Pelvic inflammation
Synonyms
Medical: pyelonephritis
Upper UTI (urinary tract infection), pyonephrosis, urosepsis
definition
In the Pelvic inflammation (Pyelonephritis) is an interstitial (i.e. between the actual kidney tissue), bacterial, tissue-destroying (destructive) inflammation of the kidney and des Pelvic calyx system. A Pelvic inflammation can occur unilaterally or bilaterally.

frequency
It is one of the most common kidney diseases. Approximately 10-20% of the population is affected. Chronic (recurring) pyelonephritis / inflammation of the renal pelvis, if it remains undetected, can lead to complete (terminal) kidney failure in approx.
Women are affected 2 to 3 times more often than men.
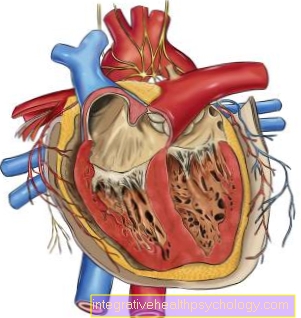
Illustration of pelvic inflammation

Pelvic inflammation
(bacterial infection of the
Renal pelvis)
Pyelonephritis
- Bacteria - Escherichia coli,
Enterococci, Proteus,
Klebsiella etc. - Renal artery - Renal artery
- Right kidney - Ren dexter
- Ureter - Ureter
- Left kidney - Ren sinister
- Calyx - Calix renalis
- Renal medulla - Medulla renalis
- Renal pelvis - Pelvis renalis
- Kidney bay (with filling fat) -
Renal sinus - Renal cortex - Renal cortex
- Urinary bladder - Vesica urinaria
- Urethra - urethra
- Prostate gland - prostate
(healthy left, enlarged right)
A - Acute primary (uncomplicated)
Pelvic inflammation
(by bacteria in the urinary tract
triggered)
B - Acute secondary (complicated)
Pelvic inflammation
(due to drainage disturbances, congestion
in urinary tract, enlarged prostate)
You can find an overview of all Dr-Gumpert images at: medical illustrations

- Renal cortex - Renal cortex
- Renal medulla (formed by the
Kidney pyramids) -
Medulla renalis - Kidney bay (with filling fat) -
Renal sinus - Calyx - Calix renalis
- Renal pelvis - Pelvis renalis
- Ureter - Ureter
- Fiber capsule - Capsula fibrosa
- Kidney column - Columna renalis
- Renal artery - A. renalis
- Renal vein - V. renalis
- Renal papilla
(Tip of the kidney pyramid) -
Renal papilla - Adrenal gland -
Glandula suprarenalis - Fat capsule - Capsula adiposa
You can find an overview of all Dr-Gumpert images at: medical illustrations
causes
Pyelonephritis / inflammation of the renal pelvis is mainly caused by bacteria such as Escherichia coli, Enterococci, Proteus, Klebsiella, Pseudomonas aeruginosa or staphylococci. Due to the close proximity of the urethra and anus, these germs are voided by smear infection (e.g. with toilet paper). a. easily transferred to the urinary tract in women, from where they rise via the urinary bladder to the renal pelvic calyx system (NKBS). The bacteria very rarely reach the renal pelvis via blood or lymph vessels.
The infection usually begins in the so-called papillae and then spreads in a wedge shape to the renal cortex (see also kidney anatomy). A pus cavity (abscess formation) within and around the kidney is possible, but very rare. Ultimately, a wedge-shaped scar with retraction on the kidney surface can occur.
Read more interesting information at: Kidney abscess
Risk factors
Various factors can promote kidney inflammation:
- Pregnancy (pyelonephritis gravidarum)
- Lack of estrogen (female sex hormone)
- Metabolic diseases (Diabetes mellitus, Gout)
- Medication (certain pain relievers, antibiotics)
- Prostate enlargement with backlog of urine, as well as any form of urinary flow disorder
- Paraplegia
Classification
One can differentiate between different forms of pyelonephritis / renal pelvic inflammation, which will be discussed in more detail below, either according to the course (acute or chronic) and according to the development (primary / uncomplicated or secondary / complicated).
To form:
- Acute primary (uncomplicated) pyelonephritis / pelvic inflammation
- Acute secondary (complicated) pyelonephritis / pelvic inflammation
causes
It is often caused by the bacteria E. coli, Proteus or Klebsiella.
Symptoms
Flank pain on one or both sides occurs, which can also extend into the groin or the scrotum (scrotum). Those affected complain of a high fever of up to 40 ° C with chills, severe feeling of illness, weakness, loss of appetite and nausea. If there is also inflammation of the bladder (cystitis), pain when urinating (dysuria), frequent urination (pollakiuria) and bladder cramps occur. There may also be changes in the urine. This can appear cloudy to flaky, and blood in the urine is also possible.
diagnosis
During the medical examination, tenderness and tapping pain are indicated over the affected kidney. The urine contains white blood cells (leukocyturia), invisible blood (microhematuria), bacteria (significant bacteriuria from 105 per ml) and some protein (weak proteinuria).
The ultrasound shows a “swelling” of the diseased kidney or even an enlarged kidney. Comorbidities should be excluded with the help of an X-ray of the abdomen (abdomen) and a urogram. For urography (urogram), an iodine-containing X-ray contrast agent is injected into the vein after the X-ray of the abdomen overview (blank image). The kidneys are then after 7 and 15 min. x-rayed. The excretion of the contrast medium by the kidneys can provide information about the anatomical relationships of the renal cavity system. The drainage conditions via the ureters and the urinary bladder can also be assessed.
A urine test is often done at the beginning. Further information can be found on our website Urinalysis
This urine test can also easily be carried out at home using a rapid test, especially to examine an initial suspicion. Read more about this at: Rapid Cystitis Test
therapy
First of all, the patient should be strict bed rest adhere to and a lot liquid to take in. Antibiotics should be taken immediately to Taking a urine culture (urine test for bacteria) and still in front When the result is received. So-called broad-spectrum antibiotics (e.g. cephalosporins) are recommended for eight days. Broad-spectrum antibiotics are effective against a particularly large number of types of bacteria.
Can that fever however, do not lower it, the patient should go to a clinic as complications must be considered. If the acute symptoms have disappeared and the results of the urine culture are available, i. H. if you know which bacterium (germ) it is, you have to switch to an appropriate antibiotic.
Treatment is continued until the urine results are normal and no bacteria can be found in the urine culture. Check-ups and follow-up examinations after several months make sense.
In the event of non-response or repeated (recurrent) infections, a complicated pelvic inflammation should be considered (see below).
forecast
With early detection and therapy, the prognosis for primary acute renal pelvic inflammation is good. It usually heals without consequences.
Acute secondary (complicated) pelvic inflammation
causes
In contrast to the primary form, secondary renal pelvic inflammation has risk factors (see above) that can trigger or maintain inflammation. Mention should be made here of drainage disturbances or congestion in the urinary tract.
Symptoms
It is a serious clinical picture with high fever, chills such as severe flank pain. It can cause serious complications, such as abscess formation or Urosepsis (Blood poisoning), come.
diagnosis
The affected kidney is very sensitive to pain. A dry or brownish, barked tongue is noticeable. The urine itself is full of white blood cells, bacteria, and protein. Said drainage disorders are to be clarified by means of X-rays, ultrasound or urogram (see above).
therapy
This condition should always be treated in a clinic. Since the cause is usually a congestion, antibiotic therapy can do little to help, as it does not remove the cause. In the case of severe complications, it may even be necessary to remove the affected kidney (nephrectomy).
forecast
If the underlying defect is not rectified, secondary kidney pelvic infections will recur.