Yeast in the intestine - what are the consequences?
Definition - what is meant by yeast in the intestine?
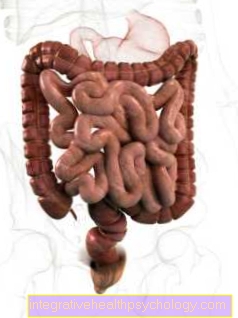
Yeasts such as Candida albicans are found on the skin or mucous membranes of about 30% of all healthy people. These yeasts are facultative pathogenic, which means that they only cause infection in immunocompromised patients.
If the immune system is mildly weak, the outer skin or mucous membranes can become infected - if the immune system is severely weak, internal organs such as the intestine can also be infected. It is not uncommon for the human body to come into contact with yeast fungi, for example through food or physical contact. In the case of immunocompetent people this does not matter and the yeasts are contained by the cells of our immune system.
What is a yeast fungus? For general information on yeast, also read: Yeast

Causes - How do yeasts get into the intestines?
The most common pathogen that causes yeast colonization is Candida albicans. This yeast can be found in about a third of all healthy people and is responsible for a large proportion of yeast infections of the intestine. Candida albicans is a facultative pathogenic germ, which means "possibly pathogenic". This allows Candida albicans to be in the intestine without causing an infection. Only when the body's own immune system is in a state of inability to contain the facultative pathogenic germ does the disease arise. If the bacterial flora of the skin or mucous membrane changes or a patient develops an immunodeficiency, it can lead to an overgrowth with yeasts.
Diseases that are associated with a strong weakening of the immune system and thus with an increased risk of yeast overgrowth in the intestine are primarily tumor diseases, diabetes, leukemia or an infection with the human immunodeficiency virus (HIV). The condition after an organ transplant also describes this fact.
Medicines such as steroids, antibiotics or chemotherapy drugs also lead to changes or damage to the natural intestinal flora.
Extreme loads with a high stress level can also lead to an increased susceptibility to yeast infections of the intestinal mucosa.
Is human-to-human transmission also possible? To do this, read: How contagious are yeasts?
When does the amount of yeast in the intestine become pathological?
There is no specific indication of the amount of yeast in the intestine that is considered normal or pathological. Rather, it depends on the composition of the normal skin and mucous membrane flora and on the interaction of the yeast with the body's own immune system.
If a person is immunocompetent, yeast colonization goes unnoticed. However, if the immune system is weakened, yeast overgrowth can lead to symptoms. It is similar when the natural intestinal flora changes - this is often the case after taking antibiotics.
Duration and prognosis of a yeast infection in the intestine
Due to the unspecific symptoms, it often takes a long time before the diagnosis of the yeast infection in the intestine can be made at all. Often there is also no direct evidence, as it is not always possible to create a stool culture. The reason for this is that the yeasts are not evenly found in the stool and are not always "caught" with the stool sample. Therefore, the right therapy is often started late anyway.
In addition, this type of infection is persistent and the pathogens can still be present even after the symptoms have subsided. They sometimes go away later or can cause the infection to come back. For this reason, the medication should still be taken for a few days after the symptoms have subsided.
Another reason for a breakout can be the existing immune deficiency - in this case the temporary infection has been fought, but the basic prerequisites for this infection are still present.
One way to shorten the duration of the illness is to strengthen the immune system. To find out what to do, also read: How can you strengthen the immune system?
What symptoms do yeasts cause in the intestines?
The colonization with yeasts (also called mycosis) often goes unnoticed for a long time. And when it becomes symptomatic, the signs are often non-specific and are not primarily associated with a yeast infection of the gut.
Often there is a bloated feeling in the stomach, gas, heartburn, diarrhea or constipation - the symptoms can alternate.
It is also possible that those affected suffer from headaches, complain of exhaustion, feel excessive hunger for sweet foods and have cravings or can no longer tolerate alcohol at all.
Recurring infections of the genital area and anus can also sometimes indicate yeast colonization of the intestine.
All of these symptoms may or may not be due to yeast colonization. Due to the low specificity, it is often difficult to establish the connection between the symptom and any existing disease.
Can it still be a different species of mushroom? General information and an overview of fungal diseases can be found at: Fungal diseases
Diagnosis of yeast in the intestine
In contrast to a yeast infection of the skin or mucous membranes, the diagnosis of a yeast infection of the intestines is more difficult to make.
It makes sense to start a stool culture in the case of the mentioned and less specific symptoms. In this case, the patient is asked to give a small stool sample in a pre-given sample tube to the doctor's office. The stool sample should not be stored at home for long periods as this may distort the results. The samples should be taken from different parts of the stool, as the yeasts do not spread evenly in the stool, but form clusters.
Furthermore, attempts can be made to create yeast cultures using swabs from the mouth or anal mucous membrane.
Read more on the topic: Yeast infection
Treatment - Which remedies help against yeast in the intestine?
In the case of yeast in the intestine, drug therapy should be chosen. This often comes with antifungal agents with the active ingredient Nystatin for use.
In addition, attempts are made to support the ailing immune system, for example through microbiological therapy. In this way, the body's own defenses in the intestine should be supported and a healthy intestinal flora restored.
It can also be helpful to adhere to special oral hygiene rules, since an infection is often associated with a Candida colonization in the oral cavity. This includes good oral hygiene as well as thorough cleaning of braces, removable dentures and regular changing of toothbrushes or toothbrush heads.
Some patients also advocate immune system support agents such as pomegranate seeds, garlic or coconut oil to combat yeasts. Since a yeast infection can be triggered by a weak immune system, the approach of strengthening the immune system through food, but also through stress reduction, is not wrong.
More information at: Anti-fungal medication
How can you treat yeast yourself?
If you have yeast infections of the mucous membranes or skin, applying anti-fungal creams or gels may help.
When in doubt, a doctor should always be visited to confirm a possible diagnosis and recommend or prescribe the appropriate medication.
If organs are also affected, a doctor should be consulted in any case before any kind of independent therapy.
Everyone can only ensure that the immune system is strengthened, that one eats a balanced and healthy diet, does moderate physical exercise, is not exposed to too much stress and that basic hygienic rules are observed.
Eating natural yoghurt helps to (re) build up a healthy intestinal flora. A high-fiber diet and adequate fluid intake (water and unsweetened teas) are also recommended.
After an infection has already taken place, the focus should also be on taking hygienic measures and measures to strengthen the immune system into account in order to minimize the risk of re-infection.
You might also be interested in: Which home remedies strengthen the immune system?
Recommendation from the editor
Further information that may also be of interest to you:
- Mushrooms
- The fungal infection of the skin
- This is how the nail fungus is treated effectively
- Treatment of vaginal thrush
- How contagious is athlete's foot?