Extrapyramidal disorder
Synonyms in a broader sense
Disorders of coordination of movements, Parkinson's syndrome, Huntington's disease, dystonia, Tourette's syndrome, extrapyramidal disorders
introduction
This group of clinical pictures includes, for example
- Parkinson's disease
- Chorea huntington
- Dystonia or that
- Tourette syndrome.
In all of them, the so-called extrapyramidal motor system is no longer functional enough. Its task is to coordinate the movements that the body should perform. The force, direction and speed of the movements are regulated. The extrapyramidal system does not directly trigger the movements, but only influences them and ensures uniform, fluid movements.

root cause
The extrapyramidal syndrome refers to a collection of symptoms that occur in various neurological diseases, e.g. Huntington's disease or Parkinson's disease. The extrapyramidal system describes nerve fibers that are outside the main path of movement (technical term Pyramidal track) lie and help to control our movements. The conscious movements are carried out via the pyramid path. The extrapyramidal movement system is responsible for fine adjustment and influences the pyramidal trajectory. It is responsible for the support and holding function and muscle tension (technical term tone) as well as for the movements of the limbs near the trunk. The extrapyramidal system and the main path of movement work closely together, only in this way is movement possible at all and only in this way can targeted movement and fine motor skills be carried out.
The extrapyramidal syndrome describes disorders within the extrapyramidal system that affect these areas. The exact disorder varies depending on the clinical picture. Nerve cells are usually destroyed for various reasons (e.g. also in Parkinson's and Huntington's disease), other possible causes can be the result of the ingestion of toxic substances or medication or also as a result of insufficient blood flow in the brain (such as a stroke) but there is also a genetic cause for certain diseases. There is a lack of important parts within the interconnection for the movement sequence. In Parkinson's disease activating aspects are missing, so that there is less movement (technical term Hypokinesia), in Huntington's chorea there are no inhibitory aspects, which leads to an excess of movement (technical term Hyperkinesia).
Parkinson's disease
The mean age of onset for Parkinson's disease is 55 years. Familial accumulation occurs in around 10 percent of cases. In the midbrain there is a deficiency in a certain messenger substance (med .: neurotransmitter), dopamine. Other neurotransmitters that counteract dopamine now predominate. As a result of the lack of inhibition of certain brain regions, the dopamine deficiency leads to increased tone (tension in the muscles) in the flexor and extensor muscles. Other regions that are normally stimulated are now more inhibited. Typical symptoms of Parkinson's disease include rigidity (stiffness), tremor (shaking) and akinesia (slowing of movements) and postural instability (inability to maintain balance when, for example, being pushed). Rigor arises from an increase in muscle tone (tension in the muscles). The tremor is characterized by the fact that it occurs at rest and subsides with targeted movements (for example, reaching for something). Akinesia can be recognized particularly well by walking in small steps. Most patients also have a so-called mask face, as the facial muscles are also impaired. The diagnosis is primarily clinical, based on the patient's appearance. If you try to stretch the patient's flexed arm, you will notice a certain “stutter” of the movement, the so-called cogwheel phenomenon.
A conservative treatment of Parkinson's disease, i.e. physiotherapy and exercise training, should also be carried out, as well as detailed education of the patient and their relatives.
As a drug therapy for Parkinson's disease, an attempt can be made to alleviate the symptoms by substituting the missing messenger substance. Not only the messenger substance itself, but also substances that show the same effect are used. A cure for the disease is still not possible. Only the progression can be stopped or slowed down.
You can find much more helpful information under our topic: Parkinson's disease.
Chorea huntington
There are several subtypes of chorea. The best known is probably the major chorea (Huntington's chorea). A minor form also occurs. It is a hereditary disease. A defective inherited gene copy is enough to cause disease. In contrast to Parkinson's, the same messenger substance (dopamine) has an increased effect ("reverse Parkinson's"). Due to the opposite cause to Parkinson's disease, the symptoms of the patients are basically opposite. In chorea there is hypotonic (flaccid) muscles and increased movement (Hyperkinesia).
Hyperkinesis is understood to be sudden, lightning-like and, above all, involuntary flinging movements. In the case of Huntington's disease, there are also personality changes.
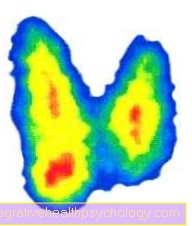
Since it is a hereditary disease, questioning (about) the family and similar diseases plays a major role. Neurological examinations, CCT (computer tomography of the skull), EEG (electro-encephalo-gram = measurement of brain waves) and blood samples follow.
Unfortunately, the cause cannot be eliminated, so the disease is incurable.Medication can be administered to reduce the occurrence of sudden involuntary movements. The prognosis for Huntington's disease is 15-20 years of survival. The prognosis for minor chorea is good, with a duration of 1 to 6 months, and healing is possible.
Further information on this topic can be found at: Chorea huntington
Dystonia
Dystonia is a state of tension in the muscles with abnormal postures. These can occur sporadically (e.g. only the right side of the neck), one-sided or generalized. The cause lies in the loss of nerve cells, which are important for the coordination of movements. Familial clusters occur. Tumors (benign or malignant) are also possible. There are therefore primary and secondary forms caused by other diseases. Depending on the location of the lesion in the nerve tissue, various complaints arise. Often the so-called Spasmodic torticollis. This is understood as a slowly progressing spastic neck and neck muscle contraction. The head then turns to the opposite side.
Other parts of the body (hands, arms) can also become cramped due to muscle contractions.
The diagnosis is made through anamnesis (questioning) of the patient and a neurological examination. Therapy is carried out by giving medication to prevent muscle spasms. The injection of botulinum toxin (Botox®) also shows a good effect, but is still being tested more precisely and should only be used by specialists in neurology, as it can lead to significant side effects (e.g. difficulty swallowing) if used unprofessionally. The Botox® blocks the receptors to which the messenger substances that mediate muscle contraction normally attach. This poison is broken down after about 3 to 4 months, so that a new injection must be made. This disease continues to progress.
Tourette syndrome
Tourette syndrome is an inherited disease that affects men more often than women. Here, too, a certain region of the brain, the basal ganglia, is affected. Ultimately, many different causes of Tourette's syndrome are currently being discussed. However, no theory is so far proven that one can speak of a certain cause. The patients suffer from motor tics (winking, mouth twitching, tongue clicking, shoulder twitching). Tics are uncontrollable muscle movements. Vocal tics are also possible (noises, throat clearing, grunts, even whole words). Obsessive-compulsive disorder is also a symptom. Questioning the patient, neurological examinations and the EEG are used to establish the diagnosis. Play therapy and talk therapy can be used as therapy. The obsessive-compulsive symptoms can be treated with medication. The tics are also tried to contain with medication.
Further information on this topic can be found at:
- Tourette syndrome
- Tics
What are accompanying symptoms?
If an extrapyramidal syndrome manifests itself with excessive movement, involuntary arm movements occur. The facial muscles are often moved involuntarily, for example in the form of chewing movements.
If an extrapyramidal syndrome manifests itself with a sedentary lifestyle, tremors, freezing when walking or when reaching for an object (i.e. the patient wants to perform the movement, but the foot or hand simply does not begin to move) can occur. The facial expressions can also become impoverished overall, so that the person concerned usually only shows an expressionless face.
The severity of the symptoms can indicate certain diseases. In general, those affected also fall more often. Since many of the causative diseases belong to the neurodegenerative group, accompanying dementia often occurs. The personality of the person concerned can also change. For example, seemingly baseless aggression can occur. If those affected notice these changes, depression is not a rare comorbidity.
Also read our topic: Parkinson's disease symptoms
How do you make the diagnosis?
The diagnosis is made primarily through a detailed medical discussion (technical term anamnese) and performed a thorough physical examination. It examines exactly what kind of sedentary lifestyle or excessive physical activity is present and how it manifests itself. In some cases a clear diagnosis can be made. However, since different clinical pictures merge into one another, until a definitive diagnosis is made, only the presence of an extrapyramidal syndrome is often discussed. Certain imaging tests (such as certain MRIs) and certain blood tests in some cases can confirm the diagnosis. Often other diagnostic procedures are added to rule out other diseases. Sometimes genetic testing, a removal of spinal cord fluid (technical term Liquor) or the response to certain medications for diagnosis.
A general statement about a prognosis is not possible. It depends entirely on the specific clinical picture and on the various therapy options as well as on the medical history and family history.
How does the coordination of movements work?
The Coordination of movements is controlled in a part of the brain that is in the Diencephalon and midbrain lies. Here is the control of the involuntary Movements and posture.
The so-called extrapyramidal system consists of several components that all perform different tasks and yet work perfectly together. In the brainstem, for example, holding and adjusting reflexes are interconnected. These are involuntary. Nobody has to consciously think about standing to stop.
Even when the bus quickly takes a sharp bend, we usually don't fall over, but instead regulate our power to the opposite side - in a flash and without having to think about it.
Another station is the Thalamus, the "gateway to consciousness", to call. Here the information about the position of muscles and joints is processed and perceived.
The Cerebellum plays a big role in balance.
In the Basal ganglia certain movement sequences are saved and called up.
Summary
The disorders of movement coordination include, among other things Parkinson's Syndrome, Chorea huntington, Tourette syndrome and the Dystonia. What they all have in common is the fact that movements can no longer be coordinated sufficiently.
These complaints range from Trembling of hands up to increased muscle tone, i.e. more cramped Musculature.
Different areas of the body are affected depending on the disease. Various mechanisms are disturbed at the brain level, but all of them affect the so-called extrapyramidal system.

















.jpg)