Inguinal fungus
definition
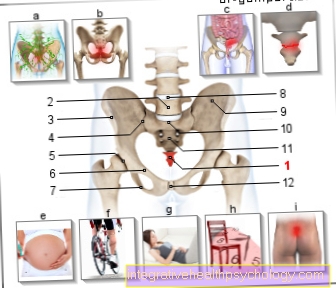
The inguinal region extends from the mostly easily palpable front upper protrusion of the iliac blades to the genital area. An infection, i.e. strong reproduction and colonization, by fungi can occur here. A so-called Mycosis the skin can also be described as inguinal fungus. Depending on the type of pathogen, such a fungal infection of the groin is also called "Tinea inguinalis" or "Intertriginous candidiasis" designated. Often the skin changes spread to adjacent areas over time.In the following, the buttocks or genital region can also be affected.

causes
There are various fungi that can affect the human body. As a rule, these fungi are actually a normal part of our skin flora. The fact that they multiply, spread and cause symptoms mostly depends on various risk factors. Although fungi are part of the body, they should still be prevented from spreading beyond the skin barrier. Therefore, our immune system is constantly fighting their growth. If a person's immune system is weak (for example in the context of an existing underlying disease), this favors the fungi to multiply.
Read more on this topic at: The fungal infection of the skin
In addition, the best growing conditions for mushrooms are found in a humid and warm climate. Frequent and profuse sweating therefore creates a favorable environment for fungal growth. There may also be a genetic predisposition for an increased risk of developing a fungal infection.
You might also be interested in: Excessive Sweating - What Causes It? and how can you strengthen the immune system?
Concomitant symptoms
A fungal infection is mainly noticeable through the changes in the skin on the affected area. Inflammation develops. This spreads out from a center in all directions. Since it heals quickly in the center, the flocks infected by the fungus look like red rings. The inflammatory reddening is often accompanied by itching. In addition, scaling with emphasis on the edge can often be seen. The skin between the skin folds, which are usually kept moist by sweat, also tends to swell or soften. This encourages the fungi to penetrate deeper skin layers. If deeper layers of the skin are infected, an additional bacterial infection can also lead to the formation of a painful abscess.
Read more on this topic at: Inflammation in the groin
itching
Itching is a typical symptom of a fungal infection. Often the itching is the first sign when there is no reddening or flaking of the skin. It is important to be careful not to scratch if possible. If you scratch the skin, it will be further injured and the fungi can penetrate deeper layers of the skin. The healing is not only delayed, but the clinical picture can get even worse.
You might also be interested in: Itchy skin and itchy rash - what disease is it?
Redness
The reddening of the skin usually indicates inflammation. The inflammation is the visible and tangible sign that the body is fighting against pathogens. An infection with fungi also causes inflammation, which includes reddening of the skin. The typical thing here is that the redness spreads outwards from a center. Since the pathogens have already been successfully combated in the first infected center, healing takes place here. What remains is the circular outer area where the inflammation still persists. Skin areas infected by the fungus therefore often look like red rings. In the case of a large-scale, massive infestation, the outward spread is noticeable, with the outermost edge being reddened and central areas already beginning to pale.
Pain
Initially, pain is not a typical symptom of a fungal infection. The itching is more in the foreground here. However, if deeper layers of the skin are attacked, the penetration of other pathogens is favored. If, for example, bacteria get deep into the skin and lead to an additional bacterial infection, this can lead to suppuration and severe pain.
Swelling of lymph nodes in the groin
A fungal infection in the groin can lead to swelling of the inguinal lymph nodes. The swelling is a sign that the immune system has been activated. The cells of the immune system are first transported along the lymph vessels to the site of the infection. Then other cells of the immune system are activated in the lymph nodes. These reactions lead to swelling of the lymph nodes and pain. The groin lymph nodes also swell in all other infections or injuries to the lower extremities (from the feet to the groin). A lymph node swelling alone does not speak for a fungal infection without the typical skin symptoms.
You might also be interested in: Lymph node swelling in the groin
Oozing skin
The sore skin in the area of a fungal infection can also ooze. This is because the inflammation, which the body uses to defend itself against the fungal infection, causes the vessels to widen. This allows immune cells to reach the site of inflammation more quickly. However, liquid can also escape from the vessels more easily. Then the wound "wets".
Treatment / therapy
Fungal infections (Mycoses) the skin are usually locally made with so-called Antifungal drugs (= "Antifungal agent") treated. The creams and solutions available contain active ingredients that either counteract Dermatophytes or Yeasts are effective. Tolnaftate, for example, acts against dermatophytes alone. Ointments containing nystatin help with candidiasis. Amphotericin B can also be used here in severe cases. In order to act against dermatophytes, yeasts and some bacteria at the same time, broad-spectrum antifungal agents are now also available (e.g. clotrimazole, terbinafine or ketoconazole). Systemic antifungal therapy may also be necessary if the fungal infection is severe and persistent. This means that medication must be taken by mouth or given through the vein. This therapy is always combined with the local therapy. This keeps the side effects of systemic therapy as low as possible. Itraconazole or fluconazole are suitable active ingredients for systemic therapy.
You might also be interested in: Antifungal and fungal medication
How contagious is a groin fungus?
Inguinal fungus is caused by fungi that are normally permanent on our human skin. The development of a fungal infection of the skin is related to the fact that our immune system is weakened by other diseases, drugs or the like. Anyone who has a fungal infection should therefore stay away from people who are in such a weakened condition. There is no great risk of infection for any other healthy person.
Which ointments and creams help with inguinal fungus?
In the case of the drugs against inguinal fungus, care should be taken that they have a so-called antifungal Contain active ingredient. This means that the appropriate solutions or creams are effective against fungi. Since not every active ingredient against all types of fungi (for the inguinal fungus come mainly Yeasts and Dermatophytes in question) is effective, pathogen diagnostics should take place beforehand if possible. It therefore depends on the active ingredient that the creams contain. As soon as you know the active ingredient, pharmacists can help very well. For example, tolnaftate is effective against dermatophytes and is contained in creams such as "Tinatox". Nystatin is another active ingredient and the cream of the same name can be used in the event of a yeast infection.
Canesten®
Canesten® is one of the local antimycotics. It contains the active ingredient Bifonazole. Bifonazole is what is known as a broad-spectrum antifungal, which means that it is effective against almost all known fungi. Infections with dermatophytes, yeast, and mold are covered. Canesten® is only suitable for local use.
Read more on this topic at: Canesten®
Lamisil®
Lamisil® contains the antifungal agent Terbinafine. It works by disrupting the structure of the vital cell membrane of fungi. Lamisil® is available in tablet form for oral intake (= intake through the mouth). The active ingredient is also available as a cream and can be applied directly to the affected area of the skin. Local application is preferred for fungal skin infections. It should be noted that the active ingredient terbinafine can only be used reliably against infection with dermatophytes. The cause of the inguinal fungus should also be a yeast infection, such as Candida albicans another preparation should be used. Unfortunately, the drug is considered poorly tolerated.
Home remedies for a inguinal fungus
In the case of fungal infections, it should be noted that fungi are particularly comfortable in a warm and humid environment. Here you will find the best growing conditions. It is therefore helpful to withdraw this milieu from you. After showering and if you sweat heavily, care should be taken to dry the skin thoroughly. The application of baby powder or baking soda can also be used in this sense. Aloe Vera also has a positive effect on skin fungus. The itching can be relieved and the skin is cared for at the same time. Other remedies that are used are, for example, apple cider vinegar, garlic or lavender oil.
Which fungi are the most common cause of inguinal fungus?
Various fungi can attack the human body. A distinction is made here between three types. These include the thread fungi (Dermatophytes)who have favourited Sprouts (Yeasts) and mold. Typical pathogens of inguinal fungus are dermatophytes. The most common infections are thereby through the Unterform "Trichophyton rubrum" triggered. Are parts of the body such as the groin that are located between two skin folds (so-called Intertrigines), one speaks of "Tinea intertriginosa" or in the special case of the bar of "Tinea Inguinalis". The skin can be attacked by yeasts, especially when the body has a weak immune system. Affects the most common form "Candida albicans" the groin region is called this "Candida inguinalis" designated.
You might also be interested in: Fungal diseases
Duration of an inguinal fungal infection
How long an inguinal yeast infection lasts initially depends on the extent of the infection. There are also acute and chronic forms in the case of fungal attack on the skin. An infection can last for a few days, but also for years. Basically, the skin has to be treated until the infection subsides. If an initially local therapy with creams and solutions does not work, a combination with systemic therapy can be started after one to two weeks. Deep-seated and extensive findings are treated directly with a two-week systemic therapy.
diagnosis
Other diagnostic means are used if one suspects a fungal infection due to visible changes in the skin. With the help of a swab or the scraping off of small flakes of skin, these can be examined under the microscope. If this is not enough, it may be necessary to take a sample from deeper skin layers with the help of a biopsy. This is how the diagnosis is secured. It is also possible to create a mushroom culture from the material obtained. This means that the mushrooms are grown on a nutrient medium so that the exact pathogen can be identified. Another method is the application of so-called "Wood light", whereby the infected regions appear in a different color depending on the pathogen.