Primary Sclerosing Cholangitis (PSC)
definition
Primary sclerosing cholangitis (PSC) is one of the so-called "autoimmune primary biliary liver diseases". In this condition, there is chronic inflammation in the small biliary tract inside and outside the liver. In the course of the inflammation leads to narrowing and thus disruption of the bile outflow. Ultimately, the primary sclerosing cholangitis leads to the destruction or regression of the small biliary tract, which in the late stage passes over to the liver tissue and a Cirrhosis of the liver caused.
.jpg)
causes
The exact causes of primary sclerosing cholangitis are currently unknown. What is noticeable, however, is a frequent association with other autoimmune diseases, especially the Crohn's disease. Since occasional familial clusters of the clinical picture are also observed, nowadays one assumes a possible one genetic factor if the primary sclerosing cholangitis develops.
Both an excessive reaction of the body's own immune system (Autoimmune reaction) on components of the biliary tract, as well individual heritable tissue characteristics so seem to play a role.
Inheritance
People with primary sclerosing cholangitis (PSC) are often concerned about the possibility of the disease being passed on to their children. To this day, however, science could no responsible genes identify or inheritance.Nevertheless, an accumulation of the otherwise rare clinical picture can be observed in some families.
Furthermore, the PSC occurs more and more in Scandinavian countries, so that heredity seems to play a role here too. Some medical studies estimate that first degree relatives, i.e. son or daughter of the person concerned, an approx. 3-5 percent risk also have primary sclerosing cholangitis. Nevertheless, this rather unlikely inheritance possibility alone should not be a reason for childlessness.
Laboratory / antibody
Various blood values, such as Antibodies can provide evidence of primary sclerosing cholangitis in the laboratory. Especially the so-called "Cholestasis parameters" can be increased. They represent disorders of the formation of bile as well as of the bile outflow. Because the little ones Biliary tubules gradually through the disease narrow and thus cause bile congestion, the cholestasis values described are increased. These include alkaline phosphatase (AP), gamma-GT and possibly liver enzymes (transaminases: GOT, GPT). In the late stage, an increase in bilirubin can also be observed in the laboratory. Due to the persistent inflammatory activity, an increased rate of sedimentation can be determined in the vast majority of patients.
Some (approx. 60-80%) of those affected also have so-called "p-ANCA" antibodies as an expression of the body's autoimmune reaction. "ANA" and "SMA" antibodies can still be non-specific, but also increased.
Symptoms
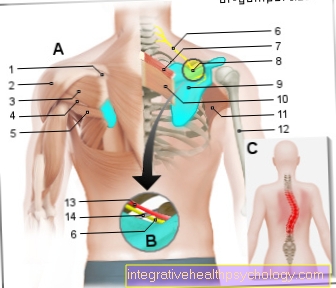
In the early stages, primary sclerosing cholangitis often has no symptoms (asymptomatic). In the context of unclear upper abdominal discomfortsuch as tenderness or nausea, those affected often go to their doctor first. Since the liver function can already be restricted, toxic breakdown products accumulate in the body. As a result, those affected suffer from severe itching (Pruritus) all over the body.
Symptoms that are felt to be particularly restrictive include tiredness, a feeling of weakness and a significant reduction in performance. When primary sclerosing cholangitis (PSC) persists, it is not uncommon for patients to complain unwanted weight loss. With acute inflammation of the biliary tract (cholangitis), fever, severe epigastric pain or chills can be observed.
In many cases the PSC is with others Autoimmune diseases (e.g. ulcerative colitis, Crohn's disease). Symptoms of these comorbidities, such as diarrhea, abdominal pain, or weight loss, can mask other symptoms.
Symptoms of liver cirrhosis appear in the later stages: jaundice, "water in the stomach" (ascites) or even liver failure.
Diagnosis / MRI
In order to clearly establish the diagnosis of primary sclerosing cholangitis, in addition to detailed questioning (anamnese) and physical examination (Jaundice Tenderness?) further diagnostic measures are taken.
In addition to blood tests in the laboratory, an ultrasound examination of the liver and gall bladder comes first. At this painless The examination creates a pictorial representation of our internal organs by means of high-frequency ultrasound waves. However, since the affected bile ducts are very small, they cannot be shown directly with an ultrasound scan. However, it is possible to discover the biliary blockage caused by primary sclerosing cholangitis without any problems!
In order to narrow down the diagnosis further, a special form of MRI examination, the MRCP respectively. During this magnetic resonance examination, patients are pushed into the tubular MRI machine for a short time. With the help of magnetic waves in specific directions, detailed images of the liver with its small biliary tract can be produced, so that the diagnosis of "primary sclerosing cholangitis" can be confirmed in the vast majority of cases.
treatment
Unfortunately, there is still no curative treatment for primary sclerosing cholangitis. Only those Liver transplant represents a final chance of recovery. In order to keep the liver values stable for as long as possible and to avoid possible infections, various medications can be used. “Urodeoxycholic acid”, or UDCS for short, has a long tradition in treatment. It has been shown to improve liver values and often lead to a decrease in the Itching and the Jaundice. Furthermore, the drug is under discussion to reduce the risk of bile duct cancer in those affected.
To prevent acute and painful inflammation of the biliary tract (cholangitis), those affected must occasionally take antibiotics.
If the biliary tract is clearly narrowed (Stenosis) the formation of gallstones is favored. In order to "widen" such constrictions again and to guarantee the flow of bile, sometimes a so-called "ERCP“Treatment done. As with a gastroscopy, a small tube with a camera is inserted through the mouth and pushed up to the bile ducts. Eventual Bottlenecks, but also smaller gallstones can be removed directly as part of the ERCP. In the meantime, the patient is asleep and, thanks to tranquilizers, feels nothing.
Cirrhosis of the liver
Cirrhosis of the liver is the end-stage of advanced liver disease. Original liver tissue is increasingly being replaced by connective tissue, so that our important organ can no longer fulfill its tasks. Liver damage that occurs in this way can occur in the most cases cannot be undone.
If left untreated, primary sclerosing cholangitis can develop into cirrhosis of the liver and cause life-threatening complications. These include Bleeding, brain disease, or kidney damage.
Colon cancer
Patients with primary sclerosing cholangitis have a significantly higher risk of developing colon cancer in the course of their lives (Colon cancer) to get sick. In comparison with the normal population, experts even name one 10 times increased likelihood. In order to detect colon cancer as early as possible, in regular intervals Colonoscopies are performed. So can precursors of cancer, so-called Polyps, usually removed during the examination. However, they occur even more frequently Bile duct carcinoma (CCC) up!
Crohn's disease
Chronic inflammatory bowel disease, such as Crohn's disease, is found in around 80% of patients with primary sclerosing cholangitis (PSC). About 80% of them suffer Ulcerative colitis and only 20% from Crohn's disease. Simultaneous presence of inflammatory bowel disease is the rule and not the exception!
Often, e.g. Crohn's disease diagnosed with the typical symptoms such as diarrhea, weight loss and abdominal pain. A few years later, patients notice new symptoms, such as fatigue or upper abdominal pain, but suspect that the intestinal disease is the trigger. Therefore, with each diagnosed Crohn's disease the typical symptoms of a PSC are queried!