less common are of an exocrine nature. In addition to the secretion of insulin, the pancreas plays a major role in digestion and in the breakdown of various substances in food. These enzymes are made in the pancreas and released into the digestive tract when needed, where they are added to the food that is ingested. If there is a so-called pancreatic insufficiency, i.e. a weak pancreas, the vital enzymes for breaking down the food can no longer be released in the amount needed, as they would be necessary.
As a result, the food ingested is no longer broken down as it should. The bowel usually reacts with mushy stools or thin diarrhea.
This is also one of the first symptoms of pancreatic insufficiency that the patient reports. The diarrhea does not get better with medication or comes back as soon as the corresponding medication is stopped.
Perenterol is sometimes attempted for severe diarrhea. It is a yeast preparation that has the task of thickening the stool.
Sometimes pancreatic insufficiency can also lead to a slight improvement in symptoms, which, however, diminishes again after stopping the drug. The suspicion is now often an intolerance reaction of the intestine.
The most common intolerance reactions are lactose intolerance, fructose and gluten intolerance. All of them can be tested and should do this if you have recurring diarrhea. If all tests were normal, it is possible that the cause of the diarrhea is the somewhat rarer pancreatic insufficiency. For this purpose, special tests are carried out in the stool and in the blood before a corresponding diagnosis can be made.
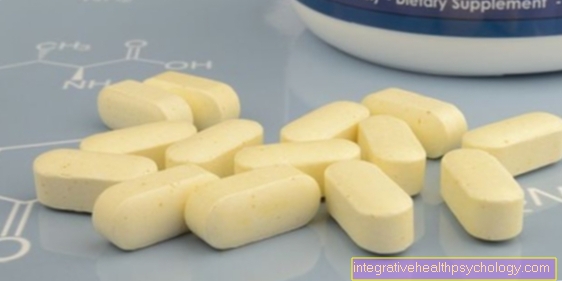
If a diagnosis of pancreatic insufficiency is made, immediate treatment must be given. As a rule, this is combined with precise documentation of the food consumption. Because what is particularly important is what the patient with this disease eats each day. In most cases, the missing enzymes, which are insufficiently produced by the pancreas, are then administered to the patient in tablet form at regular intervals. Depending on whether the diarrhea gets better or not, the dose of the ingested enzymes must be reduced or increased.
As a rule, pancreatic insufficiency is a long-term diagnosis i.e. the pancreas will no longer be able to produce enough of the missing enzymes by itself.
An exception is the pancreatic insufficiency caused by inflammation. As a rule, however, the missing enzymes have to be consumed throughout life.
Read more on the topic: Symptoms of the pancreas
Diseases of the pancreas
Cyst on the pancreas

A cyst of the pancreas (Pancreatic cyst) is a bubble-like, closed tissue cavity within the glandular tissue that is usually filled with fluid.
Possible fluids in a cyst are tissue fluid, blood, and / or pus.
The typical cyst of the pancreas is divided into two classes, the real cyst and the so-called pseudocyst. A real pancreatic cyst is lined with epithelium and usually does not contain any natural enzymes from this glandular organ (Lipase, amylase). The pseudocyst often develops in connection with an accident in which the pancreas is bruised or torn. In contrast to the real cyst, pseudocysts are not surrounded by epithelial tissue but by connective tissue. Since the pancreas enzymes, when released within the tissue, contribute to a process of self-digestion, this type of cyst is particularly dangerous. Typical fluids inside the cyst are blood and / or dead cell debris.
A pancreatic cyst is an extremely painful affair. The perceived pain is not limited to the area of the upper abdomen, but usually even radiates into the back, especially at the level of the lumbar spine. The occurrence of inexplicable back pain is a clear indication of the presence of a cyst. In addition, they express themselves as colic-like pain.
This means that they resemble the contractions during childbirth, that they do not get better or worse through certain movements or relieving postures and that the patient's condition constantly changes between symptom-free and severely limited by the pain.
A cyst of the pancreas can be visualized using ultrasound as well as computer tomography (CT). After a successful diagnosis, the condition of the gland is first observed, which makes sense because many cysts in the pancreatic tissue recede spontaneously and do not require any treatment. Drainage can help with extremely severe symptoms.
The attending physician will gain access to the pancreas by forming a hole in the stomach or intestinal wall, opening the pancreatic cyst and opening a small plastic tube (Stent) insert. This allows the fluid that has collected inside the cyst to drain away. The stent is removed after approximately 3 to 4 months.
Possible complications of a pancreatic cyst are bleeding, abscess formation, water retention in the abdomen (Ascites) and / or the narrowing of the drainage pathways of the gallbladder. The latter leads in many cases to what is called "jaundice" (Jaundice) known phenomenon.
Inflammation of the pancreas
The main cause of inflammation of the pancreas is chronic excessive or acute alcohol consumption. In addition, the pancreatitis is also a complication of the so-called ERCP, an examination method for pancreas diagnostics there. An endoscopic examination is used to inject contrast medium into the pancreatic duct. In some cases this can lead to inflammation of the pancreas, which must then be treated quickly.
The first symptoms of pancreatitis are belt-shaped pain that extends from the abdomen above the navel to the back. The abdomen is very painful on pressure, the character of pain is dull. The main point of pain is between the navel and the lower edge of the breastbone at the level of the stomach. The patients are sometimes very severely affected by the pain and can no longer perform normal movements such as turning or bending forwards or backwards without pain.
In addition to the pain, the patients are sometimes in a very poor general condition; sometimes the pale gray skin color of the patient indicates that he is suffering from a serious, sometimes life-threatening illness. A frequent accompanying symptom is also the fever, which in some patients can be 39-40 degrees and urgently needs to be lowered.
Depending on how severe the inflammation of the pancreas is, the organ may also have insufficient enzyme release, which in turn can have serious effects on digestion and sugar metabolism. This can lead to fatty stools and diarrhea, as the food can no longer be broken down and processed properly as long as the pancreas is in a highly inflamed state. It can also lead to a high level of blood sugar, as the insulin release of the pancreas is insufficient.
In addition to the complaints, the detailed patient survey can substantiate the suspicion of pancreatitis. It is essential to ask patients whether they consume alcohol regularly or excessively or whether they have had a pancreatic examination in the past few months or weeks. The background is that the cause of pancreatitis is often alcohol abuse, as well as what is known as ERCP (endoscopic retrograde cholangiopancreatography examination of the gallbladder, bile ducts and pancreas) the pancreas can become inflamed by the injected contrast agent.
The diagnosis takes place among other things through an ultrasound scan. A cloud-shaped distended pancreas can be seen here.
In addition to consistent abstinence from alcohol and 24 hours of food abstinence, antibiotic treatment is a way of making the patient symptom-free soon. In some severe cases, parts of the pancreas need to be surgically removed.
Read more on this topic at: Inflammation of the pancreas
Pancreatic pain
Pain from the pancreas can manifest itself in different ways. Often they are not clearly recognizable as such. Depending on the cause and severity of the disease causing the pain, it can radiate into the entire abdominal area.
But they can also be felt in a localizable manner. They usually occur in the area of the upper abdomen (also called epigastrium) and radiate in a belt-shaped manner over the entire upper abdomen and into the back. You may also experience pain only in the back or left side at the level of the pancreas. The pain has a different character depending on the cause. In the case of more acute diseases, such as inflammation, they are usually more stabbing, in chronic diseases, such as tumorous changes, the pain is described as rather dull.
Since pancreatic pain is often recognized late as such, it is important to act quickly when it occurs. If such pain persists over a longer period of time, this should definitely be clarified by a doctor.
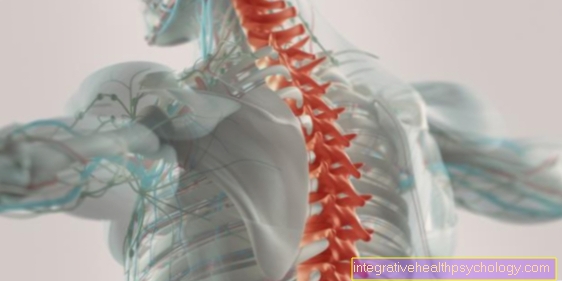
Why does a diseased pancreas cause back pain?
With diseases of the pancreas, pain in the back is common. This can be explained by the location of the pancreas in the upper abdomen. It is located in the back of the abdominal cavity at the level of the lower thoracic vertebrae. Due to its anatomical proximity to the spine in the area close to the back, many pathological changes in the pancreas are expressed in back pain at this level. The back pain is usually belt-shaped and radiates over the entire back area at this height.
It should be remembered that the back pain can only be an expression of a slight irritation of the pancreas, but also an expression of a serious disease of the pancreas. Since this is often difficult to differentiate, a doctor should be consulted in the event of long-term back pain.
You can find more on the subject of "Pain from the pancreas" at: Inflammation of the pancreas
Pancreatic weakness
Pancreatic weakness means that the pancreas cannot function properly. This is particularly evident in digestion: the pancreas is responsible for producing most of the digestive enzymes. These are needed to break down the various components of food, i.e. proteins, fats and sugar, so that they can then be absorbed in the intestine and stored in the body. If the pancreas becomes weak, the digestive enzymes, such as trypsin or cholesterol esterase, can only be released to a reduced extent and are effective. This is particularly evident in the form of gas, loss of appetite and food intolerance. However, since these symptoms also suggest other causes, such as irritable bowel syndrome or a problem with the gallbladder, pancreatic weakness is rarely diagnosed as such.
Also read: Cholesterol Esterase - That's what it's important for!
Pancreatic weakness also often causes so-called fatty stools.
More about this topic can be found: Fat stool
Overactive pancreas - does it exist?
An overactive pancreas is an extremely rare and rarely occurring disease. Depending on the affected part of the pancreas, this leads to an excessive production of the various enzymes for digestion (in the case of exocrine hyperfunction) and of insulin (in the case of endocrine hyperfunction). The latter can manifest itself in hypoglycaemia, depending on the extent of the excessive function. This can be prevented by eating small meals regularly.
Fatty Pancreas - Why?
An fatty pancreas can develop as a result of various diseases. One of the more common and well-known causes is excessive consumption of alcohol. This leads to an acute inflammation of the pancreas. Over a long period of time, the tissue of the pancreas can be damaged and perish. In some patients this manifests itself as increased fat deposits in the pancreas.
Another possible cause of an obese pancreas is the sequelae of inflammation of another origin, i.e. inflammation caused by a cause other than excessive alcohol consumption. This can be inflammation caused by a problem with bile that causes bile to build up in the pancreas. Alternatively, certain medications, diabetes mellitus or yellowing (jaundice) caused by the liver can lead to an inflammation of the pancreas, which increases fat after the disease has healed.
Stones in the pancreas
A stone in the pancreas is usually rather rare, but all the more dangerous. This is a gallstone that can migrate into the pancreas through the joint opening of the bile ducts and the pancreatic drainage. As a result, the secretion from the pancreas cannot flow into the intestines. Instead, it builds up and instead begins to digest its own glandular tissue. It is therefore an acute, very dangerous clinical picture that manifests itself in an acute pancreatitis and should be treated as soon as possible.
Further information can be found at: Complications of inflammation of the gallbladder
Calcifications in the pancreas
Calcifications in the pancreas often occur as part of chronic inflammation. This leads to long-term changes in the glandular tissue. These include deposits of digestive secretions that are produced and released by the pancreas. If this cannot flow properly into the intestines, residues remain in the ducts, which can accumulate over a long period of time. The resulting calcifications can be seen by the doctor during an ultrasound examination, depending on the severity.
Pancreatic cancer
Pancreatic cancer is a malignant neoplasm of the pancreas.
Causes can include chronic alcohol consumption and recurring pancreatitis.
As a rule, pancreatic cancer is diagnosed very late because it causes symptoms in the patient late. As a rule, the patients do not experience any pain but complain about a dark color of the urine and a lighter color of the stool.
In some cases the skin and conjunctiva may turn yellow.
Since the pancreas is also responsible for producing insulin, it can happen that the organ is no longer able to produce enough insulin in the event of cancer.
This leads to an increase in blood sugar levels, which is often routinely diagnosed.
If a malignant neoplasm (tumor) of the pancreas is suspected, an ultrasound examination is carried out first. However, one cannot always see whether a malignant neoplasm is present.
A CT or MRI of the abdominal cavity of the pancreas can provide more reliable information about whether such a disease is present.
One can only know with certainty whether a malignant neoplasm in the pancreas is through a puncture, which is often CT-controlled. At V.a. pancreatic cancer, punctures are often not performed, as metastasis can be triggered by the puncture.
The treatment options for pancreatic cancer are rather limited. Chemotherapy can be used to try to stop the progression of the disease, and so-called Whipple surgery is often used, in which parts of the pancreas are removed.
Chances of survival:
The prognosis of healing and survival depends on the diagnosis of pancreatic cancer, especially on the stages.
So-called staging is necessary to check how far the tumor has already spread in the person's body.
The most important thing is whether the tumor has crossed the tissue of the pancreas and affected the surrounding tissue.
It is also very important to find out whether there are already distant metastases in other organs and whether the body's lymph nodes are already affected.
Depending on how this staging turns out, a longer or shorter statistical survival time can be assumed.
In oncology, prognoses and chances of survival are made with the so-called 5 year survival rate described.
It is given as a percentage and indicates how many of the average affected patients are still alive after a period of 5 years.
It says nothing about the quality of life or possible complications, only whether someone is still alive.
If the pancreatic cancer has moved beyond the organ borders and infiltrated the surrounding organs as well as has affected the lymphatic system and the bile ducts are already narrowing, a curative, i.e. curative operation decided and only applied a palliative concept.
A palliative treatment concept is not understood to be a healing approach, but rather a pain-relieving approach. In this case the disease cannot be stopped and inevitably leads to death. If such a treatment concept is chosen, the 5 year survival rate is 0%, i.e. no patient is alive after 5 years.
If a curative concept is chosen, i.e. if measures such as surgery or chemotherapy are taken, the chances of survival increase. In this case one speaks of an approximately 40% 5 year survival rate. So after 5 years, 40% of the intensively treated patients are still alive, the condition they are in is not described.
Not even how many patients are still alive after 6-10 years.
The fact that over half of the treated patients died after 5 years clearly shows how severe this disease is. There is also a mean 5-year survival rate, which shows all survival rates of a disease as an average. Since there are some treatment methods that are also used individually, the averaged prognosis is not too meaningful.
The average 5 year survival rate for pancreatic cancer is 10-15%. That means only 10-15% of the patients on average survive the disease for 5 years.
Signs:
The signs of pancreatic cancer are difficult to recognize, also because the first symptoms appear very late.
If pancreatic cancer is detected early, it is usually a matter of routine examinations, the secondary findings of which include abnormal values, e.g. in the blood count or in the ultrasound picture.
The first symptoms, which is why a doctor is usually consulted, can be back pain, which is either belt-shaped at the level of the pancreas or abdominal pain that pulls into the back.
Since these are completely unspecific symptoms, the first suspicion will probably never be pancreatic cancer, which is why valuable time can pass here too.
Mostly, however, patients come to the doctor with an unclear so-called jaundice, yellowing of the skin and conjunctiva.
Jaundice is completely painless and only indicates that there is either a problem with the blood pigment bilirubin, e.g. the liver is damaged, or if it is a problem with the drainage of bile in the bile ducts or pancreas.
In the case of jaundice, the pancreas must be examined more closely in addition to the liver.
Sometimes it happens that patients notice a suddenly sharply increased blood sugar. As a rule, these patients have diabetes mellitus and are treated accordingly with insulin. In this case, however, the pancreas should definitely be examined.
The background to this is that the pancreas produces the essential substance insulin.
If the work of the pancreas is impaired by a tumor, it can happen that too little insulin is produced and released into the blood, which can then lead to high blood sugar levels.
Since there are only a handful of correct symptoms that are not pancreatic-specific either, if these symptoms are present, these should be followed closely in order not to miss this life-threatening disease.
An important and trend-setting first symptom of a pancreatic disease is a change in the stool and abnormal urine.
The majority of those affected, whose pancreatic duct is obstructed by an inflammation or by the corresponding tumor, show a lightening of the stool. At the same time, the urine becomes darker.
The reason is that the substances released by the pancreas for digestion in order to darken the stool no longer get into the digestive tract but are excreted through the urine. Therefore the coloration does not take place in the stool but in the urine.
It is imperative that patients with these symptoms be examined more closely. Although there is not always a malignant medical history behind it, the suspicion of a disorder of the bile ducts or pancreas is very high.
Treatment:
If a treatment is chosen, it depends on whether it is a curative treatment (so a healing approach) or a palliative treatment approach (loath relieving treatment) acts.
Palliative treatment:
In palliative treatment, measures are used that do not unnecessarily weaken the patient, but at the same time have a soothing effect on him.
Most of the time, in patients receiving palliative treatment, the tumor has already affected large parts of the pancreas and the outflow of bile acids is disturbed, which leads to severe discomfort and yellowing of the skin.
Here, a small tube is usually placed in the pancreatic duct by means of an endoscopic procedure to ensure that the bile ducts can immediately drain away and actively participate in digestion again.
In the case of progressive pancreatic cancer, it is usually the case that the initially complete painless tumor infestation becomes increasingly painful the further it progresses. For this reason, an important palliative treatment concept, regardless of the type of tumor, is to ensure freedom from pain.
In most cases, highly potent painkillers are chosen, which are dosed very quickly in order to ensure freedom from pain.
Curative treatment:
If a curative, i.e. healing, treatment approach is chosen, surgical measures or combined surgical and chemotherapeutic measures are usually used.
Depending on the spread of the tumor, it may be necessary to start chemotherapy before surgery. This is usually done when the tumor is very large and chemotherapeutic shrinking would make a gentler procedure possible.
It may also be necessary to carry out chemotherapy after an operation in order to subsequently kill any remaining tumor cells.
An exclusive surgical treatment is rarely carried out.
During surgery, one tries to operate on the affected pancreas as gently as possible.
An attempt is made to leave parts of the unaffected pancreas standing so that the corresponding functions can continue to be maintained.
However, the gallbladder and parts of the stomach as well as the duodenum are almost always removed and the remaining ends joined together again. This procedure, also known as Whipple OP, is now a standardized treatment method for pancreatic cancer.
There is also a modified operation in which larger parts of the stomach are left and the result is the same as the Whipple operation.
Age:
As a rule, patients with pancreatic cancer are older. Since severe alcoholism with recurring pancreatitis are considered risk factors, it can also happen that patients of younger age are afflicted with pancreatic cancer.
In Germany, 10 people per 100,000 population develop new pancreatic cancer each year.The main age group is between 60 and 80 years.
Diagnosis:
Diagnosing pancreatic cancer is not that easy.
First of all, it is important to raise suspicions, which then have to be confirmed. If there is a suspicion of a malignant event in the pancreas, in addition to blood tests, imaging methods are also used.
In the blood, the enzymes that are produced by the pancreas are primarily determined. A sharply increased increase indicates a general disease in the pancreas. But it can also be an inflammation of this gland.
For this reason, it is important to also perform imaging. Most often, an ultrasound of the abdomen is done first, which tries to visualize the pancreas.
Large tumors that are located in the area of the gland can sometimes already be seen here.
Even if a mass is seen in the ultrasound, a computed tomography of the abdomen usually follows. Here, the suspicious area can be examined more closely, usually with contrast media.
Experienced radiologists can often guess from the CT scan whether it is a benign disease, such as a particularly pronounced inflammation, or a malignant disease.
Another important diagnostic imaging measure is the ERCP. A gastroscopy is performed and a small catheter is pushed into the bile ducts and pancreatic duct at the level of the duodenum.
A contrast agent is injected through this catheter, which is then photographed using X-rays.
It shows the pancreas with a precise gait display. Here you can see whether the gear is compressed at any point and if so by what.
Even after this, also called endoscopic retrograde cholangiopancreatography, it is not clear whether it is a malignant tumor that compresses the bile duct.
The more the suspicion of a pancreatic tumor is confirmed, the consideration must be given to taking a sample, which then finally provides information about the histological origin of the tumor.
Samples can be obtained using the ERCP described above when the tumor already extends far into the pancreatic duct or from the outside by needle puncture.
Since the pancreas is a relatively small organ surrounded by important structures, it is particularly important not to injure any of the surrounding tissues such as nerves or blood vessels.
For this reason, the puncture is mostly controlled by CT. The patient lying in a CT device is controlled from the outside and placed a needle in the area of the pancreas after the radiologist has precisely located the position of the pancreas using CT.
The procedure only takes a few minutes, the sample is minimal, but it gives the decisive indication of the origin of the tumor and the next necessary therapeutic steps.
The sample is next sent to the microbiological laboratory, where the cells are treated with a special staining process. Then the samples are examined by a pathologist and an appropriate diagnosis is made.
So-called false positive results, i.e. that a cancer is seen but in reality a benign neoplasm is present, only occur if the sample was mixed up.
A false negative finding, i.e. that the pathologist does not see any malignant tumor tissue, although it is a cancerous case, can be more common.
Mostly it is because the biopsy, which was carried out precisely and CT-controlled, and caught parts of the pancreas, penetrated exactly next to the malignant cells and therefore only caught benign cells. The pathologist then only sees benign cells under his microscope. Should the microscopic findings contradict the image in the CT (typical CT image but normal microscopic findings) should be considered to repeat the biopsy.
Read more about the topics here Pancreatic cancer and biopsy
Pancreatic removal
One of the last treatment options for malignant neoplasms in the pancreas is a total pancreatic removal.
Since the pancreas is also tied to many organs, it is necessary that the organs be properly re-tied.
The stomach is usually made smaller and connected to the small intestine. The duodenum and the gallbladder are usually completely removed with a total pancreas removal.
If parts of the pancreas are still present, the bile duct system must be connected with so-called switched-off small intestinal loops.
Total pancreatic removal is associated with many risks, intensive follow-up treatment of the patient is necessary, pancreatic enzymes must be administered to the patient at regular intervals.

Depiction of the pancreas and gallbladder
- Gallbladder (green)
- Pancreatic cancer (purple)
- Pancreatic duct (yellow)
- Pancreatic head (blue)
- Pancreatic body (Copus pancreaticus) (blue)
- Tail of the pancreas (blue)
- Bile duct (Cystic duct) (green)
Diseases of the pancreas from alcohol
One of the most common diseases of the pancreas is caused by alcohol.
The so-called pancreatitis, also called Pancreatitis is a common and potentially dangerous comorbidity in severe alcoholism. Because alcohol attacks the cells of the pancreas, both chronic excessive alcohol consumption and acute alcohol consumption that occurs excessively are a great risk of pancreatitis.
A characteristic symptom of pancreatitis is a belt-shaped pain that begins slightly above the navel. The pain character is described as oppressive and extremely uncomfortable. As a rule, questioning the patient about alcohol consumption leads to a suspected diagnosis of pancreatitis.
The physical examination reveals that the abdomen is tender and the patient is in poor general condition. An ultrasound of the abdomen and, in cases of doubt, a CT of the abdomen are available as imaging methods. With inflammation of the pancreas there is often a distended pancreas, often with inflammatory fluid. The patient's laboratory is also conspicuous and usually shows high levels of inflammation and elevated lipase levels.
Consistent abstinence from alcohol is very important for treatment, and there are also some antibiotics available that can be given to the patient.
Pancreas and diet

The pancreas is an exocrine, that is, enzyme-producing organ. It is of particular importance in the utilization of food.
The so-called beta cells, with which the pancreas is permeated, produce the essential insulin. As soon as sugar is supplied to the body, these cells release insulin, which then transports the excess sugar from the blood into the cells and thus ensures that the body does not suffer from excess sugar. The pancreas also produces what is known as lipase, which is necessary for breaking down fat.
In the case of numerous diseases of the pancreas, corresponding changes in diet can have a positive effect on the disease of the pancreas. In acute pancreatitis (acute inflammation of the pancreas) should be at least for 24 hours consistent food abstinence is observed. After that, the gradual build-up of food can begin again. However, the food consumed should only be extremely low in or fat free. More fatty things can then be eaten bit by bit. In principle, however, you should live low-fat after a pancreatitis. Margarine should be eaten instead of butter, rather low-fat fish instead of meat, and fried foods should be avoided.
Pancreatic disease and diarrhea
There are some pancreatic disorders that can also be accompanied by diarrhea. Is an infectious cause (Gastrointestinal infection) has been ruled out as a cause, the pancreas should be examined more closely. It could be that the cause of the diarrhea is a so-called exocrine pancreatic insufficiency. In doing so, the pancreas is not able to produce a sufficient amount of various digestive enzymes. After eating, the intestine reacts with flatulence and diarrhea; sometimes those affected also have abdominal pain and complain of so-called fatty stools.
For diagnosis, the corresponding enzymes that are responsible for exocrine pancreatic insufficiency are quantitatively determined by a gastroenterologist. To treat this disease, either diet changes or the ingestion of the insufficiently formed enzymes can be used.















.jpg)







-mit-ten-(titanic-elastic-nail)-oder-sten.jpg)
