uterus
Synonyms
Uterus, metra, hystera
Ovary, pregnancy, menstrual cycle, ovaries
English: uterus, womb
anatomy
The uterus is one of the woman's reproductive organs and is located in the small pelvis. It is a roughly pear-shaped organ 5 cm wide and 7 to 8 cm long. Your weight varies between 30 and 120g depending on whether you have already been pregnant or not.
Further information on the anatomy of the abdominal cavity can be found here: Abdominal cavity
Illustration of the uterus

- Uterus -
uterus - Uterine tip -
Fundus uteri - Uterine lining -
Tunica mucosa - Uterine cavity -
Cavitas uteri - Peritoneum cover -
Tunica serosa - Cervix -
Ostium uteri - Uterine body -
Corpus uteri - Uterine constriction -
Isthmus uteri - Scabbard - vagina
- Cervix - Cervix uteri
- Ovary - Ovary
- Fallopian tubes - Tuba uterina
You can find an overview of all Dr-Gumpert images at: medical illustrations

- Uterus - uterus
- Uterine tip - Fundus uteri
- Uterine lining -
Tunica mucosa - Uterine cavity - Cavitas uteri
- Peritoneum cover - Tunica serosa
- Cervix - Ostium uteri
- Uterine body - Corpus uteri
- Uterine constriction - Isthmus uteri
- Scabbard - vagina
- Pubic symphysis -
Pubic symphysis - Urinary bladder - Vesica urinaria
- Rectum - Rectum
Based on their structure (anatomy), the doctor divides them into different sections. The lower part of the uterus that connects to the vagina is called the cervix (cervix uteri). It is divided into a part reaching into the vagina (portio vaginalis cervicis) and a part above the vagina (portio supravaginalis cervicis).
The section reaching into the vagina contains the outer opening of the uterus, the so-called external cervix (Ostium anatomicum uterinum externum). The part of the cervix above the vagina contains the inner cervix (Ostium anatomicum uterinum internum). An approx. 0.8 cm long bottleneck (Isthmus uteri) joins that cervix and separates it from the body of the uterus (Corpus uteri). Inside the body of the uterus is the uterine cavity (Cavits uteri), in which above the Fallopian tubes (Uterine tubes) flow. Above this point of confluence lies the uterine fundus (Fundus uteri).
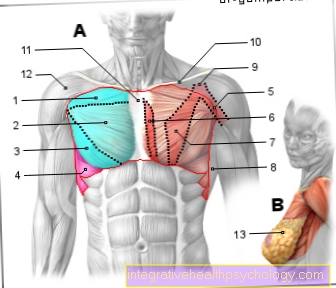
If one looks at the longitudinal axis of the vagina, the body of the uterus is bent forward from the isthmus (Anteversio uteri) and bent forward (Anteflexio uteri). The uterus comes so behind and on top of the bladder (Vesica urinaria) to lie down. At the top, the uterus also borders the Small intestine (Ileum) and to the Colon (Sigmoid colon). Behind the uterus lies - separated by the Douglas room - the rectum (Rectum).
The uterus has three layers of walls. Inside, facing the uterine cavity, lies the layer of mucus (Endometrium). This is covered on the outside by a 1 to 3 cm thick layer of muscle (Myometrium) surround. The muscle layer is in turn made up of one connective tissue (Parametrium) enclosed.
There is a connective tissue plate on both sides of the uterus (Lig. Latum uteri, mesometrium) that connect the uterus to the fallopian tubes (Uterine tubes) and the Ovaries (Ovaries) connects and runs out in the pool wall. In this connective tissue plate there are blood and lymph vessels as well as nerves. There are also special straps that have a holding function. On the one hand, it is a ligament that extends from the body of the uterus at the point of entry of the fallopian tubes (Tuba uterina) to the Ovaries (Ovary) pulls (Lig. Ovarii proprium = Lig. Uteroovaricum) and on the other hand around a band, that from Uterine body starting through the Inguinal canal (Canalis inguinalis) in the tissue of the great labia minora (Labia majora) pulls (Lig.teres uteri). At the back on the side of the connective tissue plate there is also another band (Lig. Suspensorium ovarii).

Anatomy uterus
- Uterine cavity
- Cervix / cervix
- Scabbard
- Tube / fallopian tube
- Ovary / ovary
- Corpus / body
- Portio / cervix
Size of the uterus
A normal uterus in a woman who has not yet had children is usually about 7 cm long and roughly the shape of a pear. If several births have already taken place, one speaks of a normal result even if the patient is 8 cm in length. Of course, the uterus can expand considerably during pregnancy and grow in size to such an extent that it can accommodate one (or more) child (ren). This, too, is then physiological.Some women have an extremely large uterus for no apparent reason; older women do so more often. In addition, there are also some gynecological diseases that are associated with an enlargement of the uterus. Any type of tumor (in the sense of a swelling, i.e. not only malignant tumors, but also, for example, myomas or cysts) can lead to a mostly local, but sometimes also generalized, enlargement of the uterus. The size of the uterus plays a crucial role if a surgical procedure is to be carried out, as different access routes are preferred depending on its size. In addition, a greatly enlarged uterus can lead to discomfort as it displaces and / or constricts neighboring tissue or organs.
Uterus enlarged
An enlarged uterus can have a number of causes.
On the one hand, this can otherwise take approx. 7cm long, pear-shaped hollow muscle organ during a pregnancy increase considerably in size and mass when they - adapted to the growth of the unborn child - expands.
But some women can too from birth have a larger uterus than others or it may cause insignificant enlargement in old age come. However, all three variants are physiological enlargement of the uterus and have no disease value.
In contrast to this, however, there are also changes to the uterus, which on the one hand are not physiological and on the other hand too Complaints or problems being able to lead. This includes the enlargement Cysts (liquid-filled cavities), due to benign tumors (Fibroids) or malignant tumors.
If these tissue changes occur sporadically, the uterus can only locally enlarged be, they occur multiple, but they can also increase in size as a whole (e.g. in a uterus myomatosus).
From a certain increase in size, various symptoms can appear, for example Menstrual abnormalities, Difficulty getting pregnant as well Problems urinating, Constipation, lower back pain and circulatory disorders due to the increased pressure on the surrounding organs (Urinary bladder, ureters, intestines, nerves and vessels).
Uterus tilted backwards
Usually the anatomically correct position of the uterus in the female pelvis is one facing forward bladder inclined position (Anteversion, anteflexion).
Under certain circumstances, however, the position of the uterus can deviate from the norm, so that, for example, it slightly shifted left or right, vertically or else tilted backwards (Retroversion, retroflexion) can lie.
There can be various causes for a tilted uterus, leading to one from birth is designed like this or it is only in the course of life leaves its original, forward-sloping position.
This can be done, for example, after a pregnancy or delivery (i.a. due to voltage losses in the uterine ligamentous apparatus) may be the case, but also due to scarring in the context of a Endometriosis or from fibroids.
In most cases, the uterus remains tilted backwards symptomless, however, in some cases it can also use Menstrual pain, Back pain, Constipation, Painful intercourse and Difficulty trying to have children accompanied.
May be Ovarian cysts and endometriosis may be associated with a backward tendency. Therapeutic methods are used in the case of a symptomatic, backward-tilted uterus Hormone therapies, pelvic floor exercises, pessary therapies and surgical corrections in question.
Influences of the menstrual cycle on the uterus
The mucous membrane of the uterus is subject to cyclical fluctuations caused by the Hormones be managed. These hormones are Estrogen and progesteronethat are in the Ovaries are formed.
A menstrual cycle lasts an average of 28 days.
Based on the Uterine lining the cycle is divided into four phases.
The first phase, the growth resp. Proliferation phase starts on the third / fourth day of the Menstrual period and lasts up to about 14 days after the menstrual period. During this phase, a high proportion of estrogens is formed in the ovaries. Due to the influence of these hormones, the mucous membrane in the uterus in thickness and the glands in the mucous membrane in size. New vessels also form that are spirally aligned and are therefore also referred to as spiral arteries. At this time, the mucous plug in the cervix is thin under the influence of estrogen. This thin fluid allows the sperm to pass well through the cervix, into the uterus and then into the fallopian tubes, where a Fertilization of the egg can take place. Usually it comes on the 14th day after Menstrual period for ovulation (Ovulation) and, at the same time, a sharp drop in estrogen.
The second phase of the cycle is called Secretion phase referred to because in this the uterine glands are full of mucus and secrete it (secrete). This phase lasts until the 25th day after the last period. The greatest amount of mucus is secreted on the 21st day. The plug of mucus in the cervix is now thickened and viscous. The hormone that dominates in this phase is progesterone. It is made in the corpus luteum in the ovaries. From the 25th day onwards, the concentration of progesterone also drops rapidly.
This withdrawal of hormones leads to a contraction (contraction) of the vessels in the mucous membrane (third phase). As a result, the mucous membrane is no longer supplied with the nutrients it needs and it dies.
Around the 28th day after the last bleeding, the previously contracted (contracted) vessels widen again and an influx of blood occurs. This causes the vessel walls to tear (rupture). There is bleeding. Now the dead layer of the mucous membrane is peeling off. This and that blood from the torn mucous membrane vessels the woman takes as Menstrual period true. At this stage one speaks of the desquamation phase (fourth phase). It lasts 1-3 days. After that, the concentration of estrogen in the blood rises again and the cycle starts all over again.
Uterine pain
Pain in the uterus can various causes have, whereby this does not always have to affect the uterus itself, but also other, immediately adjacent, inner (Gender)Organs can radiate to the uterus.
The most common causes of pain in the uterus include discomfort during the Menstruation - the so-called Dysmenorrhea. If the menstrual period is excessive Abdominal pain and Cramps in the uterus Accompanied by, for example, a prostaglandin level that is too high, too low Estrogen / progesterone levels, benign uterine tumors (Fibroids, cysts) or congenital uterine malformations be conditional.
Another reason for painful discomfort in the uterus can be a Endometriosis be. This means the occurrence of Uterine lining outside of their actually natural position, e.g. B. in the Uterine muscles, to the Fallopian tubes/Ovaries, in the vagina, but also on Intestines, the bladder or even the lung. This dispersed uterine lining is subject to this just like the actual one hormonal cycle the woman, so that after the mucous membrane has built up, there is also a withdrawal bleeding due to the mucous membrane rejection during menstruation. Depending on the localization, these external foci can be too significant pain (Uterine or abdominal pain) and Bleeding outside the uterus to lead.
Furthermore, it can too harmless pain in the uterus during a pregnancy come when it has to adapt to the size of the child in the process of stretching and growing.
Another cause of uterine pain can be a Inflammation of the lining of the womb be in the context of an infection (Endometritis). The reason for this is usually the rise of Bacteria from the vagina or that cervix. Local tenderness over the uterus and an additional occurrence of fever and bleeding outside of menstrual period.
Is there a Inflammation of the ovaries, this can also lead to pain that may be felt in the area of the uterus, but it is mostly unilateral pain that more to the left or right to radiate out.
Also a Prolapse of the uterus, in which the uterus turns out of the vagina, can lead to pain in the abdomen.
In addition, can also malignant tumors of the uterus lead to pain in the abdomen, although this is usually only the case at an advanced stage when it comes to other pelvic / abdominal organs.
Diseases of the uterus
Inflammation (Infections) of the uterus are mostly ascending infections from the Scabbard (vagina). The infections can be caused by viruses, bacteria or Mushrooms caused. One reason for such an infection can be, for example, unprotected sexual intercourse.
It can Inflammation of the cervix (Cervicitis) or on the body of the uterus. Only the mucous layer on the body of the uterus can be inflamed (endometritis), only the muscle layer (myometritis) or both layers (endomyometritis).
The cervix can be the seat of a benign (benign) or malignant (malignant) lump (tumor).
Benign tumors of the Cervix can genital warts (condylomas), Polyps or be cysts. Some smooth muscle wall tumors (called leiomyomas or fibroids) and changes in the cells of the Cervix in the so-called transformation zone.
Malignant tumors of the cervix are the Cervical cancer (Cervical cancer) and preliminary stages (precancerous lesions) from cervical cancer (cervical intraepithelial neoplasia = CIN).
A distinction is also made between benign and malignant tumors on the body of the uterus. Polyps, increased growth of the mucous membrane (endometrial hyperplasia) and swellings of the muscle layer (myomas) are to be regarded as benign. Parts of the uterine lining can also move to other places such as the uterine muscle layer or even the Ovaries to settle (Endometriosis) and then make cycle-dependent changes there. This would also be an example of a benign tumor.
You can find more under our topic Endometriosis.
The Uterine cancer the mucous membrane (Endometrial carcinoma = body carcinoma) and the muscle layer (Uterine sarcoma, Leiomyosarcoma) represent malignant tumors.
In old age, some women suffer from a sagging (descensus) and protruding (prolapse) of the uterus.
Causes are, for example, a weak connective tissue or previous births. (please refer: Uterus subsidence after birth) The uterus loses its hold and slides down towards the vaginal outlet.
Uterine cysts
Uterine cysts are fluid-filled cavities that are lined with epithelium and surrounded by a capsule, with either completely in the tissue the uterus or over one Tissue stalk (pedunculated cysts) can be connected to it.
The size of the uterine cysts can be varied, and they can single or multiple occur and affect every age. The cavity of the cyst can thereby be made out one or more chambers consist.
The cause of the formation of uterine cysts has not yet been fully understood, to be suspected hormonal connections. Cysts on the uterus do not necessarily have to cause symptoms; depending on their location and size, they can be complete symptomless stay and appear as an incidental finding in routine gynecological examinations or are associated with significant complaints.
Changes in the Menstruation, Abdominal pain or other uncharacteristic complaints to others Organs come when very large or many cysts put pressure on the surrounding tissue.
As many cysts reappear frequently regress spontaneously or burst therapy is not always necessary. In the case of clear symptoms, on the other hand, hormonal and surgical therapy methods are used.
Operation of the uterus
An operation on the uterus is one of the most common interventions in gynecology today. Diseases that make an operation on the uterus necessary include, among other things malicious changes (i.e. cancer or suspected cancer), benign changes (for example Cysts or Fibroids), one Endometriosis, Adhesions / adhesions or Inflammation. In addition to the classic method, which requires the abdominal wall to be opened, two new options are available for surgery on the uterus: The vaginal (Access through the vagina and therefore no scarring) and the laparoscopic surgery (Laparoscopy, i.e. only tiny incisions in the skin through which the surgical instruments and camera / light source are inserted).
Removal of the uterus
Surgical removal of the uterus - too hysterectomy called - can either the sole, complete or partial removal of the uterus mean or an additional removal of the Ovaries and the Fallopian tubes (Adnexa) - depending on the indication.
The most common reasons for a hysterectomy include benign diseases of the uterus, such as those that cause discomfort Fibroids (Uterus myomatosus), Cysts or Endometrial foci, but also serious, stressful ones Menstrual irregularities or discomfort or a Prolapse of the uterus (Uterine prolapse). In just under 10% of cases, the uterus has to be removed because of a malignant disease (e.g. cervical cancer, Endometrial cancer, Ovarian cancer).
In addition, the hysterectomy can also be considered a last resort option insatiable bleeding after a Childbirth or at severe infections or. Inflammation of the uterus be applied.
Depending on the underlying illness, accompanying illnesses, size and mobility of the uterus and the patient's request, come accordingly different surgical methods in question, generally getting conservative surgery across the stomach (abdominal hysterectomy), through the Scabbard (vaginal hysterectomy) or a laparoscopic operation using the keyhole principle through the abdominal wall differs. In addition, there is also a robot-assisted hysterectomy now possible with the DaVinci robot.
In benign diseases of the uterus, vaginal, abdominal or laparoscopic access is usually chosen, whereby the uterus is either only partially (subtotal extirpation; the cervix remains) or completely removed (total extirpation) will or even the Fallopian tubes be taken away (varies depending on the disease, in principle with benign diseases the attempt is always made to preserve as much as possible).
The abdominal hysterectomy is preferably performed in a very large uterus (z. B. in uterus myomatosus) or a Partial distance performed, with the uterus classically in general anesthetic is removed via an incision in the abdomen.
The vaginal removal, on the other hand, is the gentler and faster variantbecause the surgical route is shorter and the procedure less invasive. Here, the uterus is removed through the vaginal canal, but the cervix is preserved not possible.
If there is a malignant disease of the uterus, the so-called radical hysterectomy resorted to Wertheim-Meigs. This leads to the complete removal of the uterus and its holding apparatus, the Lymph nodes of Basin and the upper third of the scabbard.
Depending on the anatomical conditions and the patient's condition, this operation can be performed conservatively abdominally or laparoscopically.
With the removal of the uterus there is also the possibility of one conception irrevocably taken what the patient was about before the operation clearly enlightened should be. If you still want to have children, the doctor can - depending on the disease of the uterus - Consider an alternative, uterine-preserving therapy.
Further consequences of a hysterectomy include the complete absence of the Menstruation (at total distance) or a slight cyclical bleeding with only partial removal of the uterus, hormonal changes and - depending on the age at the operation - a possible entry into the Menopause with removal of the adnexa.
Transplant of the uterus
The first Uterus transplant took place in years 2011 in a Turkish patient who was born without a uterus. The organ came from a deceased donor. In September 2012, two women in Sweden were each successfully transplanted with a uterus from a living donor. The first recipient of the uterine transplant has been since April 2013 after the implantation of an embryo pregnant and there is justified hope that this pregnancy can be carried out successfully. Thanks to this new procedure, there are completely new possibilities for the many women who are born without a uterus or who have it removed in the course of their lives due to an illness. For them, too, it now seems quite conceivable that a Desire to have children no longer has to remain unfulfilled. Further developments and tests are still pending in this area.