Gastric ulcer
Synonyms in a broader sense
Medical: ulcer
Gastroduodenal ulcer disease, gastric ulcer, duodenal ulcer, peptic ulcer, duodenal ulcer, ulcer disease, gastric mucosal inflammation
Definition of gastric ulcer
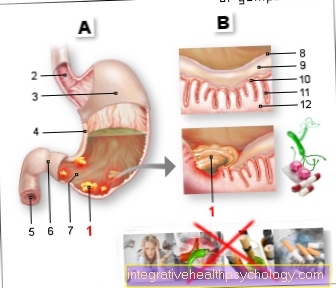
An ulcer is a benign gastric ulcer orDuodenal ulcer, which penetrates very deeply into the mucous membrane, at least into the inner muscle layer of the mucous membrane (Lamina muscularis mucosae; see also stomach), reaches into it. A dangerous complication of ulcer disease occurs when the ulcer reaches a larger vessel, causing life-threatening bleeding.
The predilection site for gastric ulcer is the small stomach curvature (Curvatura minor) in the area of the stomach cavity (antrums) near the gastric outlet. The two main causes of gastric ulcer are pain medication such as aspirin and NSAIDs and the bacterium Helicobacter pylori.

Defect of the gastric mucosa
- Gastric ulcer -
Gastric ulcer - Esophagus - Esophagus
- Stomach body -
Corpus gastricum - Small curvature of the stomach -
Curvatura minor - Duodenum -
Duodenum - Stomach porter - Pylorus
- Porter's Cave -
Antrum pyloricum - Slime coating the
Stomach surface - Surface fabric
of the stomach - Mouth of the
Gastric gland - Gastric gland
- Mucosal muscle layer
You can find an overview of all Dr-Gumpert images at: medical illustrations

Frequency (epidemiology)
Occurrence in the population
About 10% of the population has had a stomach ulcer or duodenal ulcer at least once in their life. The duodenal ulcer (ulcus duodeni) is about five times more common than the gastric ulcer (ulcus ventriculi).
Men are three times more likely to have a duodenal ulcer than women.
In the gastric ulcer, the sex distribution is 1: 1.
The peak of the onset age is between 50 and 70 years of age.

Anatomy stomach
- Esophagus (gullet)
- Cardia
- Body
- small curvature
- Fundus
- great curvature
- Duodenum (duodenum)
- Pylorus
- Antrum
Ulcer shapes / classification
A distinction is first made between an acute (sudden) and a chronically recurring (recurrent) gastric ulcer (ulcer). The acute "stress ulcer" occurs as a result of superficially damaging (erosive) Inflammation of the lining of the stomach (gastritis) on. The cause of this ulcer development are strong physical stress factors that lead to the sudden breakdown of the protective mucous membrane barrier. Such stressful situations are for example Burns, major operations and many other diseases requiring intensive medical care.
The chronic recurrent ulcers occur more frequently and can have various causes (see below).
Furthermore, the ulcers are divided according to their localization in Stomach ulcers and Duodenal ulcers. The gastric ulcer is most often found in the area of the small curvature of the stomach (curvatura minor).
The duodenal ulcer is almost exclusively at the beginning of the Duodenum (Duodenum) the duodenal bulb.
If ulcers are found in intestinal sections further away than described (e.g. jejunum section of the Small intestine), this can be an indication of a rare one Zollinger-Ellison Syndrome be.
Causes of the gastric ulcer
For the development of a gastrointestinal ulcer, the balance between the aggressive and defensive factors that protect the mucous membrane plays an important role (see figure). If the aggressive factors predominate or the defensive factors fail, an ulcer can result. A distinction is made between the causes, those that come from the body itself (endogenous cause) and those that are caused externally (exogenous cause).
1. Endogenous causes
Endogenous causes, i.e. causes that are caused by the body itself, are:
- Stomach acid
- Gastrointestinal mobility (peristalsis)
- Zollinger-Ellison Syndrome
- Hyperparathyroidism
- Rare causes
a) stomach acid
A very important factor in the development of an ulcer is stomach acid. This finding can be derived from the fact that patients with an autoimmune Inflammation of the stomach lining (Gastritis), which can no longer produce stomach acid, no ulcers. It should be noted, however, that gastric acid production is rarely increased in a gastric ulcer. In gastric ulcers, stomach acid is not the triggering factor but an accompanying factor (permissive factor) for the Entertainment / persistence of the gastric ulcer.
In the case of a duodenal ulcer, however, the excessive release (secretion) of gastric juice plays an essential role. Particularly noteworthy is the still largely unexplained increased formation of gastric acid and pepsin (aggressive protein enzyme in the digestive chain) during the night.
It is also assumed that the gastric acid is insufficiently bound by the basic bicarbonate, which is formed in the duodenum, as a partial cause of the development of the duodenal ulcer (insufficient acid neutralization).
b) gastrointestinal mobility (peristalsis)
An impaired coordination of the movement between the stomach cavity (antrum) and the duodenum is discussed more and more frequently. In some patients with peptic ulcer is next to one longer gastric passage A reverse flow of bile acid (gall reflux) into the stomach can also be observed for food. Bile acids are among the most aggressive factors on the mucous membrane.
c) Zöllinger-Ellison syndrome
Behind this name hides a rare tumor, the most common in the Brook salivary gland (pancreas) is localized and the hormone Gastrin produced.
Of the benign tumor is also known as Gastrinoma designated. The excess gastrin produced by the tumor leads to overstimulation of the acid-producing stomach cells (parietal cells). So too much stomach acid is produced. This excess of gastric acid leads to the predominance of aggressive factors in the gastrointestinal area and to the formation of many (multiple) gastric ulcers that occur at the same time.
Zöllinger-Ellison syndrome often leads to multiple ulcers in the duodenum and even further down the bowel (jejunum). These ulcers (ulcers) prove to be particularly stubborn. Treatment is long and difficult.
This syndrome causes only 1% of all gastro-duodenal ulcer diseases.
d) hyperparathyroidism
The hyperparathyroidism describes an overfunction of the Parathyroid (Parathyroidea). An excess of the hormone-producing cells (epithelial bodies) of the parathyroid gland is produced calcium (Hypercalcemia) in the body.
This in turn leads to the stimulation of the G cells in the stomach and duodenum, which produce the hormone gastrin described above. This in turn leads to overstimulation of acid-forming stomach cells.
e) Rare causes
Very rare causes are viral infections, e.g. with cytomegalyCytomegaly Virus (CMV) or the Herpes Simplex Virus (HSV) and chronic bowel disease, like the one Crohn's disease.
You can find further information under our topic:
- Crohn's disease and
- Herpes simplex
Sometimes an ulcer in the gastrointestinal area also arises as a result of one therapeutic x-ray exposure (Tumor therapy) or due to a Vascular disease.
2. Exogenous causes
Exogenous causes of a gastric ulcer are causes that come from outside the stomach. The following are particularly suitable for this:
- Helicobacter pylori (H.p.)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
a) Helicobacter pylori
The bacterium Helicobacter pylori (H.p.) has proven to be one of the most important causes of gastroduodenal ulcer disease (chronic ulcer) since its discovery in the early 1990s.
The risk of developing a gastrointestinal ulcer increases in the presence of a Helicobacter-related inflammation of the gastric mucous membrane (gastritis) by 3-4 times.
This does not mean that every person whose gastric mucous membrane is colonized with the bacterium will inevitably develop gastric mucosal inflammation or an ulcer. The Helicobacter bacterium can be detected in almost all patients with a duodenal ulcer. Approx. 75% of patients with gastric ulcer are infected with the Helicobacter bacterium.
Helicobacter pylori is also a permissive factor in the development of ulcers, which means that infection with the bacterium is not the sole cause of gastrointestinal ulcer development. Other aggressive factors (see above) must also be present.
b) Non-steroidal anti-inflammatory drugs
NSAIDs be like Acetylsalicylic acid (ASA) also, often used as a pain reliever for joint diseases and other painful conditions.
These drugs have a gastric mucus-destroying effect. The mechanism behind it is related to the inhibition of the so-called prostaglandin formation.
Prostaglandins have a vasodilating effect on the gastric mucosa and also promote the formation of protective gastric mucus. By reducing the formation of new prostaglandins, the gastric mucosa loses important protective factors. The risk of developing a stomach ulcer increases. The risk of developing an ulcer multiplies with NSAID medication and simultaneous Helicobacter pylori infestation.
You can find further information under our topics:
- NSAIDs
- Acetylsalicylic acid
Symptoms / complaints

The symptoms of peptic ulcer disease are often very non-specific. This is shown by statistics that state that 20% of ulcer patients are completely symptom-free (unsymptomatic) and in turn 20% of patients with symptoms such as ulcer disease did not show an ulcer in the gastroscopy (endoscopy).
Typically, NSAID-related ulcers are those that cause no or only very uncharacteristic symptoms.
The symptoms include:
- Upper abdominal discomfort
- nausea
- Bloating
- Food intolerance.
Pain can also occur, which often radiates to the chest (thorax), back or lower abdomen. This pain is often described as "hungry" and "gnawing".
In some patients, a certain rhythmic rhythm in the pain symptoms can be determined, which occasionally suggests the location of the ulcer / ulcer.
Nocturnal pain and post-meal pain relief appear to be typical of duodenal ulcer (ulcus duodeni). Worsening after eating is more likely to occur in a gastric ulcer (gastric ulcer).
However, the diagnosis can only really be confirmed by a gastrointestinal examination.
Complications
If a gastric or duodenal ulcer breaks through the stomach or intestinal wall and the gastric juice is connected to the free abdominal cavity (peritoneal cavity), it is called an ulcer perforation (gastric perforation).
Such an ulcer perforation occurs in the course of the disease in 10% of patients with a duodenal ulcer and in 2-5% with a gastric ulcer. Breakthroughs are more common in NSAID-related ulcers because they are recognized and treated later due to the painless process. The breakthrough (perforation) of the stomach or intestinal wall can lead to life-threatening inflammation of the peritoneum (peritonitis), which must be surgically treated as quickly as possible.
In some cases, an ulcer can also “break into” an adjacent organ, which is known as ulcer penetration (“covered perforation”). Because of the close proximity to each other, the pancreas can be affected if a duodenal ulcer crosses the outer wall of the intestine.
A stomach ulcer can also seldom break into the liver (hepar).
When an ulcer hits a blood vessel and damages it, it may cause ulcer bleeding / ulcer bleeding. This complication still has a mortality rate (mortality rate) of 10%.
Bleeding can appear as hidden (occult) blood in the stool, as tarry stool (Mälena) or even as vomiting of blood (hematemesis). Therapy consists in injecting medication such as adrenaline under the ulcer during a gastrointestinal examination, which stops the bleeding because adrenaline constricts the bleeding vessel.
Even if the bleeding stops bleeding on its own, nowadays the ulcer is injected under in order to prevent repeated (recurrent) bleeding.
Only if hemostasis cannot be achieved in any way using endoscopy does the bleeding have to be stopped during an open operation. This complication occurs more often in gastric ulcers that are located on the posterior wall of the stomach, since the anatomical proximity to a gastric artery (artery) there tends to lead to particularly heavy bleeding.
Read more about: Blood in the stool - what are the causes?
Complication of gastric bleeding
Caution: The complication of gastric bleeding is still associated with a mortality rate (mortality rate) of 10%.
For more information on this topic, see: Gastric Bleeding

Illustration gastric ulcer
The gastric ulcer can be seen localized at a typical location at the gastric outlet.
In the picture below, the stomach wall is shown in cross section and you can see how deep the stomach ulcer extends.

Layers of the stomach lining
- Mucosa (mucous membrane)
- Gastric ulcer
- Submucosa (layer of connective tissue)
- Blood vessels
If the mucous membrane is damaged, it can reach into the connective tissue below, which can lead to gastric bleeding.
A less common complication of a gastric ulcer is the Constriction of the stomach or duodenum (Stenosis) These occur mostly in the area of the gastric outlet (pylorus) and the beginning of the small intestine (duodenal bulb), when repeated (recurrent) ulcers and thus scarring and tissue shrinkage occur in this area. The typical initial symptom of this complication is repeated vomiting, as the food ingested can no longer pass through the stomach or intestines in the area of the constriction.
Stress as a cause of a stomach ulcer?
Generally, a stomach ulcer is caused by an imbalance between the stomach protective factors and the attacking substances. Stress alone however can Not lead to the formation of a stomach ulcer. However, it is possible that there is a lot of constant stress in combination With unhealthy diet, alcohol and Smoke to a Inflammation of the stomach lining leads and thus a Gastric ulcer can trigger.
The reason for this is that these factors have increased Acid production lead in the stomach. This attacks the Gastric mucosa on and can to Inflammation the mucous membrane. In addition, the Sympathetic of the nervous system activated. This sets the body on flight and fight and stops the bowel activities. So on the one hand Stomach pain from stress, Constipation or diarrhea arise, but also increased acid production.
The medically titled Stress ulcer (Gastric ulcer triggered by stress) does not refer to everyday stress as the cause, but rather to previous ones major operations, massive Burns, Multiple trauma, sepsis or a shock. There is a decreased blood flow in the stomach and an increased production of gastric acid. Both lead to inflammation of the mucous membranes and can trigger a stomach ulcer. Since this complication is known and occurs in the context of life-threatening diseases, the stress ulcer can be prevented with medication. So can Proton pump inhibitors or other medicinal acid blockers are used. These prevent increased acid production and thus the development of a stress ulcer.
Diagnosis of gastric ulcer
Diagnosing one Gastric ulcer is created by various diagnostic instruments:
- Patient talk
- X-ray swallow
- Gastroscopy
- Urease test
- 13C urea breath test
1. Discussion with the patient
This gives the first clues as to the underlying gastric ulcer disease Patient talk (anamnese) after typical complaints, taking medication (NSAID?, Aspirin? Etc) is asked. The physical examination may reveal a tender upper abdomen. In the laboratory, low hemoglobin can indicate a Anemia (anemia) and thus on an ulcer bleeding / Gastric bleeding indicate.
In the stool examination can be invisible "Occult" blood getting discovered (Hemocult test).
False positive results of the haemocult test due to certain medication intake (e.g. iron supplements) or food are possible. The definitive diagnosis of gastric ulcer, however, is not made until the stomach Colonoscopy posed.
2. X-ray swallow
At this Peptic ulcer diagnosis the stomach area is x-rayed while the patient is inside X-ray contrast media swallows. The contrast medium fills the stomach, so that the surface texture (the relief) of the Gastric mucosa can judge.This examination is mainly carried out in patients who refuse to have a gastric mirror or who cannot be examined. The ulcers typically appear as niches in the relief of the stomach wall, in which contrast media collects.
However, this examination method is not the method of choice for the diagnosis of gastric ulcer because not all ulcers / gastric ulcers are detected and, moreover, ulcers / gastric ulcers are not detected Stomach cancer (Gastric cancer) can be distinguished.
The examination is particularly valuable if one is suspected Gastric outlet obstruction. You can typically see a narrowing on the X-ray images that looks like an hourglass silhouette. Therefore, this narrowing is also "Hourglass stomach" called.
3. Gastroscopy (gastroscopy)
The "Reflection" (Endoscopy) from stomach and duodenum is the method of choice for a "diagnosis of gastric ulcer" for the direct assessment and classification of mucosal damage and should be carried out if a stomach or duodenal ulcer is suspected. During this examination, images are transmitted to a monitor via a tube camera (endoscope).
During the endoscopy you can also Tissue samples (biopsy) can be taken from suspicious areas of the mucous membrane. At least six tissue samples should be taken from an ulcer by one tumor (Carcinoma) of the stomach, which sometimes cannot be distinguished from an ulcer during the mirroring, cannot be overlooked.
The tissue assessment under the microscope (histological findings) is far more meaningful than the (macroscopic) findings recorded with the naked eye. You can also use a piece of fabric to cover the Urease Test perform. The urease test is used to detect the bacterium Helicobacter pylori.
4. Urease test
In this gastric ulcer diagnosis, the removed piece of tissue is placed in a special medium for 3 hours. Only Helicobacter pylori can in this medium ammonia from the bacteria own enzyme Urease form and the medium changes color. In this way, you can quickly and cheaply detect Helicobacter pylori infection in the gastric mucosa.
5. 13C-urea breath test
This test can also detect the bacterium Helicobacter pylori prove. The patient becomes a 13C labeled urea (radioactively labeled) administered orally via a drink.
The patient must then exhale vigorously through a straw into a special glass tube. Because the bacterium breaks down this urea into CO2 and ammonia, the proportion of labeled 13C in the exhaled CO2 can be measured. With this not exactly cheap process, the Success of antibiotic therapy against Helicobacter pylori (eradication therapy) must be checked. The advantage of this examination is that it is non-invasive, which means that it does not intervene in the patient's body and is therefore almost free of complications.
Further diagnosis of the gastric ulcer
In the case of treatment-resistant ulcers (ulcers), additional diagnostics should always be initiated to prevent gastric cancer (Stomach cancer) or less common ulcer diseases can be safely excluded. If you are unsure about gastric cancer (gastric cancer), a second gastroscopy with renewed tissue removal and examination can provide additional security.
To exclude rare ulcer causes, the Gastrin levels measured in the blood by one Zöllinger-Ellisson syndrome shoot out or that calcium examined in blood to a Hyperparatyroidism (Malfunction of the Parathyroid) to uncover.
Causes of resistance to treatment can also rare Helicobacter strains for whom the usual antibiotic therapy does not work or an inflammatory bowel disease such as the Crohn's disease or one Herpes Simplex Virus infection.
You can find further information under our topic: Crohn's disease