jaw
introduction
The upper jaw and lower jaw belong to the human jaw. While the lower jaw is a single bone, the upper jaw belongs to the bony facial skull.

Bony part
The jaw is formed from the lower jaw bone (Mandible) and the upper jawbone (Maxilla). The lower jaw bone (mandible) consists of a body (Corpus mandibulae) and a frame (Ramus mandibularis). The body is divided into a base and an alveolar part (pars alveolaris), in which the 18 teeth of the lower jaw lie. The frame (Ramus mandibularis) divides into 2 processes, the coronoid process and the condylar process, which is part of the temporomandibular joint (Art. Temporomandibulris) transforms.
The body and frame of the lower jaw together form the lower jaw angle (Angulus mandibularis). This changes in the course of life by 150 degrees in the newborn and then becomes less and less. In adulthood it is 120-130 degrees and in old age it rises again to around 140 degrees. This change is due to a change in the size of the body (corpus mandibulae) and is dependent on the number or shape and presence of the teeth.
The maxillary bone (Maxilla) is divided into bodies (Corpus maxillae), in the frontal process (Frontal process), into the yoke process (Zygomatic process), the palatal process (Palatine process) and the alveolar process (Alveolar process) which contains the 16 teeth of the upper jaw.
The temporomandibular joint
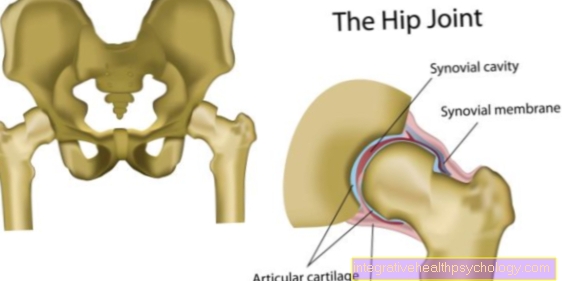
The temporomandibular joint (Articulatio temporomandibularis) is from the articular process (Condylar process) of the lower jaw bone (Mandible) on which the joint head (Head mandibularis) and the socket (Mandibular fossa) of the temporal bone (Temporal bone) located just in front of the external ear canal (Meatus acousticus externus) is formed. The joint head is cylindrical in shape and covered with articular cartilage on the front. Because of its shape, it is often referred to as a pine roller. Between these two joint partners there is a 3-4 mm thick, fibrous cartilaginous joint disc, concave on both sides (Articular disc), which is quite thin in the middle and increases in thickness towards the edges. It is on all sides with the outer layer of the joint capsule (Membrana fibrosa) grow together and divide the temporomandibular joint into two superimposed chambers. It serves as a movable socket, sits on the temporomandibular joint head (Head mandibularis) and shifts with this at the mouth opening. The joint capsule (Articular capsule) of the temporomandibular joint consists of two layers. The synovial membrane as the inner layer that lines all inner surfaces except the articular cartilage and the disc, and the synovial membrane as the outer layer, which is at the top of the anterior edge of the articular cusp (Articular tuberosity), inside and outside on the edges of the joint socket (Articular fossa), back in the area of the suture of the temporal bone and the occiput (Sutura tympanosquamosa) and below the upper part of the jaw neck (Collum mandibular) starts.
Three ligaments that lie outside the joint capsule strengthen the temporomandibular joint. The outer and inner band (Lateral and medial ligaments), which from the outside and inside along the joint capsule from the outside-inside of the zygomatic arch (Arcus zygomaticus) backwards obliquely to the jaw joint neck (Collum mandibulae) to run. The mandibular sphenoid ligament (Sphenomandibular ligament) runs from the sphenoid spine (Spina ossis sphenoidalis) to the inner surface of the lower jaw bone (Lingula mandibulae). The last of the three ligaments is the mandibular stylus ligament (Stylomandibular ligament), which from the stylus process (Styloid process) to the posterior edge of the lower jaw angle (Angulus mandibulae) running.
The temporomandibular joint is a special joint because both the right and left sides always work together. The two sides are connected via the lower jaw and always exert forces at the same time. The function of the temporomandibular joint is primarily to establish the connection between the lower jaw and the temporal bone of the skull. This enables the chewing movement. There are 3 main movements. When the lower jaw is pushed back and forth, both joints act congruently. This also applies to opening and closing the mouth. But if grinding movements are carried out, i.e. circular movements in all dimensions (right and left, forwards and backwards, up and down), the joints move asymmetrically. This is only possible thanks to the joint anatomy.
The joint consists of a joint socket, a joint head and the joint capsule. The mandibular fossa is the joint socket (pit into which the head protrudes). It is located on the skull bone. A small hump (tuberculum articulare) is in front of it. This prevents the joint head from jumping out of the pit too quickly and causing a lock in the jaw (mouth can no longer be closed). Between the joint head, which is located on the articular process of the lower jaw, and the joint socket, there is the discus articularis, a cartilage that makes it easier for the joint heads to slide in the socket. If this cartilage is worn down in old age, pain can also occur as with other joints. Together with three large ligaments, the joint capsule ensures the stability of the joints.
Read more on the topic: Temporomandibular joint

- Upper jaw -
Maxilla - Zygomatic bone -
Os zygomaticum - Nasal bone -
Nasal bone - Tearbone -
Lacrimal bone - Frontal bone -
Frontal bone - Lower jaw -
Mandible - Eye socket -
Orbit - Nasal cavity -
Cavitas nasi - Upper jaw, alveolar process -
Alveolar process - Maxillary artery -
Maxillary artery - Under eye cavity hole -
Infraorbital foramen - Ploughshare - Vomer
You can find an overview of all Dr-Gumpert images at: medical illustrations

- Lower jaw - Mandible
- Crown process -
Coronoid process - Lower jaw rest -
Ramus mandibulae - Mandible angle -
Angulus mandibulae - Upper jaw - Maxilla
- Zygomatic bone - Os zygomaticum
- Zygomatic arch -
Arcus zygomaticus - Temporomandibular joint -
Articulatio temporomandibularis - External ear canal -
Meatus acousticus externus - Temporal bone - Temporal bone
- Frontal bone - Frontal bone
- Chin hole - Mental foramen
- Eye socket - Orbit
- Upper jaw, alveolar process -
Alveolar process
You can find an overview of all Dr-Gumpert images at: medical illustrations
Muscles of the jaw
The masseter muscle (M. masseter) is divided into two parts. One part runs more superficially, diagonally back and down (Pars superficialis), one part runs deeper and perpendicular (Pars profundus), both parts arise at the zygomatic arch (Arcus zygomaticus) and start on the outer surface of the lower jaw frame (Ramus mandibulae). The temporal muscle (Temporalis muscle) arises as a flat muscle arched below the temporal line (Temporal line). It is bundled and runs below the zygomatic arch (Arcus zygomaticus) to attach to the coronoid process of the lower jaw (mandible).
The inner wing muscle has its origin in the wing pit (Pterygoid fossa) and pulls to the inside of the jaw angle (Angulus mandibulae).
The external wing muscle arises with a small upper part (Pars superior) on the lower edge of the sleeping area (Crista infratemporalis) of the sphenoid (Sphenoid bone). The lower part (Pars inferior) arises on the outer surface of the Pterygoid process. The upper part (Pars superior) starts at the articular disc, the lower part (Pars inferior) on the condylar process of the lower jaw (Mandible).
Also read: Jaw muscles
Movements of the jaw
in the jaw to run Chewing and grinding movements that come about when the movements of both sides of the jaw are coordinated. It comes to Reduce (Abduction), to the To lift (Adduction), to the Advance (Protrusion), to the Push back (Retrusion) and to grinding movements or to Move sideways (Laterotrusion). Only one jaw joint is actively involved in the grinding movement. The balance side is chewed, this is where he sits vibrating condyle (Translational condyle), on the working page of the dormant condyle (Rotational condyle) is not chewed.
The Reduce lead the front part of the dibular muscle (Digastricus venter anterior muscle), of the Chin-hyoid bone muscle (Geniohyoid muscle), of the Mandibular hyoid bone muscle (Mylohyoid muscle) and the outer wing muscle (Lateral pterygoid muscle) out.
The lifting is from that Temporal muscle (Temporalis muscle), the Masseter muscle (Masseter muscle), the outer wing muscle (Lateral pterygoid muscle) and the inner wing muscle (Medial pterygoid muscle) executed.
The Advance is executed by the outer wing muscle (Lateral pterygoid muscle) and from Masseter muscle (Masseter muscle).,the Push back from Chin-hyoid bone muscle (Geniohyoid muscle) and from the back of the dibular muscle (Digastricus venter posterior muscle).
Lock jaw
In contrast to the jaw clamp, in which the mouth opening is obstructed, with the jaw lock it is not possible to completely close the jaw. The teeth cannot completely bite each other again. The causes can be osteoarthritis or acute arthritis, i.e. problems with the temporomandibular joint. The most common reason is jaw dislocation. That means a dislocation of the lower jaw. Since at least one joint head slipped forward during the dislocation, it is physiologically impossible to close the mouth completely. In some patients this happens more often, almost "usually". Then one speaks of a habitual (familiar) jaw dislocation.
Read more on the topic: Lock jaw
The dentist can use the Hippocrates handle to adjust the jaw again. It looks like this: the dentist stands behind the patient, grasps the lower jaw with both hands, right and left. The thumbs are placed on the bottom of the row of teeth or the bone. The lower jaw is pulled forward and down. This allows the joint heads to slide back into their joint pit through the ligaments and muscles. A joint centric splint can be made as a therapy. It holds the lower jaw in this position, in which the joint is exactly in the middle. This allows the joint capsule to recover and any inflammation can heal.
Innervation
The above Muscles and the Temporomandibular joint are all from Mandibular nerve (Mandibular nerve), which is the third branch of the Trigeminal nerve is.
Vessels
The Maxillary artery runs behind the Ramus mandibularis and supplies the Lower jaw (Mandible), the upper jaw (Maxilla), and the Masticatory muscles with arterial blood. Most of the venous blood flows through the Pterygoid plexusthat is below the Ramus mandibularis lies in the Maxillary vein. The maxillary vein goes into the Retromandibular vein about which is in the Internal jugular vein pours.
Jaw pain
Pain in the jaw can have several causes. Mostly the temporomandibular joint is the trigger, but often also the muscles or radiating pain from the tooth area or the maxillary sinuses. The causes of jaw pain caused by the jaw muscles include in particular tension, but also overstretching or injuries. If pain in the jaw is triggered by the temporomandibular joint, the cause is usually trauma, injury, overstretching or incorrect loading (e.g. due to poorly fitting dentures, orthodontic misalignment of the teeth or a gaping bite with unphysiological stress).
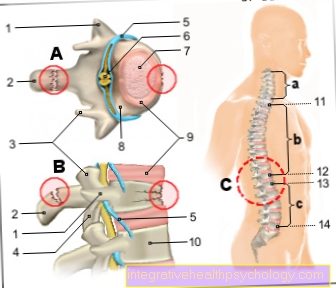
In some cases, an inflammation in the temporomandibular joint or osteoarthritis can be the cause. Often jaw pain also occurs when the wisdom teeth break through and possibly cannot find a place, but infections in the ear, nose and throat area can also project onto the jaw. Back pain (especially in the neck area), misaligned hips and the resulting tilted position of the head or incorrect loading are also associated with pain in the jaw. These symptoms should be clarified by the appropriate specialist. The most common cause of pain in the jaw (joint and muscles), however, are clenching or grinding of teeth (bruxism). If the symptoms are due to bruxism, most patients describe the increased occurrence of symptoms when they wake up in the morning. The reason for this is the nightly stress reduction through pressing and crunching. Often this leads to an enormous volume and lack of sleep on the part of the partner, who usually notices the problem before the patient himself.
Doctors use the term "CMD" (craniomandibular dysfunction) for this. Various questionnaires, analyzes and x-rays are used to make a diagnosis. Often several symptoms occur together: Bruxism is associated with tinnitus and severe headaches. Mostly, gnash splints / bite splints are used therapeutically. An alternative is "myofunctional therapy", a special functional therapy by the physiotherapist that also relieves muscular tension. Drug therapies (such as muscle relaxants) should only be used in short-term therapy.
Autogenic training and self-massage, orthodontic or prosthetic therapy for misaligned teeth and loss of tooth substance can also be indicated. With a prosthetic realignment of the bite situation, the adaptation of the surrounding structures to the new situation must always be considered and tested. Various measurements, including joint path measurements with special electrical sensors, may be necessary. Jaw pain rarely occurs even after long-term dental treatment. Here, the chewing apparatus is overstretched due to the long stay, which, however, regulates itself again after a certain waiting time.
Read more on this topic at: Jaw pain
Cracking jaw
A Cracking jaw (more precisely the temporomandibular joint) can be classified as unproblematic in most cases and does not require any therapy. Often a crack is not associated with pain. It is important that in this case other influencing factors such as muscular tension, one Gap bite, Misaligned teeth or headaches can be excluded. The situation is different if the cracking noise is accompanied by discomfort, including restrictions on eating or moving. This should always be clarified and treated immediately. Information about the duration / frequency and occurrence (type, time) of the noises and complaints, which in most cases a CMD (Craniomandibular dysfunction) can be attributed. A cracking (mostly lower jaw) after jaw operation (caused by trauma or wisdom tooth operation) must also be clarified.
In this case, the bone can remain very thin and fracture under excessive stress after the operation. Hard food should therefore initially be avoided after such an operation.

















.jpg)