Corneal inflammation (keratitis)
introduction
Corneal inflammation is rarer than conjunctivitis. On the other hand, this can impair eyesight in the long term, making corneal inflammation more dangerous than conjunctivitis.
Normally, an intact cornea is protected by its natural defenses, so that an undamaged cornea does not usually cause inflammation.
For general information on the subject of "inflammation of the eye" please also read: Inflammation of the eye
.jpg)
diagnosis
A slit lamp is used to shine into the wide-open eye.
It looks for whitish ulcers in the cornea. Pus can also be seen in the anterior chamber between the cornea and iris.
causes
- Wearing contact lenses too often / too long or poorly fitting contact lenses
- Herpes viruses
- Fungal infections
- dry eyes (= increased friction)
- Insufficient eyelid closure (= drying out of the cornea)
- Irritation / injury from foreign objects
- Rheumatic diseases
How contagious is corneal inflammation
In many cases, there is an infection with germs that can lead to corneal inflammation. Anyone who has corneal inflammation caused by germs is contagious for an average of two weeks after the onset of the disease and can carry the bacteria, viruses or fungi on. This is done simply through the tear fluid. Therefore, one should refrain from rubbing the eyes so that the infectious tear secretion that one finds on the hands is not transferred when shaking hands or touching objects. Frequent hand washing can also help prevent spreading.
However, there are also non-infectious causes of corneal inflammation, such as dry eyes, which can also irritate the cornea. Since there are no germs as the cause, no infection is possible. Nevertheless, one should still pay attention to the correct hygiene.
Symptoms of corneal inflammation
_2.jpg)
Typical signs of corneal inflammation are:
-
burning pain
-
Red eyes
-
Foreign body sensation in the eye: usually the feeling of rubbing sandpaper or grains of sand in the eye is described
-
Photophobia (photophobia)
-
Formation of tears or other secretions and mucus
While conjunctivitis does not affect vision, corneal inflammation can cause a deterioration in vision. In the worst case, it is even possible for blood vessels to form in the eye or for fluid to accumulate, which in the long term can lead to blindness or an ulcer.
A distinctive symptom of almost any inflammation is pain. With corneal inflammation, the uppermost layer of the cornea is irritated or damaged, which means that the nerve endings on the surface are free, which leads to the painful abnormal sensations.
Read more on the topic: Eye pain
forecast
As soon as the suspicion of a Corneal inflammation an ophthalmologist should be consulted immediately.
The infection must be detected in good time so that eyesight can be preserved and targeted treatment can be carried out.
After corneal inflammation, scars often form, which can lead to permanent impairment of vision.
How long does corneal inflammation last?
The duration of therapy may vary depending on the severity of the inflammation and the timing of treatment. Usually, however, adequate treatment takes anywhere from a few days to two to four weeks.
Contact lens wearers should not wear the lenses, at least for the duration of the treatment. If hygiene is inadequate, contact lenses are a breeding ground for germs. For the future, you should also ensure that the disinfectant liquid and the lens container are changed regularly.Thorough hand washing is recommended before inserting and removing the lenses so that the cornea does not develop again.
In the worst case scenario, blindness or other impairment of the eye can occur, which is irreversible. Therefore, going to the doctor early is of enormous importance for the therapy and thus also for the duration.
Corneal inflammation therapy
Depending on the cause, the different forms of corneal inflammation require (Keratitis) different therapies:
Corneal inflammation caused by bacteria (Bacterial keratitis)
Most infection-related inflammation of the cornea is caused by bacteria.
The most common pathogens are staphylococci and pneumococci; the cornea is particularly at risk when infected with Pseudomonas aeruginosa. To treat bacterial corneal inflammation, an antibiotic eye ointment is often prescribed, such as: B. Floxal eye ointment.
Except for exceptions such as Gonococci, which can cause severe infections in newborns, usually have to damage the surface of the cornea for a bacterial infection so that the pathogens can penetrate the cornea.
Bacterial corneal inflammation is the most common for this reason due to contact lenses, damage to the cornea, weakened immune defense or inflammation / obstruction of the tear ducts.
When the cornea is infected by bacteria, the patient often notices sensitivity to light, eyelid cramps and severe pain.
The conjunctiva is also very red.
The ulcer on the cornea seen during the examination is visible as a depression and usually has a grayish color with a surrounding ring wall.
Often there is also pus in the anterior chamber of the eye and can be seen behind the cornea as a whitish-yellow deposit on the lower edge (Hypopyon).
In the worst case, the corneal ulcer can break inward, leading to an opening of the cornea (Perforation, perforating ulcer) is coming.
The aqueous humor, which is located in the eye chambers, flows out through it and the iris (iris) lies down in the opening.
However, even without opening the cornea, if the cornea is severely inflamed, the iris can stick to the cornea and the intraocular pressure can increase, known as glaucoma.
As an examination, a short eye test is carried out after the anamnesis, the eye is examined and the cornea is smeared, which is sent to the laboratory.
There the pathogen can be examined and then treatment with specifically suitable antibiotics, e.g. with Refobacin®.
Since corneal inflammation can have massive consequential damage, it is recommended, before the exact pathogen has been identified, to start antibiotic therapy with standard preparations in the form of eye drops, which are effective against many types of bacteria. It can also be useful to inject antibiotics under the conjunctiva. As soon as the results of the laboratory examination are known, the selection of antibiotic drugs can be adapted to the exact pathogen.
Except in the case of an infection with Pseudomonas, additional therapy with cortisone is not allowed.
In very severe cases, when an opening (perforation) of the cornea is feared or has already occurred, an emergency corneal transplant may be necessary.
This is also possible with scars in the cornea from previous inflammation.
Which eye drops help?
Depending on the cause of the corneal inflammation, a doctor will prescribe the appropriate eye drops. A conventional moisturizing preparation can be used for dry eyes. The drops should help to put a protective film on the eye. However, if the cause is a pathogen, eye drops must be combined with certain medications. An antibiotic is used for bacteria, an antifungal agent for fungi and an antiviral agent for viruses to combat the pathogens. If it is a herpes virus, it may also be necessary to take additional tablets.
Home remedies for corneal inflammation
Since this is a very serious and potentially dangerous disease of the eye, treatment with home remedies should in principle only be carried out in conjunction with medical therapy and should be discussed beforehand with the treating doctor.
To combat burning and itching of the eyes, numerous aids can be used that have a cooling effect. Whether quark compresses, cold packs or cold compresses and compresses with water. If you have the feeling that warmth will help you, you can try that with the help of poultices.
Eye showers can also be used to flush out pus or to clean a blocked tear duct. In principle, the rooms in which you are located should also be darkened or sunglasses should be worn to protect your eyes. Computer, television screens, etc. should be avoided as far as possible and reading can already be too stressful on the eyes and should be avoided.
homeopathy
Homeopathic remedies are a way to complement therapy, but should never be the sole main therapy. Since in the worst case scenario blindness can occur, it is very important to visit an ophthalmologist. After consulting the attending ophthalmologist, homeopathic remedies can still be used.
If you like, you can use eye drops or tea infusions. Eyebright (Euphrasia) is particularly popular for this. But other plants such as marigold (calendula) or celandine are also used here. Chamomile is sometimes also recommended, but it also has potentially irritating properties on the eye and should only be used on the eyelid if possible. All of these medicinal plants can be easily infused as tea, so that the tea bag can be placed on the eyelid for use. The teas can be easily applied to the eye with a compress.
Duration of a sick leave
A sick leave can be a useful way to speed up healing. As a rule, it is recommended that you be on sick leave for about 2 weeks, as the eyes need this period of time for the inflammation to heal by the time you go back to work, school or daycare. However, this is more the case with viral corneal inflammations, as these can be very contagious. If corneal inflammation is caused by fungi, the risk of transmission is less high. A two-week sick leave is also possible here.
The different forms of corneal inflammation
Corneal inflammation caused by viruses
_3.jpg)
In most cases, that is the culprit Herpes Simplex Virus, the Varicella zoster virus (Otherwise it causes chickenpox and shingles) and the Adenoviruses.
If the inflammation flares up again after an earlier infection (with blistering on the lid), herpes keratitis develops, as the herpes viruses persist in nerve branches for life.
Herpes zoster keratitis occurs after a previous chickenpox disease and develops in the context of shingles of the face and eyes.
Adenovirus keratitis is a new infection and comes in combination with conjunctivitis (Conjunctivitis) in front.
In addition to a Redness of the eye, Pain and Foreign body sensation Characteristically branching occurs as a typical symptom when looking at the eye Defect in the cornea to days.
This can be made more clearly visible by applying the dye fluorescein.
In the case of herpes infection, the sensitivity of the cornea is also reduced, which can be tested with a cotton swab.
Herpes zoster keratitis is usually noticeable due to herpes zoster with blistering on the skin of the face, while there are rarely symptoms of the eye itself.
Nevertheless, the corneal inflammation can lead to further damage to and in the eye.
The Adenovirus keratitis (Epidemic Keratitis and Conjunctivitis) is shown by reddening, swelling and secretion of the conjunctiva. Punctiform defects on the surface of the cornea also lead to cloudiness for weeks to months and thus a deterioration in visual acuity.
Corneal infections caused by herpes simplex and varicella zoster can be treated with antiviral drugs (e.g. acyclovir) that are given as eye drops, tablets or infusions. The conjunctivitis and corneal inflammation caused by adenoviruses, however, cannot be treated with drugs, so that the focus here is on avoiding infections in people who come into contact with the sick person.
Corneal inflammation caused by fungi (mycotic keratitis)
Most corneal infections of this type are due to the yeast Candida albicans conditionally. The infection often occurs through injuries with fungal material, especially if there is an immunodeficiency.
Fungal keratitis often looks like bacterial corneal inflammation, but is often less discomforting.
Next to one Corneal ulcer usually small neighboring ulcers appear ("Satellites") and pus in the anterior chamber of the eye (Hypopyon).
The detection of the fungi takes place in the laboratory, but it is complicated.
The subsequent therapy takes place with Antifungal drugs (Antifungal agents) such as nystatin, natamycin or amphotericin B.
Corneal inflammation in dry eyes
A dry eye (Sicca syndrome) is caused by a poor composition of the tear fluid or a lack of tears in general.
In addition to chronic conjunctival irritation, microcracks in the corneal epithelium can then occur (Corneal surface) come.
Find out more about the topic: Watery eyes
Dry eyes are determined by various tests, the most important of which is the so-called Schirmer test.
With tear substitutes and nourishing ointments, one then treats eyes that are too dry or uses methods such as plugs (Punctum plugs) into the tear duct.
Read more on the topic: Dry eyes
Corneal inflammation with insufficient eyelid closure
If the eyelid is not closed completely, especially if the Facial nerve (Facial nerve, facial palsy), at Eyelid distortions (e.g. after surgery) protruding eyeball (Exophthalmos) or occurs in unconscious patients, the cornea dries out.
This causes damage to the surface of the cornea and, in some cases, an ulcer.
The therapy is carried out with tear substitute fluid, antibiotic and nourishing ointments and usually also with a so-called "watch glass bandage" that keeps the eye moist.
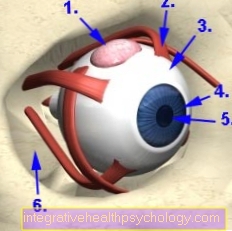
Corneal inflammation in contact lens damage
_4.jpg)
Wearing contact lenses for too long or contact lenses that are insufficiently adapted to the individual eye can damage the cornea and conjunctiva.
This then leads to micro defects up to ulcers and vessels can sprout into the cornea. As therapy, an alternative visual aid is provided via glasses and exposure to contact lenses for a longer period of time. In addition, the ophthalmologist can prescribe cortisone to reduce inflammation.
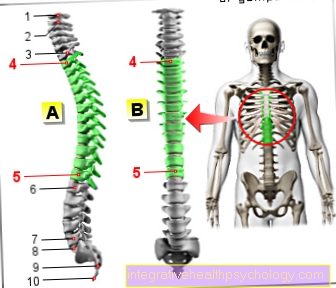
The cornea
As Cornea is the term used to describe the front, transparent skin of the eye. Through her Refraction carries them with a large part to the sharp image on the Retina at.
In addition, the cornea has a Protective function for the eye and supports the stability of the eye. Tear fluid and eyelid closure ensure that the corneal surface is wetted with fluid and thus preserve it Dehydrationwhich can lead to micro-cracks.
The cornea is divided into three layers:
- the outer, thin epithelium,
- the middle, thick stroma
- and the thin one Endothelium,
that represents the inner surface.
In general, all layers of the cornea can become inflamed and often several layers are actually affected. With inflammation of the Epithelial cell layer there is often cloudiness.
Is this Stroma affected, this cloudiness is usually whitish in color.
should that Endothelium be affected, it swells Cornea often disc-shaped. In most cases that is Conjunctiva Also reddened from the irritation from the inflammation, which is also noticeable as a symptom.



.jpg)