MRI for a herniated disc
introduction
A herniated disc is a disease that is characterized by the protrusion of parts of the disc into the spinal canal.
A real herniated disc must be caused by a so-called protruding disc (Disc protrusion) are delimited.
In most cases, the development of a herniated disc can be associated with long-term excessive or incorrect loading.
While the development of a herniated disc is rarely observed in younger years, this disease becomes more common with increasing age, due to the fact that the elasticity of the intervertebral disc decreases sharply with aging.

This is how I recognize a herniated disc
People who suffer from a herniated disc usually develop severe back pain that can spread from the affected spinal column to the arms, buttocks or legs.
In this context, however, it must be noted that the herniated disc is a comparatively rare cause of back pain.
In most cases, persistent back pain can be attributed to muscular stress.
Read more on this topic at: Causes of a herniated disc
In addition, sensation disorders such as numbness and / or tingling may indicate a herniated disc. These sensory disturbances typically occur in areas of the skin that can be assigned to a spinal column segment (so-called Dermatomes).
Read here whether your tingling sensation or numbness is an indication of a herniated disc:
- Numbness indicating a herniated disc
and - Tingling sensation indicating a herniated disc
In the case of an advanced herniated disc with a strong influence on a nerve root, the affected patients also often notice limitations in muscle strength.
Depending on the affected spinal column segment, the decrease in muscle strength can be demonstrated in certain key muscles.
People who suffer from severe back pain, sensory disturbances or limitations in muscle strength should urgently consult a specialist as soon as possible.
Only with the help of imaging procedures, for example magnetic resonance imaging (MRT), can the herniated disc be diagnosed as such without any doubt.
Read extensive information on this topic under: Disc herniation diagnosis
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
MRI of a herniated disc
Magnetic resonance imaging (MRI) is used to confirm the diagnosis of patients who are suspected of having a herniated disc.
However, before the production of an MRI can be initiated, the suspected diagnosis should be confirmed with the help of other diagnostic measures.
Above all, a detailed doctor-patient discussion (anamnese) be performed. The symptoms present in the affected patient can indicate a herniated disc.
In addition, an orienting physical examination should be performed before the MRI is initiated.
If there is a suspicion of a herniated disc, it should be noted that imaging procedures, such as computer (CT) or magnetic resonance imaging (MRT), must only be performed on people with pronounced symptoms.
Especially in patients who suffer from sensory disturbances (e.g. numbness and / or tingling), an MRI must be performed. This also applies to patients with pronounced reduction in muscle strength in one or more extremities.
Among the imaging procedures possible in the diagnosis of a herniated disc, the following applies: the MRI to this day as First choice means.
Compared to conventional X-rays, MRI not only reveals bony structures, but above all Reliably assess parts of tissue, nerve roots and intervertebral discs.
In addition, the production of a Magnetic resonance imaging (MRI) compared to computed tomography the advantage that the patient to be examined no radiation is exposed.
Both imaging methods are used in the diagnosis of a herniated disc to be more detailed Sectional images of the individual spine segments to make.
The MRT is mainly based on the physical principle of Nuclear magnetic resonance. In simplified terms, this means that the individual sectional images are generated by using electromagnetic waves within a strong magnetic field.
Of the Disadvantage of the MRI is primarily based on the fact that common replacement methods (e.g. computed tomography) only require a fraction of the working time of an MRI.
With regard to the quality of the individual cross-sectional images, computed tomography and magnetic resonance tomography (MRT) can usually be chosen no noticeable difference be perceived.
The choice of the most appropriate imaging modality depends on other factors, such as the Radiation exposure and the Investigation time, from.
Although the patient to be examined is not exposed to any radiation during the production of an MRI, there are some restrictions to be observed with this examination method.
An MRI can be used to diagnose a herniated disc not be made on patients who have a pacemaker.
An MRI is also included Carriers of electromechanical implants, for example Cochlear implants or implanted pain pumps, not suitable.
In these patient groups, the diagnosis of “herniated disc” must be confirmed with other imaging methods.
Since the conventional x-ray not suitable for displaying the intervertebral discs, computed tomography must be used.
However, examinations using MRI in people with Hip prostheses, artificial heart valves and dentures.
MRI of a herniated disc in the cervical spine
A herniated disc in the area of the cervical spine (Cervical spine) can have serious consequences for the affected patient.
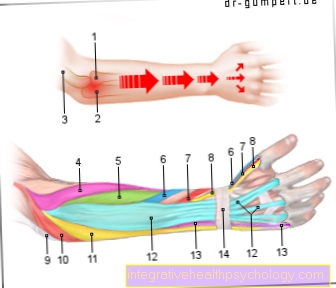
In most cases, the herniated disc of the cervical spine shows itself mainly through the appearance of sensory disturbances in the form of Numbness and / or Tingling in the arms. In addition, sustained pressure on the nerve roots of the cervical spine can cause a increasing muscle weakness in the arms to lead. These complaints often recede over a period of time.
For this reason, affected persons should urgently consult a specialist promptly and have the presence of a herniated disc of the cervical spine checked.
In the diagnosis of a herniated disc in the area of the cervical spine in people with particularly pronounced complaints Imaging procedures play a crucial role. So far, the production of a magnetic resonance tomography (MRT) has been considered in the diagnosis of a herniated disc of the cervical spine First choice means.
During the actual examination, the patient is placed on his back. Since the MRI of the cervical spine is carried out in an almost completely closed tube, the examination can be performed for people with claustrophobia (Claustrophobia) can be very stressful.
For the production of optimal sectional images, however, it is particularly important that the patient to be examined during the approximately 20-minute examination not moved. Otherwise the sectional images will be blurred and cannot be used to diagnose the herniated disc.
MRI of a herniated disc in the lumbar spine
Of the Herniated disc of the lumbar spine (lumbar spine) belongs next to the herniated disc to the Cervical spine (cervical spine) the most common forms of this disease.
In many cases, based on the existing symptoms, even without imaging procedures (e.g. MRI) a Suspected diagnosis be asked.
People who have a herniated disc of the lumbar spine often suffer from persistent, severe back painthat radiate down to the buttocks and legs.
In addition, a herniated disc of the lumbar spine is often evident Sensory disturbances such as numbness and / or tingling and pronounced limitations in muscle strength.
Even in the case of a herniated disc of the lumbar spine, diagnosis by means of MRI is not always necessary. If the symptoms are less pronounced, there is usually no need to prepare an MRI. An MRI should only be performed in patients with pronounced symptoms.
Using the sectional images of the individual spinal column segments obtained by the MRT, the extent of the disease can be reliably determined and a appropriate treatment be initiated.
The MRI is also considered imaging for a herniated disc in the lumbar spine First choice method. In contrast to conventional X-rays, both the intervertebral discs and the nerve roots can be reliably depicted with the help of MRI. When looking at a conventional X-ray, however, only the bony structures of the spine can be adequately assessed.
In addition to the MRI, the Computed Tomography to diagnose a herniated disc in the lumbar spine. However, since this examination procedure results in considerable radiation exposure for the patient to be examined, MRI is usually preferred.
Only in patients for whom the present symptoms may possibly coincide with a recent one traumatic event CT should preferably be performed.
This is due to the fact that an MRI scan of the spine takes about 20 to 30 minutes. On the other hand, suitable CT slice images of the individual spinal column sections can be made within a few seconds.
This is how long an MRI takes for a herniated disc
In contrast to other imaging methods such as CT, X-ray or sonography (ultrasound), MRI is an examination that takes a little longer. Most MRIs can be done within twenty to thirty minutes. In the case of an MRI for a herniated disc, the examination can take longer if, for example, the entire spine is to be mapped.
If, on the other hand, only the thoracic spine is specifically photographed, for example, the examination is usually done faster. Since the MRI takes images at a distance of millimeters, you have to lie absolutely still during the examination. If necessary, if the examined person is restless, some images have to be repeated due to camera shake. This can also extend the examination by a few minutes.
Contrast media necessary?
An MRI examination can in principle with or without the administration of a special contrast agent be performed. However, when confirming the suspected diagnosis of "slipped disc", it is not necessary to give it.
With the help of the contrast agent can only inflammatory changes or tumors in the area of the spine.
MRI with contrast agent
Magnetic resonance tomography (MRT) can be used in the course of diagnosis if a herniated disc is suspected, both with and without Contrast media be performed. In this context, however, it should be noted that an MRI is required to assess the individual spinal column segments (including the intervertebral discs) without contrast media is completely sufficient.
A MRI with contrast agent is only considered useful in the diagnosis of a herniated disc if other causes of the symptoms are to be excluded. Especially inflammatory processes in the area of the spine and tumors can be safely excluded by making an MRI with contrast agent.
The reason for this is the fact that the contrast medium administered via the venous vessels is located in the area of inflammations and tumors increasingly enriched. Affected areas appear clearly colored in the individual sectional images and can be easily identified in this way.
The Band washers however, even if there is a herniated disc, they usually do not absorb any contrast medium.
For this reason, making a MRI without contrast agent to confirm the diagnosis of a herniated disc is in most cases completely sufficient.
Injecting a herniated disc under MRI
In the case of a herniated disc, an injection can be made for symptomatic therapy. A local anesthetic (a local anesthetic) is usually injected where the disc irritates nerves in the spinal cord. In addition, some cortisone is often added, which can virtually shrink the intervertebral disc. As a result, the herniated disc presses less on the nerves, which can alleviate the symptoms.
So that you hit exactly the right place when injecting, the injection usually takes place under imaging control. This can be a sonography (ultrasound) if visibility is good. If the herniated disc cannot be adequately depicted with an ultrasound, the injection is performed under MRI control. On the MRI image, the first step is to plan the way in which the herniated disc will be injected. MRI images can then be taken repeatedly while the needle is being inserted, so that the position of the injection needle can be checked again and again.
Read more on the topic: Cortisone for a herniated disc or cortisone injection - areas of application and side effects
MRI or X-ray?
If a herniated disc is suspected, you must not necessarily imaging can be used. Only in people who have severe complaints, for example Sensory disturbances such as numbness or tingling diagnosis should be confirmed with the help of an imaging procedure.
Affected patients often ask themselves in this context whether MRI, CT or X-ray best suited for the representation of the individual spine segments.
While magnetic resonance tomography (MRT) works completely without radiation exposure, the patient being examined is exposed to considerable doses of radiation with CT or X-ray.
In general, it can be assumed that the radiation exposure is many times higher when performing a CT. In this context, however, it must be noted that the spine is usually displayed several x-rays must be made. With regard to radiation exposure, it is therefore almost irrelevant whether the diagnosis is made using CT or X-ray is provided.
Nevertheless, the X-ray is considered to be in the diagnosis of a herniated disc not suitable. The reason for this is the fact that only bony structures on x-rays can be usefully mapped. Both that Nerve tissue, as well as the Band washers can, however, only be visualized with the help of an MRI or CT.
MRI or CT?
Basically is suitable both magnetic resonance and computed tomography to diagnose a herniated disc. The question of whether an MRI or CT scan is the more suitable imaging method for an affected patient depends on various factors.
In this context, it should be noted that high Amounts of radiation act on the patient to be examined. The MRI, on the other hand, works completely without harmful radiation.
For this reason, the choice of whether to perform an MRI or a CT should initially fall on the preparation of an MRI.
For people who have a Pacemaker or electromechanical implants (e.g. cochlear implants), you cannot choose between MRI or CT. In these cases the cross-sectional images of the spine must be inevitably with the help of a CT be made.
In addition, when choosing between MRI or CT it must be borne in mind that in patients who are under very severe back pain and a pronounced Sciatica irritation suffer with the help of Computed tomography (CT) a more precise statement about the cause of the pain can be made. A herniated disc can be reliably diagnosed as such both in the MRI and in the cross-sectional images of the CT.
Can a herniated disc be missed on an MRI?
The MRT examination (abbreviation for magnetic resonance tomography) is a so-called slice imaging. The body region to be examined is mapped layer by layer. Typically, images are created that were recorded a few millimeters apart. In theory, a very precise three-dimensional image reconstruction of the examined body region is possible.
Due to its physical background, the MRI is particularly suitable for depicting structures such as bones, ligaments and tendons. Therefore, an MRI is preferred in the case of a herniated disc. Most of the herniated discs are discovered in the pictures. However, a particularly small herniated disc can hide between the individual slices and therefore be overlooked. In addition, one often finds findings that do not cause any complaints in the person concerned. Therefore, when assessing the MRI images, a professional look from a radiologist is required.
Claustrophobia in the MRI
Since the examination with the help of an MRI must be carried out in an almost completely closed tube, the procedure can be used for people who are under Claustrophobia (claustrophobia) suffer, be very stressful.
However, claustrophobia is not an exclusion criterion for confirming the diagnosis of "herniated disc" with the help of an MRI. Affected patients should report the problem to the medical staff before the start of treatment. Various sedatives can help to ensure that the MRI scan can still be carried out without any problems.
That is the cost of an MRI for a herniated disc
The MRI for a herniated disc usually costs between 500 and 800 €, depending on which back area is to be mapped. If the MRI is performed on the basis of a medical indication, the health insurance will normally cover the costs of the examination.
However, the indication for an MRI in the case of a herniated disc is rather reserved. Back pain of all kinds is initially treated conservatively with exercise therapy. Therefore, an exact diagnosis of the cause is not always necessary, which is why one often saves the MRI and tries to alleviate the symptoms with general therapy.
Immediate imaging is of course carried out in urgent suspicions.