Muscle weakness
introduction
Muscle weakness (myasthenia or myasthenia) is a condition in which the muscles do not correspond to their actually normal state of performance, which means that some movements cannot be performed or cannot be performed with full force.
Muscle weakness can vary in severity and range from a slight feeling of weakness to manifest paralysis.
There are various reasons for muscle weakness, the most common of which are completely harmless in nature. However, muscle weakness can also be a sign of a serious illness and should therefore be clarified by a doctor.
The most common causes of muscle weakness are briefly explained here.

Simple and disease-independent causes of muscle weakness
A simple muscle weakness is a weakness of the muscles that occurs alone, i.e. not in the context of another disease. It is the most harmless form and is mostly caused by an improper diet, often in connection with a lack of exercise. If the food is lacking in important minerals or vitamins, this can become noticeable as weak muscles, often accompanied by a general feeling of tiredness.
For the muscles to work correctly, iron and magnesium are particularly important. After a considerable amount of physical exertion, short-term muscle weakness can also occur, which is then completely natural. Also as a side effect of a flu-like infection, weakness and pain in the muscles can occur.
Muscle weaknesses can also occur in the context of stressful situations or through excessive demands.
Psychosomatic muscle weaknesses are based on a non-organic cause, i.e. those affected are physically healthy but still suffer from complaints.
Taking certain medications can also weaken the muscles.
After an operation on the hip or after the insertion of an artificial hip joint, a temporary muscle weakness can also occur postoperatively.
Muscle weakness due to a lack of vitamins
A vitamin deficiency can lead to a slight form of muscle weakness, often combined with fatigue. Relevant vitamins, the deficiency of which can lead to muscle weakness, are, for example, vitamins B12, B1, C, D and E.
Vitamin B12, also known as "cobalamin" or "extrinsic factor" in medicine, is found in foods such as fish, meat, eggs and dairy products.
Vitamin D is the only vitamin that humans can produce themselves, but certain prerequisites must be met or appropriate conditions exist so that production is also possible. For example, sunlight is able to convert a precursor through the skin. Therefore, especially in winter or in countries with low UV exposure, many have a vitamin D deficiency.
However, the exact and individual causes for the respective vitamin deficiency are again very variable. The most common reason, however, is usually an incorrect and unbalanced diet low in vitamins.
Nevertheless, there are also risk groups or certain circumstances such as pregnancy or stress that make those affected more susceptible to a vitamin deficiency, so that muscle weakness is more likely. In general, the respective vitamin deficiency can be compensated for by purely symptomatic therapy, i.e. the administration of the missing vitamin. The body is able to recover relatively quickly and well from a vitamin deficiency.
In addition to the vitamins, the two nutrients iron and magnesium also play a decisive role in the development of muscle weakness. A balanced diet should therefore always be observed as a preventive measure.
Muscle weakness after exercising
Muscle weaknesses that occur after exercise are completely normal after the muscles are used appropriately and should not be a cause for concern.
When the muscles work, they consume energy.
With a high level of stress and intensity, the body produces lactate in addition to energy under anaerobic conditions, i.e. without the presence of oxygen. If the last-mentioned metabolic product accumulates in the working muscles, it becomes too acidic. This is the moment when the feeling of no longer having any strength arises and there is temporary muscle weakness. As soon as the lactate has been metabolized with the help of oxygen again after exercising, the muscle weakness disappears.
In addition, new training requirements in terms of intensity and movement patterns often lead to muscle twitching in the stressed muscles after the first few times, with the subsequent feeling of muscle weakness. Unless the muscles are stubbornly sore, the muscle weakness disappears relatively quickly.
Therapeutically, there are simple approaches to reducing muscle twitching and the associated muscle weakness or muscle weakness alone after exercise. A balanced and vitamin-rich diet including a sufficient supply of magnesium as well as a varied training program and effective warm-up and stretching exercises also serve as a preventive measure against muscle twitching and weakness.
With regard to the metabolic product lactate, an exact lactate analysis can be carried out to optimize performance, whereby one's own individual performance limit can be determined.
Which drugs can cause muscle weakness?
There are actually a few drugs in medicine that can cause muscle weakness.
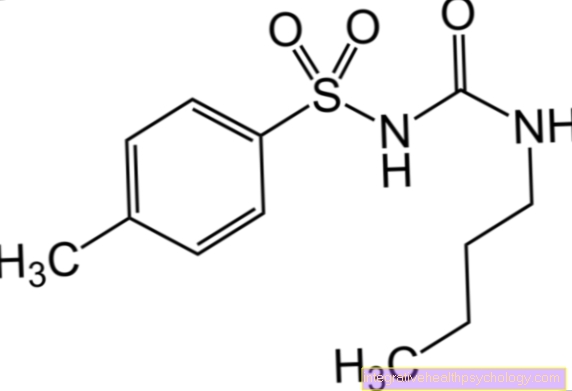
Such drug-induced muscle weakness can be triggered by taking the drugs D-penicillamine and chloroquine.
D-penicillamine plays a role in rheumatism therapy and in the treatment of heavy metal poisoning, chloroquine also in the therapy of some rheumatic diseases, but also in the prevention and therapy of malaria.
If muscle weakness occurs, the medication should be discontinued in consultation with the doctor. In the context of long-term cortisone therapy, muscle weakness can also develop, often accompanied by other symptoms.
Muscle weakness from cortisone
Muscle weakness is one of the possible side effects in the context of long-term drug cortisone therapy. In extreme cases, the muscle weakness can develop into muscle atrophy, i.e. muscle wasting.
In general, muscle weakness does not occur in isolation during cortisone therapy, but is accompanied by other symptoms. These include, for example, the weakening of the immune system, bleeding in the skin, edema and depressive episodes. There are also some contraindications to the use of cortisone. These contraindications should be clarified before taking.
However, if there are side effects when taking cortisone, such as muscle weakness, the drug should be discontinued after consulting the prescribing doctor.
Psychosomatic muscle weakness
Psychosomatic means that there is no organ-related trigger for the occurrence of muscle weakness, but that the complaints are based on mental problems or stress.
A detailed examination of one's own health or one's own illnesses beyond a natural level can provoke the occurrence of psychosomatic muscle weaknesses. Muscle weaknesses based on psychosomatic reasons are also closely related to muscle weaknesses that arise due to stress, as this is also a stressful situation. Depression also increases the risk of psychosomatic muscle paralysis. Without any organic connection, those affected complain of so-called "pseudoneurological" symptoms such as muscle weaknesses, but also symptoms of paralysis or abnormal sensations.
Diagnosing psychosomatic muscle paralysis as such is often very difficult and takes a long time, as all possible organic causes must first be ruled out and those affected often do not show any insight into the disease or do not accept that the muscle paralysis comes from the psyche.
Muscle weakness from stress
When stress is mentioned as a trigger for muscle weakness, it is referred to as distress, i.e. negative stress.
Stress in the form of physical, emotional or illness-related stress on the physical organism can lead to a vitamin deficiency. This in turn results in muscle weakness. The reason for this is an increased breakdown of vitamins by the body, as they are more needed in a stressful state.
There is a very special connection between stress, vitamin deficiency and muscle weakness, for example in the case of vitamin C and carnitine. Vitamin C is involved in the synthesis of carnitine, the chemical compound of two amino acids. Insufficient production due to a vitamin deficiency can in turn lead to disorders of the muscular metabolism, i.e. muscle weakness.
Muscle weakness after a hip replacement
Immediately after a hip replacement surgery, i.e. after a total endoprosthesis has been inserted into the hip joint, muscle weaknesses in the hip area are completely normal and harmless. After all, the operation is an invasive procedure in which the muscles are exposed to enormous tensile and tension forces so that the surgeon can easily reach the hip joint to be operated on.
The muscle weakness therefore reflects a kind of regeneration phase. The initial muscle weakness is often accompanied by pain caused by the wound on the operated joint.
The muscle weakness usually regresses after a short time. In order to strengthen the muscles, physiotherapy is usually ordered postoperatively. However, if the muscle weakness does not improve significantly in the further course of healing, it must be excluded that nervous structures were injured during the surgical procedure. This can be verified with the help of special diagnostic measures and treated accordingly if necessary.
What are the causes of muscle weakness in the legs?
Muscle weaknesses generally manifest themselves primarily in the extremities, i.e. also in the legs, and only affect the breathing or swallowing muscles at a later point in time.
There are a number of muscle-specific diseases that weaken the leg muscles.
These include myasthenia gravis, multiple sclerosis, botulism, spinal muscular atrophies, Duchenne muscular dystrophy in childhood and amyotrophic lateral sclerosis in old age.
Another cause of muscle weakness in the legs is the herniated disc. Depending on the severity and location in the lumbar or sacral vertebral area, certain muscle groups in the leg can be affected. In the case of nerve compression, for example in the context of a herniated disc, in addition to initial discomfort such as numbness and tingling sensation, muscle weaknesses and even muscle paralysis can occur.
The intervertebral discs between vertebrae L4, L5 and S1 are often affected.
In the case of an L4 syndrome, a muscle weakening can be recognized by a reduced knee extension, in the case of L5 and S1 syndromes by a reduced foot lift and foot drop.
In addition to the triggers mentioned above, general illnesses that do not directly relate to the leg muscles can also trigger a muscle weakness there.
These include, for example, depression, metabolic disorders such as an underactive thyroid, anemia or infectious diseases. It is important that those affected be neurologically examined in the event of long-term muscle weaknesses in order to be able to rule out serious diseases.
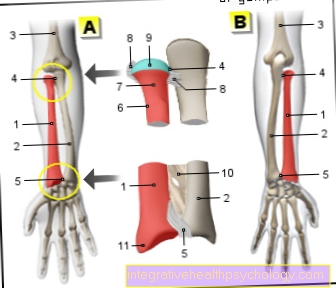
What are the causes of muscle weakness in the arms?
As with the muscular weakness of the legs, the arms, as part of the extremities, are a common place of manifestation.
A weakening of the arm muscles triggered by the spine can result from a herniated disc at vertebral level C5-C8. Here, for example, the biceps can no longer be adequately innervated in the context of a C6 syndrome, which leads to its weakening and thus a weakening of the arm flexion.
Otherwise, various general diseases such as an underactive thyroid, vitamin deficiency or stress can cause muscle weakness.
Diseases that specifically affect the muscles, such as spinal muscular atrophy, myasthenia gravis, multiple sclerosis or amyotrophic lateral sclerosis, should also be mentioned here.
A new aspect as a reason for a weakening of the arm muscles is the stroke. Due to an insufficient supply of certain brain areas with oxygen in the case of cerebral haemorrhage or blockages of the blood-supplying vessels, i.e. a thrombosis or embolism, various functions and structures can be affected. If the stroke occurs in an area that represents the arm, the arm muscles can weaken or even become paralyzed. In general, long-lasting muscle weaknesses in the arms are definitely in need of clarification.
Basic diseases as a cause of muscle weakness
Various diseases can be associated with muscle weakness, including:
- Herniated discs
- Muscle inflammation (Myositis)
- Circulatory disorders
- the autoimmune disease myasthenia gravis
- Inflammation of the nerves
- botulism
Poisoning with botulinum toxin, which can get into the body through spoiled food, for example - Arterial Disease
- Diabetes mellitus
- Metabolic diseases (especially thyroid disorders)
- malignant cancers
- Parkinson's disease
- stroke
- Amyotrophic lateral sclerosis (ALS)
Thyroid dysfunction as a cause of muscle weakness
At first glance, it may seem astonishing to the layperson if the reason for your own muscle weakness is the thyroid gland.
However, the thyroid gland is an organ that twists many of the metabolic controls and is responsible for our body growth.
Over- or under-functioning of the thyroid can therefore unbalance the body and trigger a wide variety of complaints.
In the case of an underactive thyroid, i.e. hypothyroidism, this includes muscle weakness in addition to many other symptoms. Symptomatic hypothyroidism should therefore always be treated.
Read more on the topic: Symptoms of hypothyroidism
A disruption of the thyroid function can also be very relevant in the newborn. A so-called “congenital hypothyroidism”, i.e. a congenital underactive thyroid, must be clarified as part of the newborn screening. Immediately after birth, it can lead to reduced body temperature (hypothermia), muscle weakness (muscle hypotonia), laziness to drink, constipation and much more. Unrecognized and untreated, such an underfunction in children can have serious consequences such as mental retardation in addition to muscle weakness.
In general, the thyroid values should be checked in the event of general symptoms of exhaustion and muscle weakness. Hypothyroidism and the associated muscle weakness can be treated very easily simply by taking the deficient thyroid hormones.
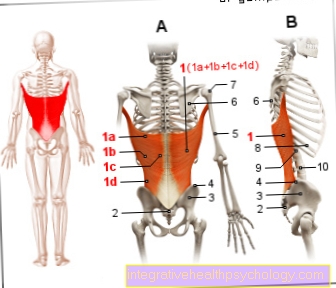
muscular dystrophy
Muscle wasting (muscular dystrophy) is a hereditary disease. There are different types of muscular dystrophy. What they have in common is that a deficiency in a protein called dystrophin, which is very important for proper muscle function, leads to gradual muscle wasting.
In the Duchenne type, this protein is completely absent, in the Becker type it is just not sufficiently available. Accordingly, the Duchenne type is associated with the more severe clinical picture, the disease becomes noticeable earlier, is characterized by a faster progression of paralysis and confines affected persons to a wheelchair at an early stage. Patients with muscular dystrophies usually die from failure of the respiratory muscles at some point.
stroke
A stroke occurs when a certain area of the brain is no longer adequately supplied with oxygen and therefore no longer functions properly. This can happen either as part of a cerebral haemorrhage or a blockage of a brain vessel (thrombosis, embolism). If the area of the brain that is responsible for controlling the muscles is affected, the stroke can manifest itself in the form of muscle weakness or even complete paralysis. These symptoms appear on the opposite side of the affected hemisphere.
Read more on the subject at: Signs of a stroke
Multiple sclerosis (MS)
Multiple sclerosis is a chronic inflammatory disease of the nervous system. The first manifestation of this disease is mostly in young adulthood with no apparent cause. It is characterized by the fact that the medullary sheaths of the nerve fibers perish. However, these are absolutely necessary to enable the rapid transmission of impulses along the nerve fibers. Depending on which nerve fibers are affected by the shrinkage of the medullary sheaths, patients may have motor or sensitivity disorders.
Concomitant symptoms
Isolated muscle weakness is rare. Much more often, in addition to muscle weakness, muscle twitching and the resulting impairment of consciousness, gait, swallowing, vision and speech disorders occur.
In the case of trivial causes such as a magnesium deficiency, muscle weakness is also accompanied by muscle cramps.
In general, the symptoms that accompany muscle weakness are always related to the actual disease or the trigger. Therefore, a very wide range of accompanying symptoms can occur.
A first example is an underactive thyroid (= hypothyroidism). Muscle weakness is just one of many symptoms here. Symptoms such as weight gain, constipation, a slow heart rate (bradycardia) and listlessness are also common. The body is so to speak slowed down and throttled in its activity and performance in many aspects.
Furthermore, so-called “neonatal myasthenia”, i.e. muscle weakness in the newborn due to an autoimmune disease, can also lead to weak suction, drooping eyelids and insufficient breathing.
Finally, accompanying symptoms in the context of long-term cortisone therapy are mentioned as an example. Cortisone is a drug that has a lot of side effects, so that, in addition to muscle weakness, symptoms such as glaucoma (= green starration), palpitations and growth inhibition in the child can occur. The immune system is also weakened by the cortisone, which has corresponding consequences. In old age, cortisone affects not only muscles but also bone stability, making osteoporosis more likely.
Muscle weakness and twitching
Not all muscle twitches are the same. They offer a wide variety of possible causes for sometimes harmless twitching, but also for serious illnesses.
The decisive factor is the intensity of the muscle twitching, but also the frequency, i.e. whether the muscle twitching occurs at regular intervals or rather sporadically. Depending on how much muscle tissue is involved in the twitch, it is not only noticeable for those affected, but also recognizable as movement for outsiders.
Benign muscle twitching occurs, for example, often in stressful phases of life, with hypoglycaemia, magnesium deficiency or as side effects of medication. Such muscle twitches are only uncomfortable for the moment and disappear as soon as the triggering factors are reduced or eliminated. Muscle weakness does not occur in this context.
The combination of muscle twitching and weakening or a weakness of certain muscles following the twitching can be part of serious illnesses. One example is amyotrophic lateral sclerosis, a degenerative nerve disease in which muscle twitching occurs initially. In the further course of the disease, there are mainly muscle weaknesses caused by muscle wasting, which can continue up to paralysis. Muscle twitching should be clarified by a doctor if it persists for a long time without any banal connection such as stress or extreme tension.
Diagnosis

To the Cause of muscle weakness To be able to determine is initially one for the doctor detailed survey of the medical history (Anamnesis) important. Questions that can be helpful in making a diagnosis include: since when the muscle weakness has existed, which ones Muscles it concerns whether there was a certain event (such as an accident) that immediately preceded the muscle weakness, whether there are other complaints (for example Sensory disturbances), whether it Medication that are taken regularly and whether the patient has any known pre-existing conditions (such as Diabetes mellitus, Multiple sclerosis or other).
Following the anamnesis, the doctor will further examinations depending on the suspicion carry out. For one is one physical examination of great importance. Here is exactly that existing force checked in the muscles for any existing ones Sensory disturbances wanted and Reflexes are checked. In addition, a blood test can be useful for many. More specific examination methods find their justification with a justified assumption of certain diseases. On the one hand, this includes imaging procedures such as Computed Tomography (CT) or the Magnetic resonance imaging (MRI), taking muscle tissue (muscle biopsies) that Electromyography (EMG), an examination of the cerebral water (using a CSF puncture), electroneurography (ENG) or the Electroencephalography (EEG). In addition, it may make sense to carry out a genetic test or have the examination by a specialist, for example a ENT doctor or one Ophthalmologist.
therapy
The Treatment of muscle weakness depends on its cause. Both simple forms it is usually enough to go to one healthy eating to pay attention to this if necessary vitamin- or to fortify nutrient supplements (usually magnesium or iron). If muscle weakness occurred as part of a simple infection, it will heal without treatment as soon as the infection disappears.
However, if a neurological disease the muscle weakness caused, so is often one extensive, sometimes lifelong therapy necessary. With some of the diseases like that Multiple sclerosis the muscle weakness can then not heal completely, but at least improve in terms of symptoms. In addition to specific measures based on the disease at hand, there are muscle weaknesses caused by the disease general treatments as the physiotherapy, physical therapy and physical therapies (Massages, electrical treatments, alternating and exercise baths and heat treatments) are used.
Prevent one can unfortunately the muscle weakness only in its simple form. It is enough to click on one healthy balanced diet rich in minerals and vitamins and regular exercise to drift. Since no causes are known or genetic errors are responsible for the diseases that are associated with muscle weakness, one can unfortunately do nothing to prevent them.
Duration of muscle weakness
The duration of muscle weakness cannot be defined in general, as it varies individually depending on the cause.
Muscle weakness can be treated the quickest if there is a vitamin deficiency or if there is severe physical and psychological stress. But many other triggers also cause muscle weakness that is only temporary.
With correct treatment, the muscle weakness can disappear after a few days to weeks. As long as no worse, partly hereditary disease could be the cause of the muscle weakness, this weakness is usually reversible and therefore relatively harmless.
Otherwise, the muscle weakness can last for life and even worsen over the course of time and ultimately be the cause of death.
forecast
The prognosis of muscle weakness can only be made depending on its severity and cause. Reversible causes such as a vitamin deficiency, stress or certain medications have a good prognosis.
The drug-induced muscle weakness, for example, is very harmless and usually decreases quickly after the drug is discontinued. However, there are also a few diseases with a rather poor prognosis.
In the specific case of amyotrophic lateral sclerosis (= ALS), for example, the prognosis is very poor, as this degenerative nerve disease ultimately leads to the patient being unable to breathe due to an inadequate respiratory excursion caused by the weakened respiratory muscles. At diagnosis, the mean survival time is usually only 2 to 5 years. Only 10% live longer than 10 years in exceptional cases.
The exact prognosis can therefore only be made if a clear clinical picture for the muscle weakness has been diagnosed. Due to the sometimes poor forecasts, no premature forecast should be made.
Muscle weakness in the baby
Recognizing and correctly diagnosing muscle weakness in babies is quite difficult. Before the age of 6 months it is hardly possible to recognize a relevant muscle weakness.
A first clue may be that the baby is unable to roll over on its stomach or that it is very strained to suckle the breast.
A delay in learning to crawl can also be seen as the first sign. A medical evaluation of the muscle weakness is very important here, as there are muscle or nerve diseases that can be inherited and / or occur at an early age.
The term "floppy infant", meaning a "flaccid" child, defines the phenomenon of a whole-body, flaccid muscle tone, which is automatically associated with muscle weakness. The causes for such a reduced muscle tone are very diverse. Therefore, the occurrence of a noticeable muscle weakness must be clarified, as a number of causes requiring treatment come into question.
In babies, what is known as “neonatal myasthenia” or “congenital hypothyroidism” can trigger muscle weakness. The first-mentioned disease is an autoimmune disease that is associated with the formation of auto-antibodies, which in turn prevents the transmission of excitation necessary for muscle activity.
“Congenital hypothyroidism”, ie thyroid function, is a serious illness in early childhood, as it can, in the worst case, lead to mental retardation. The initially manifested muscle weakness is a comparatively harmless symptom, but should be the first sign to attract attention.
Furthermore, genetic diseases with the symptom of muscle weakness already manifest in the baby. The Prader-Willi syndrome or the more well-known Down syndrome or trisomy 21 should be mentioned here, for example.
As a general rule, early physiotherapeutic treatment of muscle weakness can be very useful and effective in some cases at an early age. Depending on the disease, further therapeutic measures may be indicated.
Muscle weakness in the child
In medicine there are a number of reasons why muscle weakness develops in childhood.
Causes can be an unbalanced diet resulting in a vitamin deficiency, drug-induced muscle weakness or hypoglycaemia.
Serious diseases, some of which are genetic, can also be responsible for muscle weakness. Although congenital myasthenia can already occur in the baby, it can also develop in the course of the child's development.
The same applies to an underactive thyroid. Also worth mentioning are the so-called “congenital muscular dystrophies”, which are hereditary muscle diseases.
The Duchenne type from the group of muscular dystrophies typically manifests itself in the 3rd to 5th year of life and is based on a mutation of a muscular protein. The muscle weakness can then be explained by a deterioration of the muscles. First of all, signs of paralysis and slight muscle wasting, especially in the pelvic area, but later also in the shoulders and extremities, which is accompanied by a weakening of the corresponding muscles.
In addition, forms of spinal muscular atrophy at different ages can be responsible for muscle weakness. An early form, the so-called "infantile form" or "Werding-Hoffmann", occurs before the first year of life and has a very poor prognosis with a mean survival time of 1.5 years. In contrast to this, a "juvenile form" that manifests itself later, also called "Kugelberg Welander", has a hardly limiting life expectancy.
As with the baby, muscle weaknesses in the child should definitely be clarified by a doctor so that appropriate measures can be taken in the event of possible treatable diseases.