Helicobacter pylori
Summary
Helicobacter pylori is a gram-negative rod bacteria. There are more than 300 different strains that are distributed worldwide, that are regional and familial, and whose genetic information differs significantly in some cases. What they all have in common is a whole series of different adaptation mechanisms that enable it to survive in its main reservoir, the human stomach, even though it is acid-sensitive.

Symptoms
Not everyone with a Helicobacter pylori infection will notice something of the unwanted colonization of their stomach. Only 10% of those infected are affected by the secondary disease of the colonization, inflammation of the gastric mucosa (= Gastritis: gaster = stomach) or even a stomach ulcer or stomach cancer. This damage, which the germ leaves on the stomach lining, is the result of a unique property of the bacterium in the stomach, ammonia production.
Helicobacter pylori forms ammonia and other substances as a survival strategy in order to survive in the gastric hydrochloric acid and it is precisely these substances that are poison for the gastric mucosa and begin to attack it. The gastric mucosa begins to inflame in response to this stimulus and to form more hydrochloric acid. This irritates and damages the stomach lining and a vicious circle begins.
This then becomes noticeable with the gastric mucosal inflammation described above and, if left untreated, often ends in the complete destruction of the upper mucous membrane layer of the stomach and a gastric ulcer, also known technically as gastric ulcer, occurs. If the cell degenerates from the extreme irritation at some point, even a stomach tumor can develop.
It is precisely this gastric mucosal irritation that gives rise to the typical symptoms that a gastric mucosal inflammation or gastric ulcer caused by Helicobacter pylori. The inflammation creates a pain when you press your hand on the stomach (= Tenderness). This pressing pain changes with the ingestion of food and usually increases with eating, depending on where the ulcer is. Due to the increased gastric acid production, heartburn is often found at the same time as the gastric mucosal inflammation.
In addition, the gastric mucous membrane irritation often leads to nausea and vomiting. If the gastric mucosal inflammation persists for a longer period of time, diarrhea, gas and bloating occur.
In the case of sudden deterioration, the development of an ulcer should always be considered. The two scientists who were able to prove Helicobacter pylori to be the cause of gastric mucosal inflammation even received a Nobel Prize in 2005 for their discovery.
You can find much more information on our website: Symptoms of a helicobacter
Test for a helicobacter
When detecting Helicobacter pylori, a distinction is made between so-called invasive and non-invasive methods. Invasive means that you penetrate body tissue.
There are several non-invasive testing methods. This means that a colonization with Helicobacter pylori can in principle be very easily detected. One of the simplest methods is to use the patient's normal exhaled air. Helicobacter is the only resident in the stomach to have the ability from urea with the release of carbon dioxide (CO2) To form ammonia. This ability is essential for him to survive in the extremely acidic environment in the stomach.
The urea of Helicobacter pylori can easily be detected in the exhaled air, since it will never be found in healthy people. The equally simple methods include detection in the stool of the potentially infected. The antibodies that fight Helicobacter pylori in the body can also be detected in the blood count of those affected.
Since these test methods are not 100% accurate, invasive detection methods are often used despite the greater effort, above all sampling (= Biopsy) as part of a gastroscopy (= Gastroscopy). This sample is then examined in the laboratory and assessed microscopically.
You can find more information on our website: Helicobacter pylori breath test.
Diseases
Although Helicobacter pylori naturally colonizes the human stomach, infection with this bacterium can lead to various acute or chronic stomach diseases and associated complications.
Helicobacter pylori plays a role in bacterial inflammation of the stomach (B gastritis), some gastric and duodenal ulcers (Gastric ulcer, duodenal ulcer), Inflammation of the duodenum, and gastric mucosal atrophy. If the stomach is chronically infected with Helicobacter pylori, there is a risk of developing gastric cancer or a lymphoma originating from the mucous membrane-associated lymph tissue (MALT lymphoma). These are associated with high morbidity and mortality.
Since 1994, Helicobacter pylori has therefore also been in group 1 of the carcinogens (= cancer-causing substances) defined according to WHO criteria.

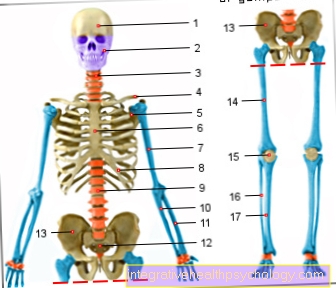
Anatomy stomach
- Esophagus (gullet)
- Cardia
- Body
- small curvature
- Fundus
- great curvature
- Duodenum (duodenum)
- Pylorus
- Antrum
infection
The transmission route of Helicobacter pylori has not been conclusively clarified. The possibility of oral-oral and fecal-oral transmission through excretion of the bacterium in the stool and re-absorption by other people, for example from the water, is discussed. Dirty food is also a source of intake.
The germ first colonizes its main reservoir in humans, the lower part of the stomach (Antrum), moves with the help of small, elongated membrane protuberances (Scourges), which are made up of spiral protein threads and function like a propeller, propagates in a directional manner and over the stomach mouth (Cardia) and the stomach body (Corpus) out.
This colonization of the gastric mucosa can take decades. The gastric environment is protected against bacteria by the aggressive gastric acid. Helicobacter pylori manages to survive for a short time due to some adaptation mechanisms in the acidic gastric juice.
Just until the bacterium attaches itself to the epithelial cells of the gastric mucosa with special adhesive structures, so-called adhesins, then penetrates them and nests in the mucus, which protects the stomach from self-digestion and, for this reason, the bacterium from gastric acid. This is a prerequisite for an inflammation of the stomach caused by Helicobacter pylori (gastritis). Inflammatory cells enter the tissue. The clinical picture is called chronic-active gastritis.
You might also be interested in: Cholera
-> Read more about Helicobacter pylori symptoms
transmission
Infection with the Helicobacter pylori bacterium is considered contagious, but not the clinical picture of gastric mucosal inflammation caused by Helicobacter pylori. It is assumed with great certainty that the transmission took place in most of those affected in childhood, when the immune system is not yet sufficiently efficient to fight the germ.
Likewise, the path of transmission itself, in addition to age at transmission, is still the subject of current research. It is suspected of being transmitted through mouth-to-mouth contact or through the feces of people who harbor it in their stomachs and then excrete it with the digested food.
Mouth-to-mouth transmission, for example, would typically take place by placing a child's pacifier or spoon in the mouth. Transmission through feces would mean that it is sufficient for an infection that the person concerned does not wash their hands sufficiently after using the toilet and that the germ can then adhere to the hands and then get into other people's digestive tract through contact with food or direct mouth contact . It can then nestle there and be passed on to other people via the same mechanism through excretion with the feces.
A transmission of the animals has been ruled out to date. In Germany alone, germ colonization can be demonstrated in many millions of people. It is assumed that around 50% of the world's population are affected. The infection rate differs greatly according to age, geographical point of view, ethnicity and social class (i.e. Housing situation, income, job).
Once Helicobacter pylori has attacked the stomach, over time it colonizes the entire gastric mucosa and often romps there unnoticed for decades. It only causes complaints in about 10% of the people affected and in an even smaller proportion it triggers an inflammation of the gastric mucosa by irritating the mucous membrane cells.
Virulence factors
Still in production Helicobacter pylori urease, an enzyme that splits urea into ammonia and CO2. This increases the pH in the bacterium's surrounding medium, i.e. it is converted into a less acidic environment.
The neutral milieu is called the ammonia coat. Helicobacter pylori also produces virulence factors such as vacuolating VacA and cagA. The VacA toxin has a variety of roles. Among other things, it forms vacuoles in gastric epithelial cells, induces the suicide of cells (Apoptosis) and inhibits special defense cells of the immune system (T-Lymphocytes).
It probably also plays a role in the development of secondary diseases that is not yet understood. The VacA is produced by about 50% of the Helicobacter pylori strains.
The cagA protein can be introduced into the epithelial cells of the stomach from the bacterium. It binds to structures and changes signaling pathways that have cell growth and migration properties. According to the results of some studies, cagA could induce secondary diseases and even be directly involved in tumor development.
Diagnosis

There are invasive and non-invasive diagnostic methods to detect Helicobacter pylori. In the invasive methods, the upper gastrointestinal tract (Gastrointestinal tract) examined.
The tissue samples taken (Biopsies) of the stomach lining are examined in different ways. In the enzymatic rapid test, the already mentioned enzyme reaction by urease is used. This test is called the Helicobacter urease test (HUT). Furthermore, one looks for bacteria under the microscope, creates a bacterial culture and examines it for Helicobacter pylori using molecular genetic methods such as the polymerase chain reaction, which can reproduce genetic material of the bacterium. With the help of the culture or the HUT, living pathogens can be detected. The non-invasive diagnostic methods do not require tissue removal using endoscopy, but are nevertheless suitable for detecting Helicobacter pylori in the stomach. The CO2 produced by the urease reaction can be detected in the breath with the help of a breath test (Urea breath test).
A special test can test the patient's stool for Helicobacter pylori components that are recognized by the organism as foreign and combated by the immune system (Antigens), examine.
Some other test methods determine antibodies against Helicobacter pylori in the patient's blood, urine or saliva, but cannot make a stand-alone statement about the current level of infection, but only in connection with the patient's medical history (= medical history).
The Helicobacter pylori urease rapid test as part of an endoscopy is now part of the routine examination if a Helicobacter pylori infection is suspected with an abnormal endoscopic finding.For check-ups after a therapy, as well as patients with unclear upper abdominal complaints without additional symptoms, a urease test is carried out if an endoscopy is not used. In epidemiological studies, antigen-antibody reactions in the blood (serology) tested.
The detection methods therefore differ based on various previous histories of patients with an existing chronic Helicobacter pylori infection or suspected initial infection and with regard to therapeutic intervention.
You might also be interested in these articles:
- Helicobacter pylori breath test
- Urease Fastest
Re-infection
Reinfections are rather rare and occur in around 1% of those affected after successful treatment.
treatment

Without treatment, the infection lasts for life. This is generally not a problem as long as there is no gastric mucosal inflammation or other risk factors that can be held responsible for additional damage to the gastric mucosa.
A purely prophylactic (= preventive) Therapy is no longer recommended today, contrary to what was previously common practice. It is only recommended in medical guidelines if a sequela occurs, known family members with a stomach tumor, after removal of parts of the stomach, if the stomach tumor is healed or during long-term therapy non-steroidal pain relievers like ibuprofen or diclofenac as well Glucocorticoids, the cortisol.
The process of eliminating the germ is called Eradication. The typical therapy consists of a combination of mostly 2 different antibiotics and an additional one Proton pump inhibitors. This therapy then takes about 7-10 days. Depending on which scheme the doctor chooses, one speaks of the Italian or French triple therapybecause three drugs are used to treat it. These schemes are only the most frequently used combination options, but there are many more that are then used in individual cases. Since the bacterium can no longer be killed by many of the usual antibiotics, it is often necessary to try several combinations of antibiotics and the duration of therapy can stretch over up to 8 weeks. The therapy is only considered successful if no bacteria can be detected in another gastroscopy after several weeks.
Proton pump inhibitors
Proton pump inhibitors are always part of the treatment of Helicobacter pylori. Proton pump inhibitors block a special structure in the gastric mucosal cell, the so-called proton pump, which is responsible for the production of stomach acid, i.e. hydrochloric acid. This re-establishes the balance of aggressive acid and protective gastric juices caused by excessive gastric acid production and allows the stomach to recover from the damage and inflammation.
Side effects on the gastrointestinal tract are very common, as the digestion of food is changed in that the digestion in the stomach cannot begin as usual. Various effects can be felt here, from constipation to diarrhea, nausea and vomiting as well as flatulence.
Much more information can be found under our topic: Eradication of the Helicobacter
Due to the metabolism in the liver, the Liver valuesthat are determined by default when blood is drawn. It mostly comes to increased liver values. In most cases, however, these values will decrease again after the end of therapy and only in extremely rare cases can liver inflammation (=hepatitis) occur.
Occasionally, symptoms such as dizziness, headache, tiredness or sleep disorders occur. However, these symptoms usually improve in the course of therapy and should not lead to immediate discontinuation of use.
Long-term use is at higher risk for the moment osteoporosis discussed, in the context of which an increased rate of hip or Vertebral fractures supposed. Visual and hearing disorders are extremely rare and usually only occur directly in the blood vessels after treatment, i.e. not as a tablet, as part of hospital treatment. If those affected notice these side effects, the doctor treating them should be informed.
Antibiotics
Among the antibiotics there are different types and substances that are used in the treatment of Helicobacter pylori. The various combinations struggle with many these days Resistances of the germ, so that it is not uncommon for several combinations to be tried before the therapy is successful.
The antibiotic is used very often Clarithromycin. Clarithromycin is part of a group of antibiotics called one Macrolides is called. These hinder the production of proteins in a bacterium that are essential for the bacterium's life. It is known to many from the treatment of respiratory infections, such as one bronchitis, one lung infection (= Pneumonia) or from the treatment of Otitis media (= Otitis media) , Tonsillitis or Inflammation of the sinuses be. Side effects can Nausea, vomiting, diarrhea, dizziness, insomnia or Hypersensitivity reactions and should be read in the instruction leaflet.
The antibiotic is also often used Amoxicillinthat belongs to the group of Aminopenicillins heard. This group is very close to the classical ones Penicillins related and inhibits the build-up of the outer shell of bacteria. In addition to its use in Helicobakter pylori infections, it is also used in infections of the Digestive tract, of the Biliary tract, of the Urinary tract or how clarithromycin in various infections im Head and neck area as well as the respiratory tract applied.
Patients with a Penicillin allergy should also refrain from amoxicillin therapy if possible. However, as with any drug, side effects can always occur and usually include Disorders of the gastrointestinal tract such as nausea, vomiting, or diarrhea. If side effects occur, a doctor should be consulted to jointly consider whether a change of antibiotic makes sense.
The last most commonly used antibiotic in the treatment of Helicobacter pylori infection is Metronidazole from the group of Radical generator. These form small aggressive molecules, the radicals, which make up the genetic material of the bacterium, the DNA, harm and allow the bacteria to perish. Human genetic material can be caused by the radicals not harmed become. The antibiotic is ideal for the treatment of various intestinal germs and, in addition to the treatment of Helicobacter pylori, also helps Intestinal infections or Infections in the genital area or in the urinary tract for use. While taking metronidazole is the Refrain from alcohol especially important because if taken at the same time, the accumulation of toxic substances can lead to serious consequences. Metronidazole, like many other antibiotics, can too Indigestion, headache, dizziness, paresthesia, discoloration of urine and allergic reactions lead, if it occurs one should always consult a doctor.
Healthy behaviors can also improve and alleviate the symptoms of those infected. All lifestyle recommendations are preceded by a balanced lifestyle Avoidance of stress as a major factor in increased gastric acid production. Stress applies alongside the emergence of Heart attacks also as a big factor in creating one Inflammation of the stomach lining. If stress reduction is not possible, learning various relaxation techniques can be helpful.
When it comes to nutrition, it is also important to adhere to the tips listed below. Since food, like the presence of Helicobacter pylori, is one of the greatest stimuli for gastric acid production, optimal nutrition can also have a major influence on the course of gastric mucosal inflammation. Either is recommended for the first painful days of an inflammation of the stomach lining complete fasting or a very Easily digestible, low-fat, mild whole food. Are very suitable for these days Oatmeal bananas, rusks and vegetable juices.
A gentle diet should then be continued throughout the course of therapy. Foods that are difficult to digest and high in fat lie in the stomach for a long time and lead to much more gastric acid production than light products that can be digested quickly in the rest of the digestive tract. So on the list of foods that shouldn't be eaten are sour citrus fruits (the harmful ones through the fruit acid PH value the stomach acid maintained), cheese, cream, fatty sauces, Fried, cream but also Sweets. Flatulent foods like lenses or Cabbage should also be avoided, as the gastric distension caused by the gases formed also stimulates gastric acid production. In the case of vegetables, digestible varieties are like Carrots, zucchini or lettuce instead of choosing legumes. Vegetables cooked beforehand become more digestible. Likewise with fruit Bananas, apples, pears and apricots rather than strongly acidic oranges or lemons, preference is given.
The meals should be divided into several small instead of a few large meals in order to reduce the stretching as a stimulus for gastric acid production. If the inflammation lasts longer, this diet should be maintained. Various drinks can also increase gastric acid production and should therefore be avoided. First and foremost are the drinks that have already been mentioned several times Alcohol and coffee. Similar to the bloating cabbage should also highly carbonated drinks not be drunk, as the gas stimulates gastric acid production by stretching the stomach. Strongly acidic fruit juices like orange juice humiliates him too PH value in addition to stomach acid and should therefore also be avoided.
In principle, anything can be eaten that does not cause any complaints. According to this simple principle, the diet can also be structured towards normal diet in the later course.
Prevalence

Helicobacter pylori infection is the second most common bacterial infectious disease in humans. The prevalence is much higher in developing countries than in industrialized countries. Worldwide, 50% become infected with Helicobacter pylori, but not everyone develops one Inflammation of the stomach lining. The majority of Helicobacter pylori infections are asymptomatic. Even unspecific symptoms, such as Upper abdominal pain or heartburn may occur. The contamination increases with age. Every second person aged 50 and over has Helicobacter pylori Inflammation of the stomach lining.
Although some pathogenetic mechanisms of each Helicobacter pylori strains are known and understood, it is still not clear which strain causes sequelae and how Gastric ulcer (ulcer) and Stomach cancer (gastric cancer) can be triggered and which patients develop them or remain asymptomatic for life.
history
Helicobacter pylori was first described by two Western Australian researchers named Barry Marshall and John Robin Warren in 1983. It was not until 2005 that they were awarded the Nobel Prize for Physiology or Medicine, often popularly known as the Nobel Prize for Medicine, for their discovery. The name of the bacterium was also found Campylobacter pylori and others only in 1989 its name still valid today: Helicobacter pylori. The German doctor and researcher Robert Koch laid the foundation stone for the discovery of the bacterium as early as the 19th century when he succeeded in growing bacteria in culture and, viewed under the microscope, bringing them into a causal relationship with infectious diseases with bacteria as pathogens.
It was previously assumed that gastric juice would not allow any harmful pathogens in the acidic environment and, among other things, made psychological influences jointly responsible for the development of gastric and intestinal ulcers.
prophylaxis
The development and use of possible vaccines against infection with are frequently discussed Helicobacter pylori. Due to the high infection rate, the unpleasant symptoms when the inflammation breaks out and the complications associated with it that can be caused by a Helicobacter pylori infection, such approaches are very important and topical. However, no breakthrough in the development of a vaccine has yet been achieved, and premature hope for an early use is warned.