The most common sores in the mouth
introduction
An inflammation in the mouth is extremely painful in most cases and is a major problem when eating and drinking. It can have many different causes and manifest itself in different clinical pictures.
Here is an overview of the most common inflammations of the mouth.

Inflammation of the lining of the mouth
Canker sores
Aphthae are small, rounded erosions of the mucous membrane (Mucosal injuries) on the oral mucosa, but they can also appear on the tongue.
The defects that look like ulcers show a whitish or yellowish surface with a crimson border. This typical appearance makes diagnosis easy.
Aphthae in the mouth are extremely painful, especially with the presence of acids.
Read more about this at: Aphthae - causes & therapy
Vesicles in the mouth
Mouth blisters can appear on the lip, tongue or cheek mucosa. Especially in children, blisters can form in the mouth as part of a fever attack. Blisters can also appear in the mouth as a result of burns, herpes or canker sores. They are usually extremely painful, but heal within a few days.
Learn more at: Vesicles in the mouth
Mouth rot
Oral rot (also known as herpetic gingivostomatitis) is an inflammatory change in the lining of the mouth caused by a herpes simplex virus infection. It usually occurs in children within the first 3 years of life and is extremely painful. But adults can also be affected.
Read more at: Mouth rot
Inflammation of the cheek
Inflammation on the cheek can either originate from the inside of the oral cavity or it can arise from the outside.
If you bite your cheek or if sharp edges of a defective crown or prosthesis irritate the lining of the cheek, then a painful inflammation develops at this point. But also an inflammation of the duct of the parotid gland radiates into the cheek.
Find out more at: Inflammation of the cheek
Inflammation of the salivary glands
Of the three large salivary glands, only the largest, the parotid, is not located in the oral cavity. If the glandular tissue or one of the ducts becomes inflamed, dry mouth, pain, and difficulty chewing and / or swallowing occur. In the case of a purulent inflammation of the salivary gland, taste disturbances may occur because the pus empties into the mouth.
Read on under: Inflammation of the salivary glands
Inflammation on and around the tooth
Tooth pulp inflammation
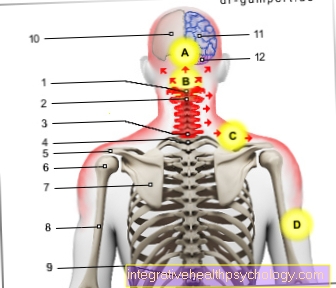
If the pulp becomes inflamed either from deep caries or from periodontal disease, in most cases this leads to extremely severe pain, which can radiate into the whole jaw and also to the temples. Without treatment, the inflammation continues and the tooth nerve dies, so root canal treatment is necessary.
More about this at: Tooth pulp inflammation
Inflammation of the wisdom tooth
Very few people today have created all 4 wisdom teeth and those who are there usually do not or only half break through into the oral cavity. A wisdom tooth that has not fully erupted is covered by a cap that can hardly be cleaned and quickly becomes inflamed.
But I can also inflame a wisdom tooth that is still completely resting in the bone and develop cysts.
Learn more at: Inflamed wisdom tooth
Root inflammation
Tooth root inflammation occurs either as a result of an inflammation of the tooth pulp (i.e. the pulp) spreading to the root tip or because the tissue of the tooth holding apparatus is bacterially infected and can thus spread to the root tip.
Typical symptoms of a tooth root inflammation are knocking pain or pain, especially when biting.
If the inflammatory process is not stopped, a fistula or abscess can form.
Read more at: Abscess on the tooth
Inflammation on the neck of the tooth
A tooth neck infection is also popularly referred to as pain-sensitive teeth / tooth necks. The gums are usually in direct contact with the crown of the tooth so that the neck of the tooth is hidden under the gums.
If the gums recede, however, then dentin or root cement is exposed. These substances are not a sufficient blockade for warmth or cold stimuli, so that there are brief pulling pains when eating. The constant irritation of the tooth nerve can also lead to inflammation, i.e. H. pulpitis develops.
Learn more about it at: Inflammation of the neck of the tooth
Gingivitis - inflammation of the gums
If the gums that are next to the tooth become inflamed, then gingivitis is present. As a rule, oral hygiene that has been neglected for 48 hours leads to inflammation of the gums, which is noticeable through sensitivity to pain, bleeding gums and swelling.
As soon as the causes of the inflammation are removed (i.e. plaque, food particles and bacteria), the gums can heal again.
Read on below: Inflammation of the gums
Periodontitis - inflammation of the periodontium
As soon as chronic inflammation of the gums progresses untreated, the inflammatory cells can spread to the jawbone. Bone loss occurs and the gums recede.
Plaque and tartar on the root surface, i.e. under the gums, also lead to periodontosis (correct term: periodontitis). Overall, the teeth holding apparatus is irreversibly weakened, so that the affected teeth can become loose and fall out because once the jawbone has broken down, it does not come back.
Find out more at: Periodontal disease - causes, symptoms, treatment
Inflammation after surgery on the tooth
Inflammation after tooth extraction- alveolitis sicca
When a tooth has been extracted, a complicated wound is initially left behind. Bones, gums, and soft tissue must regenerate in order for the wound to close. The blood plug remaining in the alveolus (the tooth socket) is important for complication-free wound healing. Without the blood cells, the wound does not heal, it dries out, so that only the bone compartment remains and becomes inflamed. The resulting inflammation of the bone is extremely painful and can spread all over the jaw.
Find out more at: Alveolitis sicca
Inflammation after a wisdom tooth operation
In principle, the same rules apply to wound healing after the removal of wisdom teeth as to other extracted teeth.
Because the wisdom teeth are mostly half or completely in the bone, a more complex operation is necessary, which means that the wound area is larger. Accordingly, the wound can become infected and become inflamed more quickly. The seams in particular create niches for dirt for food residues and bacteria.
The dentist can follow the wound healing through follow-up and check-up appointments and, if necessary, intervene in good time.
Read on under: Inflammation after a wisdom tooth operation
Inflammation after apicectomy
Because the apicectomy is a surgical procedure, like any operation, it also involves various risks. These include, for example, renewed inflammation due to inflammation foci not being completely removed or inflammation of the wound area due to wound healing disorders.
Sometimes pus forms, which is encapsulated in the tissue to protect the rest of the organism from the spreading inflammation. This process is usually very painful and is known as an abscess. In this case, an antibiotic must usually be taken.
Learn more at: Inflammation after apicectomy
Inflammation around the mouth
Swollen cheek
If the cheek is thick, the cause is usually an abscess of the back teeth. An abscess is a collection of pus in tissue caused by inflammation. Because of the inflammation, the tissue swells up and is displaced outwards, so that sometimes even the eye swells or breathing difficulties occur because the throat is narrowed by the swelling.
Read more on the topic: Abscess on the tooth
Therefore, the supposedly harmless fat cheek should not be joked with. A doctor's visit is strongly recommended.
Read on under: thick jaw
Inflammation at the corner of the mouth
An inflamed corner of the mouth is usually a painful symptom that can occur with various diseases. This is perceived as painful, especially when it comes into contact with saliva or other liquids. The most common cause of torn and then inflamed corners of the mouth is dry room air. In these cases, remedial action can easily be found. However, if the symptoms do not go away or occur frequently, it is necessary to seek medical advice in order to be able to rule out any serious illnesses that are behind the inflammation.
Read more under: Inflammation in the corner of the mouth
Inflammation on the dentures
Inflammation under a crown
The older an artificial dental crown made of plastic, metal or ceramic, the higher the probability that the edge has become leaky. Bacteria can get under the crown and caries can develop, as well as inflammation of the dental pulp.
But even a new crown can lead to pain, because grinding the tooth for a crown can irritate the tooth nerve, causing it to become inflamed. If the new crown is too high, the increased pressure when chewing can inflame the tissue around the affected tooth.
Read more about it under: Inflammation under the tooth crown
Stomatitis - inflammation of the lining of the mouth
Stomatitis is inflammation of the lining of the mouth. However, it can also occur in the context of other primary diseases or as a side effect of certain therapies, such as chemotherapy. If the gingiva (gums) is involved, one speaks of gingivostomatitis.
Symptoms of oral mucosal inflammation, as with any inflammation, are pain, redness, and swelling. Other signs of inflammation include bleeding, itching, and burning. These stimuli stimulate saliva production, which is why an enormously increased saliva flow rate can also indicate inflammation.
The main causes are pathogens that enter the tissue through small defects in the mucous membrane. These microtraumas can be caused by spicy, crunchy or pointed food. Since the mouth is full of bacteria, such a small injury is always followed by a small inflammation. If there is a lack of oral hygiene or diseases such as oral rot, there are more pathogens in the mouth, which favors a stronger and more painful inflammation. To prevent inflammation, it is therefore advisable to thoroughly clean your teeth and mouth with an antibacterial mouth rinse.
Read more on the topic: Oral rot in the adult
Causes of stomatitis
There are a few different causes that can cause this inflammation in the mouth. Most of the time, the inflammation is caused by inflammation of the gums. This can be due to poor dental or oral hygiene or dehydration.
But also microorganisms such as viruses, bacteria, fungi and protozoa can infect the oral mucosa and thus trigger stomatitis.
Read more about this under the topic: Vesicles in the mouth
Wearing a denture can be an additional risk factor, as inadequate denture care can also cause inflammation.
Alcohol and nicotine abuse as well as deficiency symptoms (including vitamins A, B, C; iron deficiency; scurvy) also favor stomatitis.
Allergies, immune deficiencies, and excessive oral hygiene can also be the triggers.
Finally, as already indicated in the introduction, stomatitis can occur as part of chemotherapy. The drugs administered damage the oral mucosa and sometimes also lead to more or less severe immunosuppression.
Symptoms of oral mucosal inflammation
The symptoms of stomatitis are typical of an inflammation in the mouth. There will be redness and swelling in the mouth. It hurts, especially when eating, so that small children in particular refuse to eat completely. In addition, those affected have bad breath and show increased salivation (hypersalivation).
Ultimately, it comes to ulceration, easy bleeding in the mouth and bleeding gums.
Stomatitis therapy
Therapy for stomatitis depends on the underlying cause.
Good oral and dental hygiene is also particularly important. Dentures can be cleaned with special denture brushes.
In the case of bacterial infections, antibiotics are used, in the case of a viral cause with antivirals and in the case of a fungal infection with antimycotics.
Gargling with ratanhia tincture can have an anti-inflammatory effect on inflammation in the mouth and throat and thus contribute to recovery. The tincture is obtained from the root of the rattan shrub.
Dynexan® oral gel can be applied to the affected areas for pain relief.
Inflammation in the corner of the mouth
Reasons for torn corners of the mouth can be, for example, extreme air temperatures, different humidity or constant irritation of the corners of the mouth with the tongue and teeth. The lips become chapped by very cold and also very hot air temperatures. It is the same in a dry room. It is therefore important to provide the lips with sufficient moisture through adequate hydration.
Irritation of the sensitive skin on the lips leads to minor injuries and thus promotes inflammation. Such irritation is caused by spicy food, a lack of vitamins, or allergies. A hormonal change also increases the sensitivity of the skin.
Inflammation in the corner of the mouth occurs because bacteria or viruses can enter through these small cracks and cause inflammation. These so-called Angular rhinitis are not in themselves a dangerous disease. But if other symptoms occur at the same time, you should contact a doctor to rule out more serious problems and causes.
Inflammation in the corner of the mouth is treated with creams and ointments to grease the lips to prevent tearing. Depending on the severity of the inflammation, these may also contain an antibiotic or an antiviral substance. In the case of contact allergies, for example from a costume jewelery piercing, it is of course sensible to remove it.
Inflammation of the salivary gland
There are many salivary glands in the mouth. In addition to the three large glands (submaxillary gland, sublingual gland and parotid gland), there are many small glands that are located throughout the tongue and mouth. The most commonly affected gland is the parotid gland (Parotid). In addition to redness and pain, inflammation also includes swelling. When pressure is applied to the bulging area, there is therefore more pain.
The causes of inflammation of the salivary glands are bacteria and viruses, which lead to inflammation, especially in a weakened immune system. The reason for an immune system weakness, in turn, can have many reasons. There are diseases such as mumps, Epstein-Barr virus or influenza viruses. In the case of alcohol abuse, tumors or stones, the drainage path of the saliva is prevented, which offers the pathogens a "perfect" environment.
The bacteria are not washed out of the gland due to reduced salivation, for example due to poor nutrition, radiation or anxiety. A lack of saliva thus also promotes the development of inflammation.
Inflammation in the mouth from dentures
If you have been wearing the denture for a long time, it should not actually cause any inflammation. Unless the bacteria are brought into the mouth via the dentures. With thorough care and storage, however, no bacteria that could cause inflammation should get on the plastic prosthesis.
If the prosthesis remains in the mouth for too long and the oral mucosa under the prosthesis is not cleaned, this area offers the bacteria the best environment to grow. Warm and humid, and constantly new nutrients that are ingested through food. This allows the bacteria to multiply easily and inflame the underlying gums.
This is bad insofar as inflammation causes pain and weakens the body and the immune system as a whole, and on the other hand, the bones can become infected even if not treated. Despite the therapy, the prosthesis would no longer fit and a new one would have to be made.
Aphtous stomatitis
Synonyms of aphtous stomatitis are Aphthous stomatitis, Herpetic gingivostomatitisHerpes gingivostomatitis, Herpetic somatitis or mouth rot.
Causes of aphthous stomatitis
This form of inflammation in the mouth is caused by an initial infection with the herpes simplex virus type 1. This inflammation of the lining of the mouth mainly affects children aged 1 to 3 years. Adults are only affected in isolated cases.
The type 1 herpes virus is carried by about 95% of people without becoming ill. It manifests as a disease when the immune system is attacked, for example in the context of a flu. Children can easily get infected with other children in the crèche or with their parents.
You can find more about aphthous stomatitis in the main article: Mouth rot
Symptoms of aphthous inflammation of the oral mucosa
The incubation period until the onset of the disease is around 3 to 7 days.
The infection manifests itself in a very pronounced inflammation of the lining of the mouth and throat. Blisters form, which also burst in the course and have a bloody blister base. They are extremely painful that the children refuse to eat.
The papillae of the tongue appear as small white dots. The gums are also inflamed and very red. Also typical is a very sour, unpleasant bad breath and increased salivation.
This is accompanied by a fever and swelling of the lymph nodes in the area, which is also painful.
Therapy of inflammation in the mouth
The prognosis for immunocompetent children is usually very good. The inflammation in the mouth heals without scarring within a week.
A causal therapy, which is based on the causes, is usually not necessary, so that a symptom-oriented treatment is completely sufficient. Antipyretic drugs such as ibuprofen are recommended. These are also pain relievers. Local anesthetic oral gels and solutions are also used to relieve pain in the mouth and make it easier for children to eat. These usually contain lidocaine. Read about this: Dynexan® oral gel.
It is also advisable to consume chilled, soft foods such as Milk, yogurt, vegetable puree and rice. Spicy and acidic foods should be avoided. In the case of very severe disease courses, causal therapy with the antiviral acyclovir can be carried out.
Candidiasis - fungal infection in the mouth
Candidiasis is generally understood to be an infectious disease caused by fungi of the Candida genus. Oral thrush (also Candidomycetica stomatitis called) is a candidiasis of the mouth and possibly the pharynx.
Read more on this topic at: Candidiasis.
Causes of Candidiasis
The oral thrush is mostly caused by the fungus Candida albicans caused. This fungus is a harmless saprophyte in the mucous membrane of the mouth and throat and does not cause any disease in healthy people.
In the case of congenital or acquired immunosuppression (e.g. due to HIV, antibiotics, cytostatics or sepsis), the fungus can be infectious and attack the mucous membranes, which is then expressed as an inflammation in the mouth.
Diagnosis of the fungal infection
The diagnosis is made microscopically with the help of a smear of the mucous membrane. However, in order to initiate adequate therapy, the fungus still has to be grown in a culture. Then the diagnosis is certain.
Candidiasis Therapy
Candidiasis of the mucous membrane of the mouth and throat is treated with antimycotics such as econazole, nystatin, amphotericin B, natamycin or miconazole. These are applied locally.
Disinfecting mouthwashes and cleaning agents such as gels are also available.
It is also important to eliminate the cause. If the candidiasis developed, for example, as a result of antibiotic treatment, the antibiotic should be discontinued or changed.
Read more about this under: Means against fungal diseases.
Habitual canker sores
This is an inflammation in the mouth that very often recurs. The disease is very painful and non-infectious. It is estimated that up to 25% of the total population suffer from these recurrent canker sores.
Causes of habitual canker sores
Many different causes are discussed in connection with the development of habitual canker sores. It is therefore assumed that habitual canker sores are the manifestation of very different underlying clinical pictures.
Possible allergies, food intolerances (e.g. nuts and citrus fruits), deficiency symptoms (vitamin B12, iron, folic acid) and minor trauma caused by biting the lining of the mouth and cheek.
In addition, immunological reactions seem to play a role, which occur, for example, in the context of Behçet's disease.
Virus infections also seem to be involved, as the cytomegalovirus can be partially detected in the canker sores. This virus belongs to the herpes virus family.
Finally, intolerance to components of the toothpaste are also a possible cause.
Read more about this under: Aphthae - what causes the painful sores?
Symptoms of habitual apthens
The canker sores appear as sharp, oval swellings that are delimited by a red border and appear whitish. They can be up to 2 cm in size and usually heal without scars within 2 weeks. These canker sores are mainly located on the inside of the lips and cheek mucosa. It can also cause canker sores on the tongue and canker sores in the throat.
Therapy of habitual canker sores
In the treatment of canker sores there are different approaches that are more or less successful.
First of all, avoiding potentially intolerable foods like nuts can improve the situation.
Antibiotic pastes and mouthwashes (e.g. tetracycline and chlortetracycline) can shorten the duration of the illness. Antiseptic and local anesthetic mouthwashes can be used to relieve the symptoms of an inflammation in the mouth, but this does not reduce the duration of the illness. Anti-inflammatory gels and pastes containing corticosteroids are also used.
Finally, if the course is very resistant to therapy, systemic therapy, etc. with colchicine, dapsone, doxycycline and thalidomide.
Read more about this under: Canker sores - different options of treatment.
Home remedies for mouth sores
Also different Home remedies can help with an inflammation in the mouth.
For example, can Douches With Camomile tea or can be used with lemon water. Also Sage tea can be used for douching. However, the taste is not necessarily pleasant, especially for children. You can also rinse with a pure salt water solution. It should only be ensured that the salt water is not swallowed.
Since canker sores are very sensitive to acidic foods, in the case of canker sores from Rinsing with lemon water is not recommended.
Also honey has an antibacterial effect and is therefore easy to suck. However, honey should not with fungal attack be used because it can provide the mushrooms with new food and thus support them in their growth.
Home remedies should always Applied for a limited time only and if there is no improvement in the inflammation in the mouth, the Go to the dentist in order to ensure a targeted, professional therapy.
Homeopathy for mouth inflammation
- Borax, also called tinkal or sodium borate, is a salt that not only relieves skin inflammation but also inflammation in the mouth. It rarely occurs in nature. With a daily dose of 3 globules Mercurius solubilis C5 and 3 globules Borax C5, the canker sores can be treated.
- Otherwise, the homeopathic Borax C9 is the basic treatment. 5 globules are taken every 2 hours.
- Homeopathy beads are particularly suitable for children. In addition, they are not painful; in contrast to other questionable home remedies such as hard liquor
Caution: the effect of globules is reduced by essential oils. This includes, for example, camphor, chamomile or peppermint. For this reason, there should be an interval of half an hour between ingesting the oils and the globules.








.jpg)