electrocardiogram
Definition / introduction
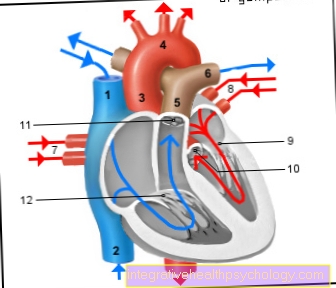
The EKG (= electrocardiogram) records the sum of the electrical voltages of all heart muscle fibers and is therefore used to assess the heart muscle function.
In addition to the heart rhythm and heart rate, malfunctions of individual sections of the heart muscle can also be detected. Every cardiac action is preceded by an electrical excitation, which usually begins in the sinus node. From here the excitation spreads over all cells of the heart muscle according to a known scheme.
This creates a recurring picture of the heart's action, and changes in this picture allow conclusions to be drawn about possible malfunctions.
The EKG is increasingly being evaluated by computer programs. Nevertheless, the manual evaluation by the doctor is still not dispensable today.

function
The EKG is a non-invasive, repeatable method for assessing the Cardiac functionon.
Next rhythm, Heart rate and Location type the function of the Atria- and - chambers read off.
It is possible through that EKG one Heart attack, one A.V-block, Arrhythmia or one hypertrophy of the myocardium (thickening of the heart muscle). You can also Inflammation of the Heart sac (Pericarditis), of Heart muscle (M.yocarditis) and Electrolyte imbalances can be recognized by a changed ECG image.
execution

Basically, the electrocardiogram is one of the Routine examinations; almost every general practitioner or Cardiologist, and every hospital is able to perform an EKG. Furthermore, the investigation is perfect painless and usually causes no problems whatsoever.
First, the patient lies down with them fully stripped torso, as well as without shoes and stockings, relaxed on a lounger. It is important to find the most comfortable and relaxed position possible, as muscle tension can lead to a falsified ECG. It is also important to avoid muscle tremors, for example due to excitement or cold.
In the next step, the medical support staff bring about ten electrodes on the upper body as well as the arms and ankles on. Under certain circumstances, the chest hair of very hairy men must be shaved, as otherwise the conductivity may be restricted. In contrast to the adhesive electrodes on the upper body, so-called clamp electrodes are used on the arms and legs. Then the appropriate cables are attached to the individual electrodes and connected to the ECG device.
Now the patient should lie as quietly as possible; Movements, coughing, hiccups, but also particularly deep inhalations can falsify the result. Diseases that cause involuntary tremors, such as Parkinson's disease, should therefore be taken into account when interpreting the ECG.
The devices write within at the push of a button less minutes an electrocardiogram. In some cases, the procedure must be repeated if, for example, electrodes are not optimally positioned or the skin contact is insufficient.
After a meaningful EKG has been written, medical personnel remove the electrodes and cables. As a rule, the adhesive electrodes can be easily removed and hardly cause any skin irritation.
Invest
In order to get a meaningful EKG, some things have to be considered when applying the electrodes. To better conductivity they are often done water or Disinfectants moisturizes.
As a rule, the Electrodes on both forearms, as well as both Ankles created; then the positioning of the six chest wall electrodes. Nowadays it is common Adhesive electrodes utilized. In older hospitals or medical practices, so-called suction electrodes are still used, which are automatically sucked onto the patient's skin.
For the sake of standardization, each of the six chest wall electrodes has a name:
- V1: to the right of the breastbone in the 4th intercostal space
- V2: left of the breastbone in the 4th intercostal space
- V3: between V2 and V4
- V4: on the left at the intersection of the 5th intercostal space and the mid-clavicle line
- V5: front axle line same height as V4
- V6: middle axis line, same height as V4
physiological background
Our Heartbeat, but also every other muscle movement, is based on the targeted displacement of charged particles (Ions). They flow between the inside and outside of the cell and thus cause electrical potentials. So ultimately it works every pumping action of the heart, such a electrical excitation ahead. But how can the electrocardiogram be explained?
Starting from the pacemaker center of the heart, the Sinus node, the excitation (depolarization) runs at a speed of about 1m / s in the direction of the heart muscle cells.
Now, in simplified terms, imagine that the excitement a heart muscle cell positively charged particles (Cations) of the Cell surface in the interior the cell flow. Compared to still unexcited neighboring cell, the excited cell is at hers Surface now negative loaded. This creates a so-called charge difference electric dipole. A dipole is understood to mean two opposite poles with the same charge (e.g. +1 and -1), one of which is electric field goes out.
The excitement and with it that too electric field spread over the various structures of the heart in one orderly wave. Finally, the excitations of the individual heart muscle cells add up so that they can be recorded by the sensitive electrodes on the body surface.
Through the specific timing the excitation (first the atria, then the ventricles, etc.) creates the typical wave and jagged pattern of an electrocardiogram.
EKG leads and location types
Derivatives
There is one in our heart permanent flow of differently charged particles (ions). This redistribution in turn creates various electrical potentials. These “electrical heart currents” can be measured from different perspectives and levels through individual leads. Combined, the derivations provide a comprehensive picture of the condition of the heart muscle and its conduction system.
Usually comes in Germany 12-lead ECG is used, which can register twelve leads simultaneously. These include:
1) Einthoven derivation (Frontal plane): It belongs to the classic bipolar limb lead, because the voltage between two arm or leg electrodes with equal rights is determined.
One differentiates:
- Derivation I. between right and left arm,
- Derivation II between right arm and left leg and
- Derivation III between left arm and left leg.
2) Goldberger derivation (Frontal plane): In this limb lead two electrodes of the Einthoven leads via a resistance to a single indifferent electrode, a kind of electrical "zero point", interconnected. This creates leads between the zero point and the remaining electrode.
They are called
- Derivation aVR between the right arm and the interconnected electrodes on the left arm and left leg,
- Derivation aVL. between the left arm and the interconnected electrodes of the right arm and left leg and
- Derivation aVF between the left foot and both arm leads.
3) Wilson derivative (Horizontal plane): In contrast to the two previous leads, the six electrodes on the chest wall are used here. you will be V1-V6 called.
If certain pathological events are suspected, such as an infarction of the back wall of the heart, additional leads can be made using additional electrodes.
Location types
The medical professional understands the type of location to be vector of the electrical heart axiswhich can be determined in the ECG with the help of the Cabrera circle.
The electrical heart axis is very much dependent on the Location of the heart in the body and the Heart muscle mass certainly. Therefore, determining the type of location is an important aspect of EKG analysis. A distinction is made between the following location types:
Link type
This is the most common type of location heart-healthy adults over 40 years. The type of position can also be observed when the left half of the heart is enlarged (left heart hypertrophy) in the context of high blood pressure, for example. Pregnant women also sometimes have a link type.
Indifference type
At young adults with healthy hearts the most common type of location; therefore it is also called the "normal type".
Steep type
Occurring at Children, adolescents and very slim people. It can be disease value in the context of for example one Emphysema exhibit.
Legal type
Come on healthy young children, very slim adults and deep inhalation in front. Also observable in the context of congenital heart defects or enlargement of the right half of the heart (right heart hypertrophy).
Overturned left type or right type
Have always disease value, for example with congenital heart defects or heart attacks.
Evaluation / interpretation
After recording the electrocardiogram, the interprets doctor partly using a ruler standardized for this purpose, the EKG. He analyzes the Height of the individual deflections, the time intervals to each other, as well as theirs Duration and Steepness. Correct evaluation of the ECG can make pathological processes and changes such as infarcts or arrhythmias in the heart visible. Nowadays, modern computer programs in many places analyze the written EKG in a few seconds. However, it is essential that a doctor also personally undertakes the interpretation, as the devices may overlook or misinterpret pathological changes.
The EKG is recorded on graph paper or electronically.
As a rule, the writing speed corresponds to 50 mm / s and the deflection 10 mm / mV. 1mm corresponds to 0.02s in the writing direction and 0.1mV upwards.
Since that EKG records the excitation of the individual heart muscle cells, the standard ECG contains various waves and spikes, as well as their intervals, which represent signs of a certain excitation or its regression:
- The P wave represents the atrial excitation through the sinus node, usually represented by the first small, positive wave starting from the zero line; it should last a maximum of 0.12 seconds.
- Of the QRS complex represents the physiological spread of the excitation over the chamber, which should take a maximum of 0.10 seconds. It shows itself in the form of:
- Q wave as the first negative rash, the
- R-point as a subsequent positive rash and the
- S-point in the form of the second negative rash.
- The QRS complex is followed by the relatively broad one T-wave: This marks the regression of excitation in the heart chambers. In some cases a U-wave can occur after the T-wave.
- The U-wave corresponds to post-fluctuations in the regression of excitation, although their origin has not yet been finally clarified. It is assumed on the one hand that it reflects the repolarization in the excitation conduction system (Purkinje fibers), other sources assume that it is, for example, in electrolyte disorders, such as a Potassium deficiency can occur.
In addition to the waves and spikes, certain functions can also be assigned to the sections in between:
- The PQ interval represents the distance between the start of the P wave and the start of the Q wave and should not be longer than 0.2 seconds and should be isoelectric, i.e. on the zero line. This interval is an expression of the transfer time between Atrial excitation and Ventricular excitation.
- The QT interval (also QT time) is the distance between the beginning of the Q spike and the beginning of the T wave and represents the duration of the entire ventricular excitation. This time can fluctuate depending on the current heart rate, which is why there is no standard value.
- The ST segment includes the end of the S wave up to the beginning of the T wave and marks the regression of excitation (repolarization). As a rule, it is on the isoelectric line and should not be raised above 0.2 mV. However, their duration varies considerably and depends, among other things, on the heart rate.
Please also read our page Recognizing arrhythmias.
Other recording methods

Depending on the question, different methods can be used EKG lead can be used.
That happens most often Resting ECG for use.
Usually the patient lies still, but it can also be done while sitting. Since it only takes a few seconds, it can also be used in an emergency. In addition, it is very meaningful and is therefore used most often. However, it is only a snapshot, so rarely occurring Arrhythmia may not be recorded.
In order to recognize this, the Long-term ECG used. This is recorded over 24 hours using a portable EKG device. The patient should move normally and usually follow a normal daily routine in order to be able to recognize possible situation-dependent changes. The long-term ECG is usually used for Rhythm diagnostics used.
The Exercise ECG (Ergometry) is used to record possible load-dependent Arrhythmia. The patient is defined using a treadmill or Ergometry burdened what Heart rate and Blood pressure can be observed under stress. You can also Arousal regression disorders provoked and recorded.
Electrocardiogram diagnostics
Due to the precisely defined generation and regression of excitation, deviations in the individual waves and intervals can be traced back very specifically to malfunctions.
By observing the individual P waves, their regularity and frequency, conclusions can be drawn about the heart rhythm. A normal sinus rhythm is present when the P waves are regular and positive in leads II and III, the PP intervals are uniform and each P wave is followed by a QRS complex.
The normal heart rate in adults is between 60 and 100 beats / min. A higher heart rate is called tachycardia, and slower than normal frequencies are called bradycardia.
Blockages of the conduction from atrium to ventricle are shown by prolonged PQ intervals or the absence of QRS complexes.
If the PQ time is abnormally prolonged, there is AV block; if a QRS complex follows each P-wave, conduction is delayed. This means that the excitation from the atrium to the ventricle is prolonged, but still occurs regularly with every excitation.
This corresponds to an AV block I ° (atrio-ventricular block; atrium = atrium, ventricle = chamber).
If a QRS complex no longer follows each P wave, one speaks of AV block II °. This is again differentiated into 2 types:
- Type 1 (Type Wenckebach) means that the distance between the P wave and the QRS complex increases with each excitation until the conduction fails completely. Then the period starts all over again.
- The type 2 (Mobitz type) leads to a sudden blockage of the atrial excitation on the ventricle without the interval having been extended beforehand.
Several atrial excitations can be blocked in this way. The most dangerous form is AV block III °. The conduction of excitation from the atrium to the ventricle is completely absent. This means that the P wave is no longer followed by a QRS complex. A further heart function is only possible if a replacement system is formed by the heart. This is shown by independently occurring P waves and QRS complexes.
By assessing the chamber complex or the regression of excitation, conclusions can be drawn about signs of ischemia (insufficient oxygen or nutrient supply) or electrolyte disturbances. If the ST interval> 0.2 mV on the anterior wall is positive in two adjacent leads, then one speaks in medicine of an ST elevation myocardial infarction (STEMI), i.e. a heart attack, an insufficient supply of oxygen in a certain area of the heart muscle. However, heart attacks are also possible without the ST segment elevation (Non- STEMI = NSTEMI). Angina pectoris manifests itself as a lowering of the ST segment.
Read more about this on our website Diagnosing a heart attack.
Electrolyte disturbances, especially changes in potassium, such as hypokalemia, can be represented by the formation of a further wave following the T wave (so-called. U-wave). It is a sign of delayed arousal regression. Hyperkalemia is manifested by an increased T wave and a broadened QRS complex.
A zero line (permanent isoelectric line) is created when there is no potential difference between two derivation points. It is a sign of asystole (cardiovascular arrest).
Conduction disorders can be assessed by looking at the baseline:
- Atrial flutter is shown by a typical sawtooth-like pattern of the baseline,
- Atrial fibrillation shows up in a slight sawtooth-like pattern on the baseline. The QRS complexes are random and not rhythmic, the P wave is absent.
In addition to assessing the cardiac excitation, the type of position of the heart can also be determined using the electrocardiogram.On the one hand, this describes the position of the heart in the chest, and on the other, individual thickenings of the wall, for example due to increased stress or inflammation. The position is determined by the course of the excitation from the heart base to the heart tip and can be determined with the help of the Cabrera circle. While a steep or left type is physiological, a right type can indicate a pulmonary embolism due to the increased acute stress. The type of position allows the size and position of the heart to be assessed in the chest and can be an indication of serious cardiac diseases.
Another option for examining the heart is the so-called swallowing echo, in which an ultrasound head is swallowed and the close proximity of the esophagus to the heart allows the functioning of the heart to be assessed.
Summary
The EKG represents a simple, fast and non-invasive way of diagnosing serious and life-threatening diseases.
Especially those Cardiac arrhythmias and the Heart attack can be done using the EKG good and quick recognize and the suspicion of these diseases always leads to the derivation of an EKG.
However, since the ECG can also quickly and easily rule out possible cardiac causes of symptoms, an ECG is recorded for almost every patient today. Since there is no need for complex technology, an EKG is easy to transport and can also be recorded on site, for example to directly detect a possible heart attack. However, due to the very diverse and distinct diagnostic possibilities of an EKG, it is all the more so harder to interpret this correctly and to correctly recognize the many different deviations from the norm.