Horner Syndrome
Symptom complex
The Horner syndrome is expressed by three defined symptoms (Triad of symptoms).
These symptoms are:
- Constriction of the pupil (Miosis),
- Drooping of the upper eyelid (Ptosis) and
- Sinking of the eye into the eye socket (Enophthalmos).
These eye symptoms are accompanied by impaired perspiration in the upper halves of the body. Horner syndrome is not a disease in its own right, just a symptom (sign) of a disease.
However, certain nerves show certain damage. This damage can be localized in different parts of the body and can be caused by a number of pathological processes. An innate form of the Horner triad is also known.

Recognizing Horner Syndrome
Living with Horner Syndrome.
The pupil on the affected side is smaller than that on the opposite side, the lid hangs down a little and can only be lifted slightly. While the pupil normally reacts to the incidence of light with a constriction, the (miotic) The pupil in Horner's syndrome is normal with narrowing to light, but it dilates more slowly and only incompletely when it darkens.
For more information on the pupillary difference, see Different sized pupils.
A paralysis of the radial muscle cells of the iris (Dilator pupillae muscle) is causally responsible for this pupil constriction.
The paralysis of the upper eyelid muscle (Tarsalis muscle) leads to the drooping of the upper eyelid (= ptosis).
Enophthalmos of the eyes means the sinking back of the eyes into the eye socket (Orbit) while the disturbed sweat secretion is caused by damaged nerve fibers that control sweat release in the body area. The uneven sweat secretion can be clearly seen on the skin.
How is Horner Syndrome diagnosed?
With cocaine eye drops on the pupil and the lack of pupil dilation, the cord lesion of the sympathetic nerves is detected.
The subsequent administration of amphetamine eye drops can further narrow down the localization of the damage. The diagnosis is then made by the ophthalmologist using the clinical signs.
Then it is examined where the damage is and what the trigger for the damage is.
When Horner's syndrome is accompanied by other signs of brainstem dysfunction, such as:
- hemiplegia,
- Double images,
- Difficulty swallowing or speaking,
so the location of the damage can be clearly determined. A circulatory disorder can be assumed if the symptoms develop very quickly.
Magnetic resonance imaging of the head is advisable to rule out a tumor disease or a disturbance of the blood flow. Cardiac arrhythmias can be detected by ultrasound examinations of the heart and the neck vessels and a long-term EKG.
If the Horner syndrome is accompanied by signs of syringomyelia (disease of the spinal cord) and there is therefore pain or paralysis in the arms and a reduced feeling of pain, it can be assumed that the nerve fibers are also affected there.
Syringomyelia would show up on an MRI of the cervical spine.
If Horner's syndrome occurs after an accident and if there is paralysis and / or sensory disorders in one arm, damage to the arm-nerve network can be assumed. It is through these possible side effects that the doctor makes the decision for further examinations
Treating Horner Syndrome
How is Horner Syndrome treated?
A treatment of the Symptom Horner syndrome does not exist. However, treating the causes can reduce the signs of Horner's triad. However, if there is a complete severance of the nerve pathway, complete recovery of symptoms cannot be achieved.
Prevention of Horner Syndrome
What are the causes of Horner syndrome?
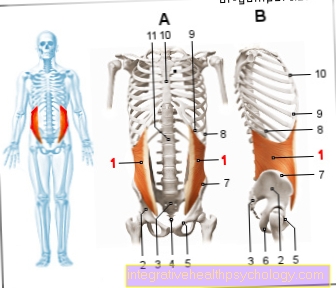
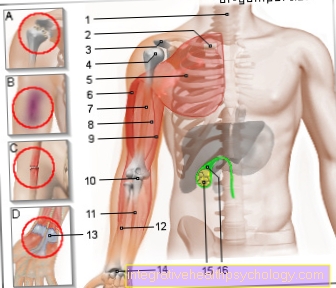
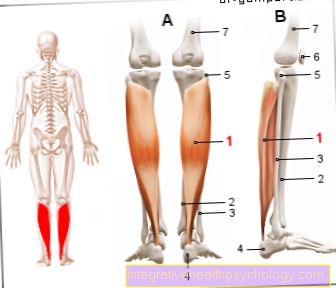
The nerve fibers that control the enlargement of the pupil and the width of the eyelid and the sweat formation in the upper half of the body belong to the so-called sympathetic nervous system, which is part of the autonomic nervous system.
The nerves in the head and neck area are very complicated and have their control center in the brain stem (see also: Stellate ganglion). From there, fibers run down into the spinal cord of the neck.
As part of a blockade of the stellate ganglion, Horner's syndrome also occurs. Please also read our article on this: Stellate ganglion blockage
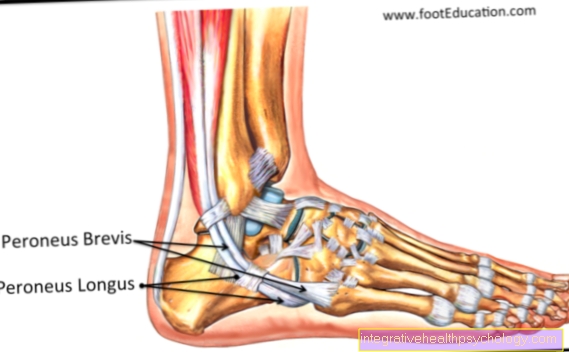
The fibers emerge from the spinal cord through the eighth cervical nerve root and form the first thoracic nerve root on one side of the body. The nerve fibers pull on to the inner carotid artery through a plexus of nerves called the cervical trunk (Internal carotid artery) and follow this vein in its forks through the middle cranial fossa to the eye.
From this tortuous and long course of the nerves it follows that the Horner syndrome can theoretically arise on the entire way from the brain stem to the eye through a pathological process.
The nerve tract in the brain stem can be damaged by a circulatory disorder, usually in the context of a Wallenberg syndrome combined with sensitivity disorders and cranial nerve failure or, rarely, by a tumor.
A pathological cavitation (Syringomyelia) in the cervical marrow can damage the nerve fibers there. From a cancer of the upper apex of the lung (Pancoast tumor) the trunk itself is often damaged. However, a so-called plexus lesion, i.e. an injury to the arm-nerve plexus (e.g. in a motorcycle accident) in the area of the cervical spine, can lead to the development of Horner's syndrome. In addition, inflammatory changes or tumors in the middle fossa can damage the nerve fibers.
Course of a Horner syndrome
What are the consequences of Horner syndrome?
ly the eye symptoms are impairing for the person concerned. The disturbance of the pupillary reflex in particular clearly limits the perceptual behavior of the eye.
The drooping of the eyelid also narrows the field of vision (visible area of the eye) and worsens three-dimensional vision. It is also important that the Horner syndrome is also very psychologically stressful for the patient, because their facial expressions change.


















.jpg)