Plavix®
Synonyms
Clopidogrel
definition
Plavix® (clopidogrel) is used as a drug and belongs to the group of platelet aggregation inhibitors. It prevents the blood from clotting and thus prevents the formation of thrombi (Blood clots) that potentially lead to emboli (complete relocation of blood vessels), which can end in a pulmonary embolism or a stroke, for example, and is therefore life-threatening if left untreated.
Read more on the topic Clopidogrel

Mechanism of action of Plavix®
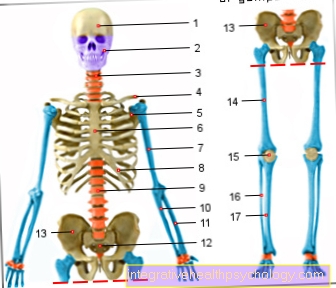
Blood clotting is roughly divided into two phases. Primary hemostasis (from the Greek hema = blood and stasis = breastfeeding) with the blood platelets (thrombocytes) as the main players and secondary hemostasis, in which 13 coagulation factors play the main role. Both run side by side and never in isolation.
Plavix® (clopidogrel) has an inhibitory effect on primary hemostasis. The platelets are in an inactive form in the undisturbed flowing blood (i.e. if there has been no injury to the surrounding tissue and no medication is taking effect). In order to go into the active form, they need various activating substances. These include thromboxane and ADP (adenosine diphosphate).
Only when such a substance has bound to the platelet does it change its shape from relatively round and uniform to spiky with many runners and thus makes the first step towards blood clotting. Because only in this prickly form are the platelets able to network with one another and - together with other substances such as fibrinogen - to form an insoluble aggregate, which is immensely important for sealing wounds after tissue damage. However, such platelet aggregation can also occur undesirably or too violently and thus harbors the risk of blood clots forming.
Plavix® (clopidogrel) prevents ADP from binding to blood platelets by blocking the ADP receptor (precise name: P2Y12 receptor). This means that the blocked blood platelets cannot be activated and the clotting process does not begin. Plavix® blocks the receptor irreversibly, so that the platelets can no longer be activated for their “entire life”.
Since platelets have a lifespan of around 10 days, clotting can only fully take place again when the blocked blood platelets have been sorted out and new ones have formed.
Basically the same principle of action also has the - mostly better known - ASA (acetylsalicylic acid), but via a different inhibition path.
Pharmacokinetics and Dynamics
Plavix® (clopidogrel) is a prodrug, which means that it is only converted into its active form in the organism (i.e. after administration). It takes 5-7 days for its full anticoagulant effect to take hold. Although its physical half-life is only 7-8 hours, its effects last much longer.
It is excreted in roughly equal proportions via the kidneys and liver (bile).
application areas
Plavix® is used for:
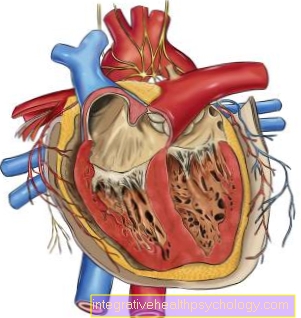
Coronary heart disease
- Coronary artery disease (CHD) - here are the blood vessels that make up the heart supply (coronary vessels) narrowed by sclerotic processes and there is a risk of developing a Blood clot (thrombus), which can be abducted and then pose a serious danger. To protect against this (preventive), anti-coagulants such as Clopidogrel.
- peripheral arterial disease (PAOD) - here - in a similar way to CHD - blood vessels are narrowed, but not in the area of the heart, but rather in the area of the lower extremities (legs). Here too, anticoagulants are used to prevent thrombosis.
- to Heart attack or stroketo keep the blood as fluid as possible and avoid another incident like this.
- in combination with ASS to Stent implantations (Stents are small tubes that are inserted into previously narrowed vessels in order to reopen them further and thus ensure adequate blood flow)
In the above-mentioned indications, however, it is usually the drug of choice ASS used. Clopidogrel is therefore mainly used in patients who are intolerant to ASA.
Side effects of Plavix®
As with all anti-clotting drugs, there is also Plavix an increased risk of bleeding, for example in the form of rather harmless Epistaxis and tendency to bruises (hematomas), but also in the form of much more critical internal bleeding e.g. in the gastrointestinal tract). It can also be under Clopidogrel the following side effects occur:
- a headache
- nausea
- dizziness
- Exhaustion
Joint pain
Joint pain is a very rare possible side effect of Plavix®. In numerical terms, this means that about 1 in 10,000 people who take the drug will experience joint pain. However, since joint pain generally occurs very often, other causes of the symptoms, such as a flu-like infection, are much more likely. If new joint pain occurs while taking Plavix and does not go away after a few days, your doctor can be asked for advice.
fatigue
One of the possible side effects listed with Plavix® is fatigue. However, it is a very nonspecific symptom that can have many causes and this drug is rarely responsible. In the event of new tiredness over a longer period of time without an identifiable cause, the family doctor can be visited so that he can get to the bottom of the cause by questioning and investigating. He will then be able to assess whether it is a possible side effect of Plavix® or another medication taken, or whether another cause is more likely.
itching
An occasional side effect of Plavix® (affecting about one in a hundred users) is itching. The symptom can appear either in isolation or as part of an allergic reaction. The latter can also manifest itself as a skin rash and the drug should then be discontinued in consultation with the treating doctor. If there is only itching, you should first wait to see whether it goes away again. However, if the itching persists and is perceived as too annoying, Plavix® may also have to be discontinued and another medication prescribed.
Do I have to stop using Plavix® before a dental procedure?
The dentist will tell you whether and when Plavix® has to be discontinued before a dental procedure such as a tooth extraction. If necessary, he will determine in consultation with the family doctor when the drug should no longer be taken. Under no circumstances should you stop taking it yourself. It is also particularly important to inform the dentist in good time if you are taking Plavix® or another blood-thinning drug. It is best to do this when the medication is ordered and not just when a dental procedure is imminent.
How much does Plavix® cost?
The price of Plavix® is usually between 100 and 300 euros for 100 tablets. However, it is a prescription drug, the costs of which are fully covered by the health insurance company if the indication is justified. The price of Plavix® is significantly higher compared to some other platelet inhibitors. However, there are also drugs with the same active ingredient from other manufacturers that are significantly cheaper (from 50 euros for 100 tablets).
What alternatives do I have to Plavix®?
In addition to Plavix®, there are other drugs that contain the active ingredient clopidogrel. With the same dosage, these can be taken equivalent as an alternative. There are also drugs from the group of platelet inhibitors that have a slightly different active ingredient, such as prasugrel. The attending physician must determine whether such drugs are an alternative to Plavix®. Taking one or two platelet inhibitors is not recommended, as these have been shown to have a protective effect on vascular occlusions and thus, for example, heart attacks and strokes if indicated.
Marcumar®
With its active ingredient phenprocoumon, Marcumar® is also a blood-thinning drug, but it intervenes in the blood coagulation cascade via a different mechanism of action. There are therefore medical indications in which Plavix® or better Marcumar® should be taken. When taking Marcumar®, the blood coagulation must be checked regularly by a family doctor with a blood test and the dose adjusted.This is not necessary with Plavix®.
Read more about the topic here: Alternatives to Marcumar®
Xarelto®
The drug Xarelto® is one of the so-called new or direct oral anticoagulants (“blood thinners”). It works by directly inhibiting an important factor in blood clotting and thus prevents the formation of clots in the blood vessels.
Plavix®, on the other hand, intervenes in the coagulation cascade by inhibiting the blood platelets. Due to the different approaches to action, the indications for the two drugs also differ. As a rule, Xarelto® is therefore not an alternative to Plavix®; instead, the doctor will decide on the right medication depending on the patient and the illness he or she has.
Similar drugs
- Ticlopidine - it uses the same mechanism of action as Plavix® (Clopidogrel), however, became severe because of the possible development of a Leukopenia (severe decrease in the number of white blood cells) as a side effect largely suppressed by its partner with fewer side effects
- Abciximab, eptifibatide, tirofiban - they also inhibit primary hemostasis, but not by the same mechanism as clopidogrel, they block another receptor (Glycoprotein IIb / IIIa) and thus prevent platelet aggregation (Networking of platelets) by fibrinogen.
- Heparin, Clexane, Coumarins - They inhibit secondary hemostasis by - in various ways - impairing the function of coagulation factors. Accordingly, they are not used as platelet aggregation inhibitors (because they do not inhibit the platelets) but called anticoagulants.
When is a Plavix® "non responder"?
If a patient who takes Plavix® regularly does not have the desired effect of inhibiting blood platelets or is only inadequate, this is referred to as a “non responder”.
The causes for this can be varied and the mechanisms for the lack of response are largely unexplained. If an event occurs while taking the medication, which Plavix® is actually supposed to prevent (for example, another heart attack), another medication should be tested if necessary.
What do I do if I forget to take Plavix®?
If you forget to take Plavix® and notice this within the next twelve hours, you should take it immediately. The next tablet is then simply taken again at the scheduled time.
However, if you only notice after more than twelve hours, you can skip this intake and only take the next tablet at the usual time. Under no circumstances should you take a double dose instead, as this would lead to an excessive inhibition of the blood platelets and increase the risk of bleeding.









.jpg)