Meningitis
synonym
meningitis
definition
Meningitis is an inflammation of the das caused by bacteria or viruses brain spanning Meninges with sometimes life-threatening consequences.

causes
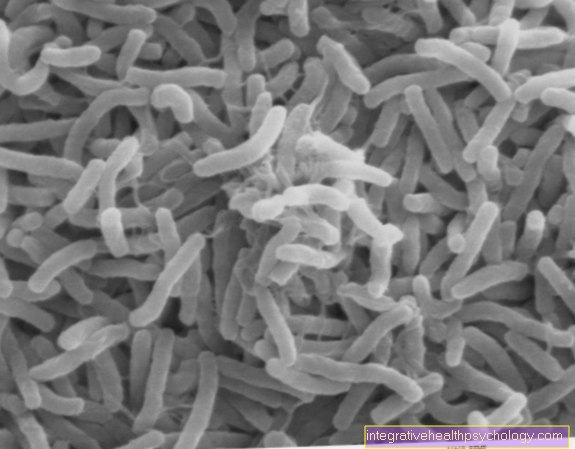
There are numerous pathogens, such as Viruses or bacteria that get into the body and either go unnoticed there for a certain period of time or can lead directly to an infection of the meninges. E.coli, streptococci, listeria, meningococci, Haemophilus influenzae, pneumococci or Neisseria should be mentioned.
Find out more about the topic here: Meningococcal vaccination
There are also numerous hospital germs with which patients on wards can become infected. These include Pseudomonas aeruginosa, staphylococci and enterobacteria. Patients who are already immunocompromised by medication or a previous illness also have an increased risk of developing meningitis caused by listeria or cryptococci. In addition to bacteria, numerous viruses can also lead to meningitis. Coxsackie, echo or mumps viruses, but also measles, cytomegalovirus and the TBE virus are among the most common pathogens.
In rare cases, "Still's disease", a rheumatic disease, can also be the cause. For the most important information, read the article under: Still's disease - what's behind it?
What are the first signs of meningitis?
As a sign of meningitis, the occurrence of classic three symptoms fever, Headache and neck stiffness rated.
Accompanying nausea or vomiting can be seen as signs of increased intracranial pressure in the context of meningitis and represent a medical emergency.
While Fever and headache also with many other infectious diseases occur is the Neck stiffness typical for the presence of meningitis.
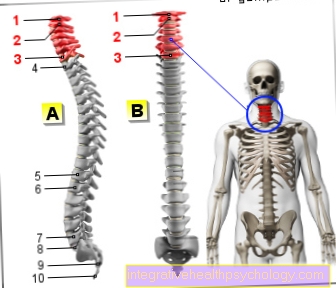
The Movement of the head is severely restricted and takes place in pain. The treating person is used to determine the stiffness of the neck doctor several Investigation methods. The patient reacts reflexively to a head movement by pulling in the knees (Brudzinski sign). Alternatively, bending the legs with the knees straight leads to bending the knee joint (Kernig's sign). These reflex-like movements of the patient are due to the additional tension in the area of the meninges that surround the spinal cord as well as the brain.
Symptoms
Most often, patients in poor general health seek medical attention. The most common symptom of meningitis is headache. Sensitivity to light is also regularly described. Nausea and vomiting as well as high fever may or may not occur. Other neurological complaints such as dizziness, double vision, movement disorders or feelings of numbness tend to occur less often and usually only when the clinical picture is very advanced. Neck stiffness is very commonly reported, i.e. the head cannot be bent forward passively or only with severe pain. These symptoms occur in a weakened form with meningeal irritation.
Read more on the topic: Meningitis symptoms and meningitis signs and fever, dizziness and headache
fever
As one of the classic symptoms meningitis occurs fever on. The increased body temperature is a defense reaction of the body in order to be able to fight invading bacteria and viruses.
The amount of the Fever varies depending on the pathogen and patient. While an infection with a virus tends to produce a mild fever, bacterial infections can lead to a very high fever within a short period of time. Meningitis can occur in young children and infants even without a fever. Instead, these children are primarily characterized by a poor general condition.
a headache
The most common symptom of meningitis is a headache. Due to the sensitive supply of the meninges through nerve fibers, inflammation occurs in the area of the meninges Irritation of nerve fibers and severe, localized headache. These often occur in the back of the head and go with one painful neck stiffness hand in hand.
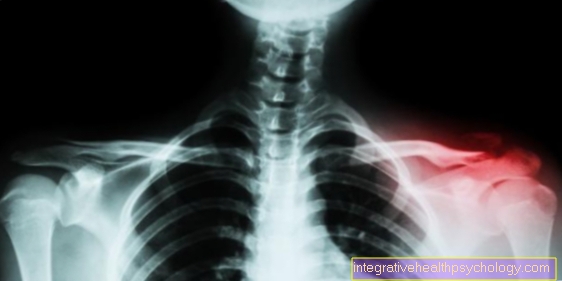
Neck stiffness
Another classic symptom of meningitis is that Neck stiffness. Compared to the other symptoms mentioned, which also occur with many other diseases, is the neck stiffness typical of meningitis.
The patient can only move his head to a limited extent or with pain. Especially the Movement of the head towards the sternum causes severe pain, as this movement also tensions the meninges. An examination in which the doctor passively lifts the patient's head up to the sternum causes the patient's knees to reflexively tighten to reduce pain, a phenomenon known as the Brudzinski sign.
Nausea and vomiting
The three classic symptoms of meningitis are often caused by Nausea and vomiting accompanied.
Due to the inflammation caused increased intracranial pressure different centers, i.a. the vomiting center in the area of the brain stem become irritated. As a result it comes to nausea with sometimes difficult Vomit. This is a clinical emergency because the increased intracranial pressure other centers in the brain area can become irritated and pinched. With the help of imaging, in this case computed tomography (CT) of the head, increased intracranial pressure can quickly be ruled out.
How contagious is meningitis?
During a Meningitis itself is not contagious is, they can causing pathogen from person to person be transmitted. The Type of transfer e.g. via the air, saliva, contact, sexual intercourse or ticks, depends on the respective pathogen. Often these pathogens are initially too responsible for another clinical picture and only later lead to the development of meningitis. An infection with the pathogen without developing clinical symptoms is also possible.
Some Viruses and bacteria are transmitted via small droplets of secretion that come from the human respiratory tract and saliva and from other people via the Breathing added become (droplet infection). Most of the pathogens that cause meningitis, including Herpes viruses, meningococci, pneumococci and Haemophilus influenzae.
Other viruses and bacteria are transmitted via ticks and are therefore not infectious from person to person (e.g. Borrelia, TBE virus). Many other forms of infection are possible.
How dangerous is meningitis?
Meningitis can cause meningitis, especially when infected with bacteria severe course to take. The The prognosis depends on the general condition, the immune system and the Age of the patient. The earlier therapy with antibiotics is started, the sooner serious and sometimes life-threatening consequences for the patient can be avoided.
At a The inflammation spreads to the brain tissue are many neurological disorders and failures possible. Disturbances in consciousness, general restlessness, seizures and hearing disorders can occur. In extreme cases, it can also lead to paralysis.
This is a dreaded complication of meningitis Waterhouse-Friedrichsen Syndrome. It occurs primarily in the event of untreated infection with the meningococcus bacterium. The spread of the bacterium through the bloodstream throughout the body (sepsis) causes severe damage to the blood coagulation system. A Multiple organ failure is possible.
From Waterhouse-Friedrichsen Syndrome toddlers and young adults, in whom the immune system is not yet fully developed, are particularly affected.
diagnosis
The suspected diagnosis is made after the patient has one or more symptoms that are typical of meningitis. The medical survey is also important. The patient should always be asked about recent long-distance trips or stays in meningitis areas or whether in the past Tick bite was present. The sudden active flexion of the knee with passive flexion of the head is one of the meningitis signs with an urgent suspicion of this disease. If these so-called meningitis signs are positive, a neurological evaluation must urgently be carried out on the patient. A detailed blood count is then usually done in the hospital. The inflammation values such as CRP or leukocytes are particularly important. A massive increase strengthens the suspected diagnosis of meningitis. The next diagnostic measure is the examination of the cerebrospinal fluid, the so-called CSF punctureIt may only be carried out when increased intracranial pressure has been ruled out. This is done with a reflection of the fundus. If the optic nerve is arched forward, an increased intracranial pressure can be assumed, which prohibits the CSF puncture. If the optic nerve is normal, the liquor puncture can be performed.
therapy
Once meningitis has been diagnosed, symptomatic and therapeutic treatment must be started immediately. Therapeutically, antibiotic therapy must usually be started by infusion, which is based on the detected pathogen. So-called 3rd generation cephalosporins (cefotaxime, ceftriaxone) are mostly used. This treatment is supplemented with ampicillin. The duration of treatment should not be less than 10 days. Intensive monitoring of the patient is essential. The symptomatic treatment of the patient includes an adequate treatment Pain management also controlling intracranial pressure. If this increases as a complication of meningitis, treatment with cortisone should be started immediately. Furthermore, regular blood tests should be carried out, which should immediately indicate electrolyte imbalances.
Duration of meningitis
Of the Course and duration of meningitis varies strong depending on the trigger Pathogen. At bacterial infection it often comes to one severe course. The first symptoms appear approximately 2 to 5 days after infection with the bacterium (incubation period). During this period, the bacterium spreads and multiplies in the body without the patient noticing the infection. The infection with a certain is a specialty bacterium represent the Meningococciin which the incubation period can last up to 10 days. As a result, the infection often takes a very severe course that can be life-threatening.
At viral infection the disease usually takes a milder course. Depending on the virus, the time it takes for the first symptoms to appear differs greatly (incubation period). The incubation period varies between 2 and 14 days. The result is a course in which the symptoms typically include a slight fever, headache and stiff neck for a few hours to several days occurs. In patients with a functional immune system, the symptoms then subside without further therapy.
A special feature is the course of meningitis when infected with tuberculosis bacteria. The incubation period is between 2 to 8 weeks. The infection begins slowly over several weeks with repeated attacks of fever.
What are the consequences of meningitis?
The consequences of meningitis are depending on the pathogen and from the time of Commencement of treatment.
Without treatment consists of Risk of further spread of the pathogen to the Brain tissue and about the blood circulation throughout the body. When the brain substance is transferred (meningoencephalitis), disturbances of consciousness up to coma and psychological symptoms, such as general restlessness and seizures, are possible. The risk of damage to cranial nerves can lead to hearing impairments, among other things.
While the disease usually takes a milder course when infected with viruses, often heals on its own and has hardly any consequences for the patient, when bacteria are infected there is a risk of spreading throughout the body. Without treatment is meningitis caused by bacteria triggered, often fatal. In the case of treatment with antibiotics, the further course depends on the general condition, the condition of the immune system and the age of the patient.
Consequences of meningitis from a tick bite
Ticks can transmit various pathogens that lead to different diseases in humans.
On the one hand, the transmission of the TBE virus (early summer meningo encephalitis) is possible. The TBE virus can spread to the central nervous system in the first few days after the appearance of flu-like symptoms. There is a risk of meningitis with attack on the brain substance, a so-called meningoencephalitis.
Without further treatment, there is a risk of neurological failures (e.g. paralysis) due to damage to the nerve cells and fibers. That is why vaccination against the TBE virus is recommended in large parts of Germany.
On the other hand, borreliosis can also be transmitted by ticks. After typical reddening and infection of the skin in the area of entry after a few days to weeks, the pathogens can also spread to the central nervous system here. Meningitis with damage to the cranial nerves is possible after several weeks to months without treatment with antibiotics.
Read more on the subject at: What can be the consequences of a tick bite?
Consequences of meningitis caused by herpes viruses
Herpes viruses are the most common infectious cause of meningitis.
Herpes viruses spread along nerve fibers. In addition to the typical vesicle formation in the area of the nerve supply area, there is also the risk that the virus will spread towards the central nervous system.
This can lead to meningitis, damage to the affected cranial nerves and an attack on the brain substance.
forecast
The prognosis of meningitis depends on the time of diagnosis, the type of pathogen and the patient's comorbidities. Patients with meningitis caused by meningococci die 10% of the time. With Listeria infection the death rate is even 50% and with pneumococci 25%.If the patient survives, no statement can yet be made about the consequential damage. The possibilities range from no complaints at all to severe intellectual disabilities.
Meningitis in children
The pathogens that most commonly cause meningitis in children are Haemophilus influenzae (if no appropriate immunization was carried out), meningococci in over 50%, as well Streptococci.
Meningitis is more likely to develop in children compared to adults. The symptoms, such as stiff neck, sensitivity to light as well as general condition deterioration and high fever but occur in children as well.
In contrast to babies, children usually describe the symptoms very precisely and in detail, which is helpful in establishing a diagnosis and saves important time during treatment.
Diagnosis is also carried out according to adult treatment.
Meningitis in babies
The most common pathogens for meningitis in babies are E. coli, group B streptococci and listeria. In babies, diagnosis is extremely difficult due to the lack of clear symptoms. Besides screaming and Pain signaling the babies are usually conspicuous by an extremely high fever with subsequent clouding and presented to a doctor. Unusual refusal to eat and skin discoloration with pale spots can also be harbingers of this serious infectious disease. Sometimes a bulging fontanel is a sign of meningitis in a pronounced form. In some cases, the first neurological abnormalities already indicate meningitis.
Treatment often occurs relatively late. In babies, the diagnosis corresponds to that of adult treatment. In addition to a neurological examination, cerebral water punctures and fundus imaging are also performed. For some years now, infants have been vaccinated against Haemophilus influenzae, which can also lead to meningitis, as a preventive measure. The vaccinations are repeated in the third, fourth, fifth and 12th month of life.
Meningitis from tick bite

Meningitis can be transmitted by ticks, especially between March and November, with an incidence peak in July. This is a viral infection that is triggered by the TBE virus that the ticks carry. Areas such as Russia, the Baltic States, Eastern Europe, Bavaria, Baden-Württemberg, Carinthia and the Balkans are high-risk areas. After a tick bite and virus transmission, one occurs Incubation period of 5-28 days before the disease breaks out. In 70-90% of the cases there is a so-called asymptomatic course. The rest of the way is typically bimodal Rise in fever, as well as flu symptoms. After the first defensive treatment with a corresponding improvement in the symptoms, the fever rises again with the symptoms typical of meningitis such as headache, Neck stiffness and neurological limitations. A complication can be what is known as meningoencephalitis, i.e. not only meningitis but also encephalitis. This course is highly dangerous and can also lead to death.
The diagnosis is made when the patient states that he has been in a tick area in the last few days or months or has been bitten by a tick and has symptoms typical of meningitis. A blood count is then made, which on the one hand shows the inflammation values such as CRP and leukocytes, but also includes a pathogen determination. The treatment is carried out with doxycycline as an antibiotic, whereby the duration of treatment should not be less than 2 weeks. The most important measure to prevent TBE meningitis is to protect and prevent infection.
Particularly in risk areas, arm and leg covering clothing should be worn during the endangered seasons. The use of Insect repellants be helpful. If a tick bite occurs, the tick should be removed immediately and the bite site disinfected. It is important to ensure that the tick is completely removed from the skin. Special tick tongs that can be bought in pharmacies are suitable for this. If parts of the tick remain in the skin, the risk of TBE transmission is reduced.
After a tick bite, the skin area should be observed accordingly. A circular reddening around the bite site could mean the onset of Lyme disease. Appropriate antibiotic treatment should definitely be started in this case. For people who live in high-risk areas and who are often out and about in forest areas, consideration should be given to having an appropriate vaccination carried out in advance. After a tick bite, vaccination makes no sense, as a TBE infection that has developed here can no longer be stopped.
Can meningitis occur without a fever?
In rare cases can meningitis even without a fever occur. Especially with Children meningitis occurs often not symptomatic and in rare cases can occur without a fever. Meningitis without fever has also been reported in older people.
At a Virus infection, which leads to meningitis, usually only develops one mild fever (just over 38 ° C). There is a risk that the meningitis will not be recognized or misinterpreted.
Vaccination against meningitis
The so-called TBE vaccination is the only vaccination against viral meningitis. It is primarily intended for people who are in high-risk areas such as Bavaria, Baden-Württemberg, Russia, the Baltic States or Eastern Europe and who are often in forest areas. This vaccination is just as advisable for forest workers and foresters as it is for hikers and regular forest walkers. The TBE vaccination is a Active vaccination a dead vaccine. Here, killed pathogens are injected into the muscle, whereupon the body then reacts with the formation of antibodies. In the case of an actual infection with the pathogen, e.g. After a tick bite, the prepared immune system can start the immune response and destroy the invading pathogen.
The basic immunization of the TBE vaccination consists of 3 partial vaccinations. After approx. 3 years, the booster should be carried out.
There are also vaccines that need to be refreshed every year. The corresponding manufacturer approval must be observed here. Like any other vaccination, the TBE vaccination has associated risks and side effects. Due to the deadly vaccine, the feared excessive immune reactions of the body are rather small. In some rare cases, however, an allergic reaction can occur. However, inflammatory reactions in the skin area of the puncture site with reddening and swelling are relatively common. Pain in arm movement can also occur days after the vaccination. The arm should be spared. Sometimes, after the vaccination, there are mild flu-like symptoms with a slight fever and malaise. These symptoms should then go away completely within a few days.
The vaccination was developed purely to prevent TBE. Neither treatment can be carried out with a vaccination, nor does vaccination after a recent infection make sense. After a tick bite, it makes more sense to check the other vaccination protection such as tetanus and diphtheria and should then be done if necessary.
Babies and toddlers have been vaccinated against for several years Haemophilus influenza, a pathogen that can also cause meningitis. The vaccination is carried out in the third, fourth, fifth and 12th month of life and is then sufficient for the rest of life. Please refer: Vaccination against meningitis. Together with a TBE vaccination from the age of 6, the greatest risks of meningitis can be reduced. Infection with one of the numerous other pathogens is not excluded.