Obstetrics
Synonyms in the broadest sense
Delivery assistance
introduction
The Obstetrics, also Tokology or obstetrics Called, is a medical specialty that deals with monitoring normal and pathological Pregnancies, as well as with the birth and follow-up treatment. Obstetrics is a branch of the Gynecology (gynecology). The work of obstetricians and midwives also falls under the field of obstetrics.
history
The Obstetrics was for a long time the only medical field that specifically treated women. Other pathological abnormalities in women were not treated by specially trained doctors. This is how the sub-area developed Gynecology only well into modern times. The field of obstetrics was considered a women's domain until the 17th century. Only then were men trained as so-called obstetricians. The predominantly practical activities of midwives have been handed down from ancient Greece. The transition from midwife to doctor was fluid. Since the early modern period, special emphasis has been placed on the professional training of midwives. This is how midwifery textbooks and midwifery regulations were created.
The first printed midwifery textbook for obstetrics is from the year 1513 and was made by Eucharius Rosslin, one City doctor in , composed. However, the resulting midwifery regulations also had disadvantages. So they became Midwives gradually ousted from their leading positions, and the City doctorsThose who had learned their skills themselves from the midwives took the leading positions.
In contrast, prenatal diagnostics did not change until the middle of the 20th century. Until then, midwives and doctors had to rely on simple manipulations and physical exams. By developing the Contact compound scanners 1957 by Ian Donald, and the construction of a real-time scanner 1965 by Richard Soldner it was possible to have much more precise knowledge of a pregnancyto get the course and the child. This has not only brought great benefits for the obstetrician, but also for the expectant mothers.
In addition to prenatal diagnostics, the area of abortion has also undergone major changes. Was a Termination of pregnancy Previously associated with great risks, the complications are now so minor that an abortion can hardly lead to a dangerous situation for the mother.
Care during pregnancy
The Care of pregnant women during the entire period of pregnancy and under the birth is the field of activity of obstetricians.
The first examination and consultation of a pregnant woman should be done as soon as possible after the onset of pregnancy in order to check for abnormalities, such as a Ectopic pregnancyto determine. In the case of normal pregnancies, the following examinations can be carried out according to the maternity guidelines, i.e. every 4 weeks up to the 32nd week of pregnancy (SSW), then every 2 weeks until the due date. These are health insurance benefits.
In practice, however, an examination scheme is used Spreader recommended. In the first 4 months (until 1st to 16th week of pregnancy) one every 4 weeks Medical check-up instead, in the following 3 months (17-28 weeks of pregnancy) every 3 weeks and in the following 2 months (29-36 weeks of pregnancy) every 2 weeks.
After that, the patient will be examined weekly up to the 40th week of pregnancy, every 2 days from the calculated due date. If the child has not yet been born 10 days after the calculated due date, the mother should be admitted to hospital.
The initial examination of the pregnant woman for Obstetrics includes a thorough medical history, i.e. Age, name, marital status, occupation, number of previous births and pregnancies. Problems or abnormalities in previous pregnancies should also be discussed. Also should have chronic diseases of the mother or infections like hepatitis, HIV and rubella as well as other known illnesses in the family. In order to be able to calculate the exact due date, it is helpful to know the woman's cycle, and thus the first day of the last Menstrual period.
The following examinations should be carried out at every preventive examination: A thorough medical history of the current situation. For example, changes in the last few weeks with regard to child movements, bleeding, or other complaints. In addition, the mother's body weight should be measured every time. A weight gain of 1-1.5kg / month is considered normal. To a pregnancy-induced high blood pressure to recognize, this should be measured regularly. The limit is 140 / 90mmHg. Urine should also be up regularly Egg whites or sugar checked to one Gestational diabetes to recognize early. You should also have regular blood tests to get a anemia to exclude. As a physical examination method for optimal Obstetrics In principle, the fundus level should be felt in order to check the timely development of the child and a vaginal examination is carried out to assess the cervix, the cervix and the pelvic situation.
Further preventive measures in obstetrics are 3 Ultrasound examinations during pregnancy, unless the pregnancy is at risk. These ultrasound screenings take place around the 10th, 20th and 30th week of pregnancy. The first Ultrasonic serves to determine the position of the child in the uterus. In addition, the due date can be calculated based on the size of the child. The other two ultrasound examinations serve primarily to rule out fetal malformations and to monitor timely development. In addition, the calculated due date is checked again and corrected if necessary.
In addition, from the 28th week of pregnancy regularly the Heart sounds of the child with the help of a CTGs to be checked.
In Rh-negative mothers, Rh prophylaxis should be carried out at this time to avoid possible complications under the birth of a Rh-positive child. From the 30th week of pregnancy, it is important to determine the exact position of the child. In other words, whether the child is facing the pelvis. Hepatitis B screening is carried out as close as possible to the due date.
If the child has exceeded the due date, very regular checks of the heart sounds, as well as ultrasound examinations showing the blood flow to the fetal organs, are essential in order to detect a possible under-supply of the child.
Field of activity of midwives

The Activity of midwives obstetrics covers a wide area and hardly differs from that of doctors. A midwife is according to the Midwifery law trained to give birth without a doctor. On the other hand, a doctor is not allowed to give birth without a midwife. The midwife supports the mother-to-be in dealing with the premature labor during the birthLabor pains. She gives advice and helps with pain relief. With a physiological Spontaneous birth she should also respond to the wishes and concerns of the woman giving birth. For example, the position can be changed. But the midwife also needs one physiological of a pathological birth process distinguish and act when in doubt or consult a doctor.
In Emergency situations a midwife should be able to act independently, and so, for example, a trapped one shoulder free the child. If a doctor needs to be called in, the midwife will act as Obstetrics for the doctor and also assists during one Caesarean section.
The midwife takes over during the birth the birth management. She takes the mother into the delivery room, pays attention to her general condition, checks the contractions and gives Contractions or Contractions after consultation with the doctor. In addition, she has to assess the progress of the birth by checking the opening of the cervix and the attitude and posture of the child as well as stepping deeper into the pelvis in order to identify postural anomalies or other complications at an early stage. Furthermore, it is used for constant monitoring of the child CTG responsible, judge that Amniotic fluid for pathological bleeding and may if necessary Fetal blood analysis to be able to better assess the child's situation.
During the Expulsion phase it prevents too early pressure to prevent a uterine rupture by instructing the mother to breathe properly.In the interests of the child and mother, the expulsion period should not last longer than 60 minutes. The proper rotation of the child's head must be checked during the entire expulsion period. In addition, the child must be constantly monitored using CTG. The midwife is also responsible for the Dam from tearing to protect, possibly a must Perineal cut be performed. After the birth, she is responsible for cutting the cord and the subsequent first aid.
Be there size, Weight and Head circumference measured. In addition, it is checked whether all body orifices are properly created, and other abnormalities must be recognized. In addition to looking after the newborn, the midwife also takes care of the mother's follow-up care right after the birth.
Also in the course of the Puerperium the midwife is an important contact person for the mother. She gives important tips on nutrition and care of the child, controls the tissue regression in the mother and offers regression gymnastics.
Course of birth

Only approx. 4% of all pregnant women give birth exactly on the calculated due date. Most children are born +/- 10 days around the calculated date.
The Obstetrics starts a few weeks before the expected due date. About 4 weeks before the actual birth, the uterus begins to lower itself. This is easy Labor pains hand in hand. During this time the head also enters the maternal pelvis. In multiparous women, the head may have entered the pelvis relatively little before birth.
Uncoordinated labor occurs a few days before delivery. In addition, the Cervix softer in the days before childbirth and the cervix opens easily. Then the Cervical mucus Shed with added blood is the sign of an imminent onset of labor.
The normal one The birth process is divided into 3 phases a.
In the Opening period will the Labor pains slowly regularly. The Opening pains occur every 3-6 minutes and the entire phase lasts 7-10 hours for primiparous women and approx. 4 hours for multiparous women. In addition, at the beginning of this phase, the rupture of the bladder occurs. The opening phase ends with the complete opening of the cervix.
With the opening of the cervix the Expulsion phase.
This takes about 1 hour for first-time mothers, i.e. about 20 contractions, about 30 minutes for multiparous women. In this phase there is permanent monitoring by means of CTG essential.
If the child's head or rump is lower, the urge to press begins to increase. If there is a risk of overstretching or of perineal cracks, a perineal incision should generally be made to avoid uncontrolled tearing. At the moment of the head passage, pressing is prohibited and there is a dam protection. The midwife places one hand on the perineum and tries to avoid tearing it. During the entire birth, the child has to make 5 turns in order to always stay in the optimal position.
Following the birth / obstetrics, the so-called Postpartum period. First of all, the child's umbilical cord must be cut. There are 3 possible times for this. Immediately after the birth, after about 1 minute or after the umbilical cord pulsation has stopped. The contractions in the afterbirth phase serve on the one hand to shrink the uterus and on the other hand to reduce the size of the uterus Expulsion of the placenta. This usually takes about 30 minutes. The blood loss during placenta detachment is usually around 300ml. To speed up the solution process and to keep blood loss as low as possible, often Contraction means given. If the placenta detachment is delayed or if the detachment takes place only partially, the placenta can be detached manually.
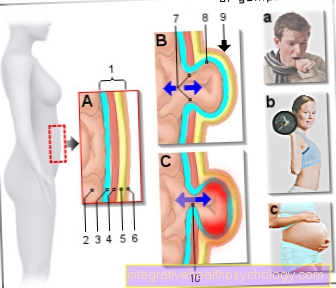
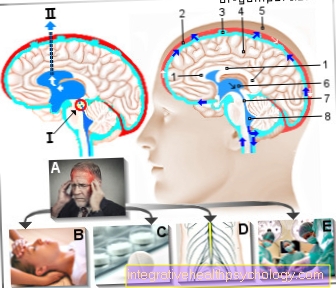
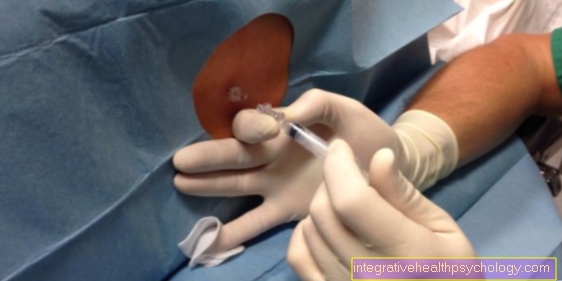
To reduce the pain during childbirth, one can Buscopan® be given to the spasms of the Musculature to reduce. If the contractions are too strong, the birth does not run normally, with a caesarean section, or at the request of the mother one can Epidural anesthesia be created. A local anesthetic is injected into the epidural space in the lower vertebral area. The danger of a Spinal cord injury does not exist. The third option is a pudendus block. A local anesthetic is injected into the genital region in order to relieve the perineal stretch pain. This relaxes the pelvic floor muscles, the perineal area, vulva and lower Vaginal area are anesthetized without affecting the pain in labor or the urge to press. Indications for this are one vaginal delivery, at the request of the mother or earlier Perineal cut.
Also read: Perineal cut.
Complications

Regular birth is the most common form of delivery. Nevertheless, there are various positional and postural anomalies that can lead to problems during childbirth, require intervention by the obstetrician / obstetrician or make a caesarean section necessary.
Read more on this topic: Breech position
Postural anomalies are when the child's head is not held regularly, i.e. with the chin pressed lightly on the chest. The postural anomalies are usually not unexpected, as they often represent an adaptation to the birth canal. One differentiates between the frontal position. Here the child keeps their head relatively straight. This increases the diameter that must pass through the middle of the pool. This is often underestimated. Another possibility is the forehead position. The child overstretched its head and the first thing at birth the forehead emerges from the birth canal. Since the diameter is the largest here, this position is the most unfavorable. The final type of postural abnormality is face position. Here the head is completely overstretched. It is often possible to give birth spontaneously, but a caesarean section should not be delayed if indicated.
Approx. 5% of births result from breech birth. The child does not lie ahead with its head, but with its rump. Due to its flexibility and its smaller size, in contrast to the head, this is less suitable as a dilator of the birth canal. In addition, at a certain point during the birth, the umbilical cord is compressed and the child is under-supplied with oxygen. Furthermore, the head must be born against a significantly higher resistance. As a result, the pressure and tensile loads on the head, neck and spine are significantly stronger and can lead to neurological abnormalities. For these reasons, breeches should always be carefully monitored. If there is the slightest doubt that the birth will go off without complications, a caesarean section should be performed.
Breeches are more common in premature births, since the child is physiologically in breech position until the end of the 2nd trimester and does not rotate until the 3rd trimester. Due to the great exertion and high complication rate, children born before the 36th week of pregnancy should be brought in with a caesarean section if they are in breech position. A distinction is made between different forms of breech position. The purely breech position means that the feet pinch the head and only the rump precedes. In the rump-foot position, the feet are angled as if sitting cross-legged and go ahead together with the rump. These two positional anomalies are the most favorable and can lead to a natural birth without a caesarean section in an otherwise uncomplicated birth.
In the foot position, the legs are straight and the feet go ahead, while in the imperfect foot position, one leg is straight and the other is bent. Both positional anomalies make a natural birth very difficult and are an indication for a caesarean section.
Absolute indications for a caesarean section from breech position are an estimated weight> 4000g, a foot position, hyperextension of the head, with a previous caesarean section or suspected malformations or a Hydrocephalus (Water head).
Another positional anomaly is the banked position, which occurs in 0.7% of births. The reason for this is that the child can move extremely freely in the pelvis, which can have different reasons. These include a very small child with premature birth, a lot of amniotic fluid, and a sagging uterine wall and abdominal wall in multiparous women. However, obstacles such as multiple births or uterine anomalies can also lead to a lateral position. If this is not treated, the arm prolapses after the rupture of the bladder and the shoulder becomes trapped. If the labor activity increases, the uterus can contract continuously and tear. The caesarean section is absolutely indicated in such a situation.
Multiple births are also always considered to be risk births. After the birth of the first child, there is a risk of premature placenta detachment and thus a life-threatening situation for the second child. If the twins are both in the skull position and there is no reason for complications, nothing stands in the way of a natural birth process. Even if the second twin is in the breech position, a spontaneous delivery is possible as long as it is relatively small. In all other cases and with more than 2 children, a caesarean section is usually carried out immediately.