Prostate cancer
What is prostate cancer?
It is a malignant growth of the prostate gland (prostate). The most common place of origin are the mucous membrane cells (epithelium), which line the ducts. Overall, prostate cancer is the most common tumor and the second most common cause of cancer-related death in men. The likelihood of developing prostate cancer increases with age. Occurrence before the age of 40 is rare.
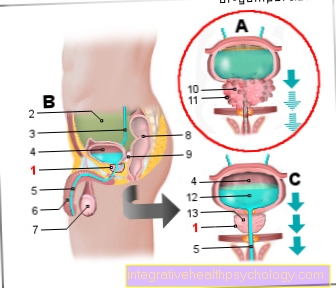
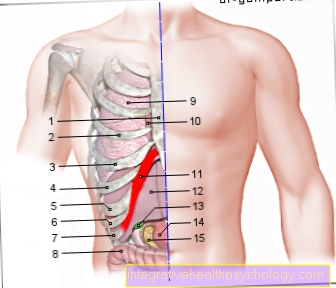
Prostate cancer (prostate cancer, PCa)
Cancer of the prostate gland
(Malignant tumor disease)
- Prostate gland - prostate
- Peritoneal cavity -
Cavitas peritonealis - Ureter - Ureter
- Urinary bladder - Vesica urinaria
- Male urethra -
Urethra masculina - Male member - penis
- Testicles - Testis
- Rectum - Rectum
- Cystic gland (seminal vesicle) -
Glandula vesiculosa - Nodular tumor tissue
- Malignant tumor
- Urine (urine) - Urina
- Glandular tissue of the prostate
You can find an overview of all Dr-Gumpert images at: medical illustrations
Which forms do you differentiate?
A distinction must be made between the following forms:
- Clinically manifest prostate carcinoma: Here the tumor can be diagnosed with the possibilities of clinical examination, especially rectal palpation.
- Incidental prostate cancer: It is found by chance in a tissue sample that was taken during the treatment of benign prostate enlargement (benign prostatic hyperplasia; BPH).
- Latent prostate cancer: More than 40% of those over 50 and 60% of those over 80 have prostate cancer, but die from other conditions without the prostate ever causing them any problems.
- Occult prostate cancer: There are no abnormal findings. The tumor is only noticeable through its daughter tumors (metastases).
Symptoms
As mentioned above, symptoms in the early stages are very rare. The reason for this lies in the location of the tumor. Most carcinomas arise in the so-called peripheral zone of the prostate, which is relatively far from the urethra. Benign prostate enlargements, on the other hand, are usually in the immediate vicinity of the urethra. Symptoms such as urinary retention therefore occur in the case of benign prostate enlargement at the beginning, in prostate cancer, however, more in the end stage.
The carcinoma is usually diagnosed as part of the preventive medical check-up or as an incidental finding during the histological examination, e.g. detected due to benign prostate enlargement.
In the late stage, the following symptoms may appear:
- Incontinence (= inability to hold back urine or stool) due to involvement of the circular muscle of the urethra and narrowing of the rectum
- Urinary retention due to the enlargement of the prostate volume, which narrows the urethra.
- Urinary stasis kidneys as a complication of urinary retention (the renal pelvis expands and kidney failure eventually occurs)
- Erectile dysfunction (= inability to get an erection) due to involvement of the blood vessels that are necessary for this
- Pain in the bones (often lumboischialgia-like) as an indication of secondary tumors (metastases) e.g. in the lumbar spine
- General symptoms of a tumor disease: unwanted weight loss, night sweats, fever
Learn more about prostate cancer symptoms.
What is the Typical Age for Prostate Cancer?
Increasing age is a risk factor for prostate cancer, therefore the probability of the disease increases with increasing age. The median age of onset for prostate cancer is 70 years.
Most men develop prostate cancer in the course of their lives, but often the disease does not become symptomatic and those affected die from other causes. The prostate cancer is then only diagnosed retrospectively. For example, in the over 80 age group, the incidence of prostate cancer is around 60%.
However, the annual check-up is recommended from the age of 45 and is covered by statutory health insurance.
How is the process?
No general statement can be made about the course of prostate cancer, as this is very individual.
In addition to the initial stage, the course depends primarily on the therapy and the general condition of the patient.
Among the cancers leading to death in men, prostate cancer was second in 2014 with 11.4% after lung cancer (24.4%) and should therefore not be underestimated. However, it is a relatively slow-growing tumor and, because of the preventive medical examinations, more and more carcinomas are being detected in the early stages.
How do you treat prostate cancer?
There are several ways to treat prostate cancer. Three factors lead to a decision:
- Tumor stage
- Age
- General condition
Specific treatment measures for locally limited tumors without metastases are surgical removal of the prostate (radical prostatovesiculectomy) and / or radiation (radiotherapy).
Hormone treatment can supplement radiation or be used independently for tumors that have already metastasized.
If distant metastases are present, hormone therapy or combined hormone chemotherapy can also be initiated.
In addition to these methods, you always have the option of treating yourself with wait and see. Since prostate carcinoma is a relatively slow-growing tumor, a low-risk finding can initially be observed with wait and see ("active surveillance"). So there is no need for immediate treatment, which avoids the side effects of the therapy options. However, there is a risk of therapy not being initiated on time.
Another concept is the controlled waiting ("watchful waiting"). This is mainly used in older patients in whom the carcinoma does not lead to a significant reduction in life expectancy (tumor-independent life expectancy <10 years). It is also used in palliative medicine when a cure is impossible.
Read more about the
- Treatment of prostate cancer
- Therapy of a prostate cancer
OP
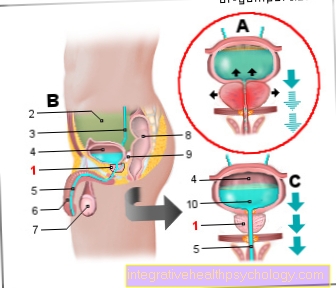
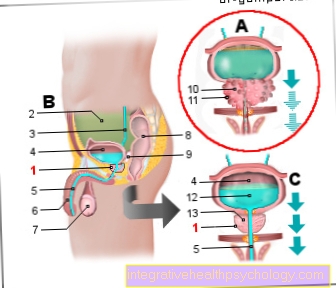
Surgical removal of the prostate (radical prostatectomy) is, in addition to radiation, the optimal procedure for non-metastatic tumors.
In addition to the prostate, the neighboring seminal vesicles and pelvic lymph nodes are removed and the vas deferens severed. The patient must therefore be aware that he will be sterile after this operation.
In addition, the operating room harbors risks.
Above all, there is stress incontinence, i.e. an involuntary loss of urine during exercise. The cause is damaged pelvic floor muscles. The degree of severity is determined based on the intensity of the exercise. In the first time after the procedure, incontinence is normal and usually straightforward. If it persists, however, you have to treat medication, surgery or conservative with pelvic floor training.
Erectile dysfunction (= inability to get an erection) occurs in 50-70% of cases. For reasons that are not yet fully understood, changes in the anatomy of the small pelvis caused by surgery or radiation can lead to this. It is believed that erectile dysfunction is a result of influencing the neurovascular bundles that supply the prostate.
Irradiation
The irradiation is equivalent to the OP as an optimal therapy.
The patient is usually irradiated daily for several weeks on an outpatient basis. The procedure only takes a few minutes and is painless. Then the patient can go home.
A distinction is made between percutaneous radiation (from the outside) and so-called brachytherapy (from the inside).
Thanks to the latest technologies, the irradiation is carried out selectively with the intention of destroying as little surrounding tissue as possible. However, this cannot be avoided entirely.
Side effects can therefore be burns, redness and inflammation of the skin. In the long term, incontinence, impotence and diarrhea can result from damage to surrounding structures.
Get more details on the advantages and disadvantages as well as the exact procedure of radiation for prostate cancer.
chemotherapy
Chemotherapy is indicated above all in an advanced stage of the disease, when the tumor has already spread to other organs. There is not much that can be achieved here with local surgery or radiation.
The patient must be aware, however, that chemotherapy only serves to extend the life span; it cannot cure the patient. In addition, this therapy places an enormous burden on the body and is therefore not suitable for every patient.
Chemotherapy is carried out in several cycles. The infusion takes about an hour to run through, after which the patient can go home.
The goal of chemotherapy is to destroy rapidly dividing cells, which include tumor cells. Other rapidly dividing cells are e.g. the cells of the lining of the digestive tract, hair root cells and blood-forming cells in the bone marrow. This can lead to vomiting, nausea, hair loss, susceptibility to infection or anemia. The patient is therefore closely monitored and medicated
Hormone therapy
With hormone therapy, the testosterone dependence of prostate cancer is made use of. Androgens are the male sex hormones that are mainly produced in the testes and one of which is testosterone. Among other things, they cause the growth and multiplication of prostate cancer cells.
In principle, hormone therapy can be used both curative (for healing) and palliative (healing is no longer possible). However, the curative approach only works in combination with other therapies such as radiation. On its own, hormone therapy cannot bring about a cure, as the tumor becomes resistant to the medication after a certain period of time and continues to grow despite low testosterone levels.
There are various substances that are either injected into the muscle or under the skin as a depot syringe, or given in tablet form. Despite different mechanisms of action, all these substances have in common that they cancel out the androgen effect. One therefore speaks of chemical castration.
The side effects of hormone therapy can be summarized under the androgen withdrawal syndrome.These include loss of libido, muscle breakdown, enlargement of the mammary gland (gynecomastia), osteoporosis, erectile dysfunction or hot flashes.
Find out more about the process, advantages and disadvantages of hormone therapy.
Immunotherapy
Immunotherapy for prostate cancer is the subject of current studies. So far, the use of immunotherapy is known primarily from the treatment of lung or skin cancer.
Cancer immunotherapies help the immune system recognize and destroy cancer cells. The immune system is not only able to fight foreign pathogens such as bacteria or viruses, but also to eliminate the body's own degenerate cells. However, this is extremely difficult in the case of cancer cells, as they have developed various camouflage mechanisms with which they can trick the immune system. At this point, immunotherapy is a good support.
Due to the exaggerated reaction of the immune system, side effects must be expected, such as chronic or acute inflammation of the intestine with diarrhea, vomiting, weight loss or fatigue, inflammation of the skin and inflammation of the liver.
What are the chances of recovery?
The chances of recovery vary depending on the stage the tumor is in. In general, when it comes to cancer, the earlier the tumor is discovered, the better the chance of recovery.
If the tumor has broken through its original organ and metastasized to other organs, healing is almost impossible. Nevertheless, it is difficult to make a statement about the remaining lifetime. Various therapies are used to keep cancer in check.
In the case of prostate cancer in particular, it should be emphasized that it is a slowly growing tumor that, thanks to regular annual preventive examinations, can often be discovered early and then completely cured.
It is therefore imperative to attend the preventive medical check-up.
Find out more about the chances of a cure for prostate cancer.
What is the life expectancy with prostate cancer?
Of course, life expectancy correlates to a certain extent with the chances of recovery.
A tumor that is recognized early and has not yet metastasized and thus can probably be cured does not in many cases mean a reduction in life expectancy.
The more advanced the stage of the tumor, the worse the chances of recovery and thus also the life expectancy.
Other important factors that affect life expectancy are:
- Age (with older age the body is less resistant)
- General condition (other diseases, nutritional status, psyche)
- Lifestyle (little physical activity, one-sided low-plant diet, alcohol abuse, etc.)
Although prostate cancer is the most common cancer in men and is the second leading cause of cancer death, it is a fairly slow growing tumor with a relatively good prognosis. In some cases, the men go unnoticed and only die years later from other causes.
A look at the 2014 data from the Center for Cancer Registry Data of the Robert Koch Institute confirms the relatively good prognosis for prostate cancer. There a relative 5-year survival rate of 91% and a relative 10-year survival rate of 90% of all prostate cancer patients are given. In comparison, only half of all patients with cancer of the mouth and throat survive the 5 years and only slightly more than a third survive the 10 years.
Get more information about prostate cancer life expectancy.
What does terminal prostate cancer look like?
While prostate cancer often does not cause any symptoms in the early stages, the end stage can manifest itself through pronounced symptoms. This is caused on the one hand by the size of the tumor and the metastases in other organs.
Often times, the tumor causes urination problems because it presses on the urethra. This leads to a weakened or interrupted urine stream, a reduced amount of urine, difficult urination and an increased urge to urinate, especially at night. Urinating can also be painful.
Erectile dysfunction can also be an indication of an advanced tumor. These include erectile dysfunction, erectile pain and decreased ejaculation.
Ultimately, the pain symptoms are particularly pronounced in the end stage. Metastases that have spread into the bones in particular cause severe back pain, movement disorders, etc.
Regardless of the cancer, the body is weakened in the end stage. The patient experiences weight loss, fever and night sweats. The most important task of the medical professional is to make the time remaining for the patient as comfortable as possible. The right pain therapy is paramount. In addition to medication, physiotherapy and occupational therapy, acupuncture or nerve stimulation methods can also help.
Read more about how end-stage prostate cancer manifests itself.
What are the causes of prostate cancer?
The exact origin is still unclear.
However, prostate cancer seems to need stimulation by male sex hormones (androgens). This can be seen from the fact that the suppression of these hormones leads to a shrinkage of the prostate and in approx. 80% of the cases also to a reduction in the size of the tumor.
Furthermore, genetic causes and environmental influences such as diet, exercise, etc. are suspected of contributing to the development of prostate cancer.
Is Prostate Cancer Hereditary?
Prostate cancer is not a hereditary disease in the classic sense, but the latest findings show that men who have developed prostate cancer in close relatives have an increased risk of developing the disease themselves.
If the father is affected by prostate cancer, the risk doubles; for a brother with prostate cancer it is up to three times higher than for men with no hereditary predisposition.
Each ...
- more family members are sick,
- and younger they were at diagnosis
- the tumor growth was more aggressive,
the higher the risk for male relatives of developing prostate cancer.
Men who have prostate cancer in their close relatives should therefore undergo the screening examination from the age of 40.
Prostate Cancer Early Detection
Unfortunately, prostate cancer rarely causes symptoms in the early stages, as it occurs on the outside of the gland (i.e. far from the urethra) and problems with urination only arise when the tumor is already very large. Since prostate cancer can only be completely cured at an early stage, participation in early detection measures ("screening") is extremely important. These include the following procedures:
- Digital rectal examination: The doctor feels with his finger over the anus for typical abnormalities of the prostate. Usually the consistency of the ball of the thumb is the same (elastic). A rough, hard knot would be suspicious.
- Transrectal sonography: It is an ultrasound examination of the prostate to assess the prostate tissue. An ultrasound probe is inserted into the intestine through the anus. The close proximity to the prostate results in a better image quality than an examination of the abdominal skin.
-
Determination of prostate specific antigen (PSA) in the blood. PSA is a protein that can be detected in the blood and is produced by the glandular cells of the prostate. An increase in can indicate prostate cancer. But there are also other causes of an increase in PSA levels.
The annual check-up is recommended for men over the age of 45 and the costs are covered by the health insurance company. In this case, however, the doctor initially only has a conversation with the patient and then carries out the digital rectal examination.
If the patient makes suspicious observations or the doctor feels changes in the prostate, an extended diagnosis is carried out, the costs of which are also borne by the health insurance in this case.
If the suspicion is confirmed in this step, a tissue sample should be taken for further clarification. If prostate cancer is diagnosed early on, there is a good chance of a cure.
Get more detailed information about the Prostate cancer screening and prostate examination.
What is the Gleason Score?
The Gleason score, together with the PSA value and the TNM classification, is used to determine the prognosis for prostate cancer. For this purpose, a biopsy (tissue removal) is examined microscopically and the stages of the cell change are determined.
To determine the Gleason score, the worst and most frequent values occurring in the tissue sample are added. The lowest degree of degeneracy is 1 and the highest 5, so in the worst case a Gleason score of 10 can occur.
A Gleason score of> 8 is an indication of a rapidly and aggressively growing carcinoma. A low value in the Gleason score, on the other hand, suggests a more favorable prognosis.
The Gleason score can also be used to make a statement about the risk of developing a relapse (recurrence of the tumor):
- low risk with Gleason score up to 6
- Medium risk with Gleason score of 7
- high risk with Gleason score from 8
In the case of palliative treatment of prostate cancer (watchful waiting), a Gleason score of up to 6 with a mortality of less than 25%, a Gleason score of 7 with 50% and a Gleason score of over 8 with a mortality rate above 75% to be expected.
What is the PSA value?
The PSA value (= prostate-specific antigen) is a cancer-unspecific value for the prostate that is measured in the blood. It is a protein that is produced by the prostate and can provide information about cellular changes in the prostate.
The PSA value is used as a tumor marker, among other things. As part of the annual prostate cancer check-up, the PSA value is determined in the event of an abnormal medical history or palpation examination. However, the results should be assessed with caution, as an increased PSA value (=> 4ng / ml) does not necessarily indicate a tumor. Conversely, in a patient with prostate cancer, the PSA value can be in the normal range.
The PSA value can also be easily manipulated, for example through mechanical stress or stress on the organ up to 48 hours before the blood is taken. These include, for example, the palpation examination at the urologist, hard stool and constipation, cycling, sexual intercourse and especially ejaculation. The value can also be increased by other influences that do not directly affect the prostate, e.g. going to the sauna or taking a hot bath before taking a blood sample.
The PSA value can be indicative for a disease, but it should definitely be supplemented by other diagnostics!
Read more on the topic: PSA level in prostate cancer
Find out about other causes of an increased PSA level and how you can lower it.
Diagnosis of prostate cancer
Most important for the diagnosis of prostate cancer are the palpation examinations and the PSA determination in the blood, which should be performed regularly as preventive examinations from the age of 45.
If the above-mentioned examinations give rise to suspicion, tissue should be removed in the form of a so-called punch biopsy. Six to twelve samples are taken from different areas of the prostate. The procedure takes place through the rectum and is painless due to the speed of the procedure. Secondary bleeding is possible, so blood-thinning medication (e.g. aspirin) should be discontinued beforehand in consultation with the attending physician.
The following examinations are necessary for the exact size estimation of a possibly existing tumor:
- digital - rectal examination (palpation)
- transrectal ultrasound
- PSA - concentration in the blood
For further therapy planning, a CT (computer tomography) or MRI of the prostate (magnetic resonance tomography) may be necessary.
The MRI of the prostate has come more and more into focus in recent years, as specially trained radiologists can now make good statements about the location and spread of the tumor. Samples can now also be taken under the MRI of the prostate.
Read more about MRI of the prostate.
In order to discover secondary tumors (metastases), a scintigraphy of the skeleton is necessary, since the first distant metastases are usually to be found there (especially in the pelvic bones and the lumbar spine).
Learn more about Metastases in prostate cancer.
If the PSA value is lower than 10 ng / ml, metastases are highly unlikely and a skeletal scintigraphy should therefore not be performed.
In the subsequent microscopic examination of the removed tissue, the pathologist can determine the degree of malignancy (degree of malignancy) using existing tables (Gleason score, classification according to Dhom).
Here is the main article Prostate biopsy.
TNM classification
The TNM classification describes prostate cancer in terms of the local tumor itself (primary tumor), abbreviated with (T), as well as the presence of lymph node metastases (N) or distant metastases (M). The disease stages determined here have a direct impact on therapy planning and the prognosis for the patient (healing / survival rate)
- T1: incidental carcinoma (not palpable or visible), d. H. discovered by chance during a biopsy
- T1a - <5% of the tissue removed as part of a scraping of the prostate in BPH (benign prostate enlargement)
- T1b -> 5% of the removed tissue as part of a scraping of the prostate in BPH (benign prostate enlargement)
- T1c - larger tumor detected by stem biopsy (e.g. with elevated PSA)
- T2: tumor limited to prostate
- T2a - less than half of a lobe involved
- T2b - more than half of a lobe affected
- T2c- Both prostate lobes are involved
- T3: tumor exceeds the prostate
- T3a - prostate capsule is exceeded
- T3b - tumor affects the seminal vesicles
- T4: tumor affects neighboring organs (bladder neck, sphincter muscle, rectum, etc.)
- N + / N-: Lymph node involvement in the pelvis yes / no
- M0 / 1: Distant metastases no / yes
Read, Which It stages prostate cancer gives.