Inflammation in the abdomen
General
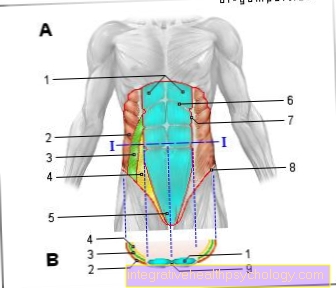
The term “abdomen” is used in medicine to describe an anatomical region that is filled by many important organs and structures. In women, these include the ovaries (Ovary) and the fallopian tubes (Tuba uterina / Salpinx). Ovaries and fallopian tubes are combined as appendages (Adnexa / Adnexa) designated. The uterus also belongs to the female abdomen (uterus) and the vagina (vagina).

All of these organs mentioned can be potential locations for inflammation in the abdomen. For one thing, the ovary and fallopian tubes can become inflamed (Adnexitis), on the other hand the cervix (Cervicitis), the lining of the uterus (Endometritis), as well as the muscles of the uterus (Myometritis). If the vagina is inflamed (vagina) one speaks of a Vaginitis or colpitis. Most inflammations rise from the bottom (vagina) to the top (towards the ovaries). This leads to an inflammation of the vagina (vaginitis), followed by an inflammation of the uterus (cervicitis, endometritis, myometritis) and ultimately an inflammation of the fallopian tubes and ovaries (adnexitis).
causes
The cause of an inflammation of the abdomen are usually germs (mainly bacteria) that rise and thus continue to spread and multiply.
Inflammation of the vagina is usually caused by a disturbed vaginal flora caused by antibiotics, tampons, strong hygiene measures (e.g. alkaline soaps), lack of female sex hormones (estrogens), foreign bodies (e.g. piercing) or certain contraceptive methods (e.g. the diaphragm / pessary). From the vagina the germ can now rise further towards the cervix and inflame it (Cervicitis) and then on the lining of the uterus (Endometritis) and ultimately on the muscles of the uterus (Myometritis) spread. For an inflammation of these structures, however, there must also be a disruption of the normally protective barrier function of the cervix, i.e. the entrance into the uterus from the direction of the vagina. This is e.g. This is often the case after a birth or miscarriage, but also after operations on the uterus and after the use of contraceptive methods (e.g. IUDs). The occurrence of benign ulcers (tumors) such as myomas or polyps in the area of the cervix can also cause inflammation.
The reasons for an inflammation of the fallopian tubes and ovaries are mostly bacterial infections. These can ascend from the uterus via the fallopian tubes to the ovaries. But also an infection via the bloodstream (hematogenous) and a descending infection (e.g. via appendicitis) are possible.
Women who have adnexitis are at high risk of developing adnexitis
- frequently changing sexual partners
- use oral contraception
- are under 25 years old
- were very young when you first had sex
- Show changes in the mucous membrane in the area of the cervix (Cervical ectopy).
Inflammation often occurs shortly after ovulation (ovulation) or after the menstrual period, as the cervical mucus is very soft and permeable for germs during this time.
In general, sexually transmitted diseases (syphilis, gonorrhea / gonorrhea, genital herpes) can also lead to inflammation in the abdomen.
For more information, please also read our pages Inflammation of the uterus, Inflammation of the ovaries and Fallopian tube inflammation.
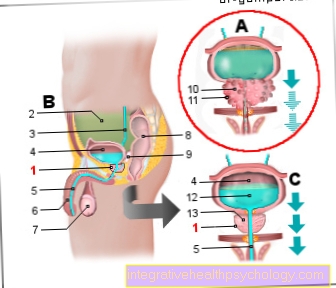
Cystitis
Cystitis is often caused by germs from the gastrointestinal tract. Women are more likely to be affected because their urethra is shorter, making it easier for germs to penetrate the urinary bladder. Symptoms include an increased need to urinate and a burning sensation or pain when urinating. The doctor diagnoses the cystitis using a urine sample. If there are white blood cells and possibly even blood or nitrite in the urine, a cystitis can be assumed. Initially, treatment can be carried out on a purely symptomatic basis with increased fluid intake. However, if this does not alleviate the symptoms, antibiotic therapy should follow.
Read more about this on our main page Cystitis
Ovarian inflammation
Inflammation of the ovaries, also known as adnexitis, is usually accompanied by inflammation of the fallopian tubes and salpinges. The typical pathogens are bacteria. They can either rise up via the vagina and uterus or extend from the abdomen to the ovaries. The symptoms are sudden severe pain in the lower abdomen with fever, nausea and vomiting. Appendicitis must be ruled out in the clinic, as it would have to be treated surgically. Ovarian inflammation can be treated with painkillers and antibiotics. If there is fever and nausea, as well as abnormalities in the ultrasound, the ovarian inflammation should be treated in hospital.
Read on for more information Ovarian inflammation
Uterine inflammation
The uterine inflammation can be inflammation of the lining of the uterus (endometritis) or of the other wall layers. Endometritis is often associated with ovarian inflammation. Here, too, bacteria are the trigger for the inflammation. The symptoms are similar to ovarian inflammation, with pelvic pain, nausea and vomiting. In addition, the uterine inflammation can also cause bleeding that does not match the cycle. In diagnostics, a pain can be triggered during the gynecological examination when the cervix is moved. This then speaks for an inflammation. The uterine inflammation is treated symptomatically with painkillers and antibiotic therapy.
You can find more information at Uterine inflammation
After birth
An inflammation of the abdomen after birth occurs when the weekly flow cannot properly run off. The reasons for the lack of weekly flow are, for example, a blocked cervix or reduced regression of the uterus due to a lack of contractions after the birth. The secretion builds up in the uterus and provides an excellent breeding ground for pathogens. If an infection occurs, the clinical picture is called puerperal endomyometritis, an inflammation of the uterine lining and muscles. Symptoms include bad smelling discharge, fever, and pain around the edges of the uterus. Rest and cooling of the region is prescribed for therapy. In addition, drugs are given that induce the uterus to contract, and antibiotic therapy is started.
Read more about this: Bed sicknesses
Chronic uterine inflammation
An acute uterine inflammation can turn into a chronic stage and thus cause a permanent, smoldering inflammation in the abdomen. The women complain of dull tenderness in the area of the uterus. Fever is rather atypical. Chronic uterine inflammation can, however, revert to an acute stage at any time and be accompanied by sudden severe pain with fever and nausea. Furthermore, a uterine inflammation can lead to adhesions in the pelvis. If the fallopian tubes are affected, sterility can occur in up to 40% of the sick women and the risk of an extrauterine pregnancy (ectopic pregnancy) is increased. Chronic pelvic pain can also occur due to the adhesions. The adhesions and adhesions are not only limited to the pelvis. Another possible complication after a uterine infection is the adhesion of the liver to the peritoneum. This is called Fitz-Hugh-Curtis syndrome. In addition, the pus can accumulate and encapsulate after an acute uterine inflammation. This creates an abscess in the pelvis. Typically the abscess is located in the Douglas space, which is located between the uterus and the rectum.
Symptoms
Inflammation of the abdomen can show many different symptoms.
For example, inflammation of the vagina can lead to increased discharge (fluorine), Itching, abnormal sensations in the vagina or pain during sexual intercourse (Dyspareunia) to lead. The discharge can have different colors (yellow, white, green, bloody), smells or consistencies (foamy, slimy, crumbly) depending on the pathogen or cause.
Also read on this topic: Swelling in the vaginal entrance
In the case of inflammation in the area of the uterus, the patients report pain in the middle of the lower abdomen, as well as pain on pressure when the abdomen is palpated. Here, too, an increased malodorous discharge (bloody, whitish-yellow, purulent) can occur. Furthermore, increased, prolonged or painful menstrual periods as well as spotting or intermenstrual bleeding can occur.
With inflammation of the ovaries and fallopian tubes, patients often report sudden onset of pain in the lower abdomen that is particularly pronounced on one side or severe pain during intercourse. Severe pain can also occur when touching or palpating the abdomen.
It can also lead to increased discharge or spotting. In very severe infections, you may feel very sick with a high fever, diarrhea, vomiting, painful urination, or bowel paralysis (Ileus) and liver inflammation.
Adnexitis is often an acute emergency.
diagnosis
An inflammation of the vagina can easily be determined by a clinical examination or visual diagnosis. The lining of the vagina often appears swollen and red. In addition to these typical signs of inflammation, small blisters can sometimes be seen. Those affected also report a disruptive discharge (fluorine).
As an important diagnostic method, the doctor will determine the pH of the vagina, take a swab from the mucous membrane and examine it under the microscope or request a microbiological examination in a laboratory. The exact pathogen can be identified here.
In the case of inflammation in the area of the uterus, in addition to the exact questioning of the symptoms (anamnesis) by the doctor, a mirror examination (Speculum examination) to detect inflammation or purulent discharge around the lining of the uterus. Here, too, a smear should be taken and examined microscopically and microbiologically. The collection takes place in the area of the cervix (cervical smear). An ultrasound scan can also indicate inflammation in the area of the uterus. This may reveal changes in the mucous membrane, accumulations of pus in the uterus, and changes in the uterus (size, shape, myomas or polyps).
Inflammation in the area of the ovaries and fallopian tubes can be detected by a palpation examination, as well as by an ultrasound examination or a keyhole operation (Laparoscopy) can be diagnosed. The swelling and accumulation of fluid (e.g. abscesses) caused by the inflammation can be detected in ultrasound and laparoscopy.
All inflammations of the abdomen have in common that, in addition to fever, changes in the blood can also appear. These changes can be detected in what is known as the blood count. For example, increases in the typical inflammation parameters in the blood (CRP value, white blood cells or the rate of sedimentation) with additional typical symptoms can be indicative of inflammation of the abdomen.
therapy
Depending on what type of inflammation of the abdomen is prevalent, one must special therapy be initiated.
So should one Inflammation of the vagina The first step is to determine which pathogen is responsible for the inflammation and what could be the cause of an inadequate protective barrier in the vaginal mucous membrane. In the next step, a specific therapy, for example in the form of Antibiotics (for bacteria) or Mushroom medicines (Antifungal drugs) can be started. This can be done using creams or vaginal suppositories, as well as syringes and tablets.
It is important that the partner must always be treated with sexually transmitted diseases!
At Inflammation of the uterus should first bed rest are complied with, as well as by an adequate Antibiotic therapy the inflammatory pathogens are combated. Also Painkiller can be used for very severe pain. If there is an accumulation of pus in the uterus, it must operationally if necessary drained and the uterus flushed with disinfectant solution.
The cause of the inflammation lies in introduced foreign bodies (e.g. the spiral), these should away become.
Also after birth it can either be through in the uterus remaining plaster cake residues (Placenta residues) lead to inflammation of the uterus, which must then be surgically removed or rejected by agents that promote uterine contraction (e.g. oxytocin).
At Inflammation of the ovaries and fallopian tubes an attempt is usually first made to contain the inflammatory process with antibiotics. If there is no improvement in the symptoms and the patient's condition, or if the pus caused by the inflammation has been encapsulated, in some cases a surgery be necessary.
There are some notable complications from such inflammation, such as
- Adhesions in the abdomen
- infertility
- Collections of pus in the abdomen with a The ovaries and fallopian tubes stick together
- a Inflammation of the peritoneum (Peritonitis) with inflammation spreading to the blood and the whole body (sepsis).
Therefore, early and intensive therapy should be carried out for inflammation of the ovaries and fallopian tubes.
Home remedies for inflammation in the abdomen
In the case of acute inflammation, local cooling measures can be useful. You can either create a cooling with the help of damp cold or ice. It is important that cooling is only carried out for a short period of time in order to avoid damage to the skin or circulatory reactions. If the inflammation is already in the healing phase, heat can also be beneficial. To apply heat, simply place a hot water bottle, a cherry stone pillow or something similar on the abdomen. If you have ovarian inflammation, you can work with mud baths or Sitz baths with hay flowers. To do this, increase the water temperature steadily until you break into a sweat.Afterwards, care should be taken to ensure sufficient rest, as these baths stress the circulation. During acute cystitis, drinking a large amount is the best home remedy. So-called bladder and kidney teas can also be useful as they contain ingredients such as bearberry leaves, which are believed to have an antibacterial effect. To prevent further bladder infections, urine can be acidified with vitamin C, for example. Plants such as nasturtiums or horseradish roots also have a good preventive effect. In general, care should be taken to ensure that sufficient amounts of water are consumed during the symptom-free phase.
You may also be interested in this topic: Home remedies for cystitis
prophylaxis
To prevent inflammation in the abdomen, there are a few important things you need to do. On the one hand, emphasis should always be placed on correct intimate hygiene. Regular washing, especially during the menstrual period or during the puerperium, is very important, but soap-free washing lotions and no vaginal douches or intimate sprays should be used. In addition, too frequent washing also destroys the vaginal flora and as a result it can no longer ward off intruders well.
On the other hand, the use of a condom during intercourse is a preventive measure to prevent inflammation in the abdomen, since the use of a condom reduces the risk of infection with sexually transmitted diseases to almost zero.
forecast
The prognosis for inflammation in the abdomen is this usually very good. With a consistent and correct treatment of the inflammation, both the vaginal inflammation and the various forms of uterine infections heal quickly and well. Inflammation of the fallopian tubes and ovaries usually also has a good prognosis with rapid, intensive therapy, but it can more often lead to complications and an emergency (acute abdomen).