Psychosomatics
definition
In the Psychosomatics it is a special field of psychiatry.
In psychosomatics, the main thing is to pay attention to the physical (somatic) illnesses and the mental problems (psyche) of the patient and to see whether these are related to one another. Psychosomatics thus combines the mental health of the patient with the physical reactions.
For example, a patient may suddenly have severe abdominal pain as a result of a stressful event. This pain occurs even though the patient has no organic disease or infection. Still, the pain is real. In this case, they were triggered by the psychologically stressful event.

What is psychosomatics?
Psychosomatics is a special field of psychiatry. In order to understand what psychosomatics is, it helps to translate the term into German. The psyche stands for the soul, soma means body. Psychosomatics is a specialty that deals with the physical and mental well-being of the patient and tries to treat both in harmony. The main concern here is that the patient's physical problems are treated, even if no organic cause can be found.
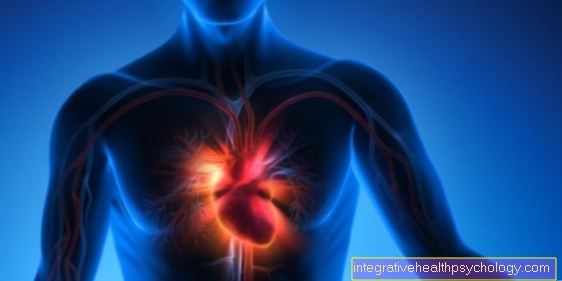
What psychosomatics is and what diseases it deals with can best be discussed using a few examples. For example, psychosomatic medicine deals with patients who suffer from an addictive disease. The addiction can lead to physical illnesses, such as rapid heartbeat (tachycardia), increased sweating or liver disorders. However, the addiction itself can be traced back to a psychological or emotional problem, for example depression.
In psychosomatic treatment, the doctor will initially help the patient to treat the drug problem and the underlying mental illness (such as depression). Treatment of the mental illness often leads to an improvement in the physical symptoms. Thus the physical illness (for example tachycardia) was also treated by stabilizing the patient psychologically.With the help of this example you can clearly understand what psychosomatics is and that this specialty has the whole person in view in order to treat him holistically. In addition to addictions, there are other diseases that are treated in psychosomatics. These include eating disorders such as anorexia, mental disorders that lead to physical symptoms (e.g. panic attacks), post-traumatic stress disorders and many more.
Take the test here: Am I suffering from depression?
Who treats psychosomatic complaints
Psychosomatic complaints are treated by Specialists in psychiatry, of so-called Psychiatrists. In addition, however, psychologists can also General practitioners treat a psychosomatic illness.
Patients often turn to their family doctor, especially at the beginning of the diagnosis. This can often help the patient to a certain extent. In more severe cases, however, it is absolutely necessary that a patient with psychosomatic complaints is treated by a psychiatrist or a psychologist.
Treatment can be either outpatient or inpatient. This means that the patient either repeatedly comes to the practice of the psychologist or psychiatrist (outpatient) or that he is treated in a special ward for psychosomatics in the hospital.
In some cases so-called Rehabilitation centers (REHA for short), where the patient stays for a few weeks. In such centers, various group therapies as well as individual treatments with a psychologist or psychiatrist are offered. This treatment concept can be particularly useful for patients with eating disorders or addictions. The patient also meets in such facilities Occupational therapists, physiotherapists and other assistants who also do a small part of the psychosomatic treatment. However, those who mainly treat psychosomatic complaints are psychiatrists.
The psychosomatic clinic
The psychosomatic clinic is part of one psychiatric clinic. Depending on the range of treatments at the clinic, this is one inpatient clinic, in which the patients are completely housed for several days to weeks or around one outpatient clinic. In this, the patients can go home in between. You either come to the psychosomatic clinic only at agreed appointments or every day, but spend the night at home (so-called day clinic).
Every psychosomatic clinic is structured somewhat differently and geared towards different patient groups. For example, there are special clinics that only focus on eating disorder specialize. Other clinics, on the other hand, deal exclusively with addiction.
Take the test here: Do I have an eating disorder?
Often psychosomatic clinics and rehabilitation centers are put on an equal footing, although it is often difficult to make a precise distinction. In general, acutely ill patients should go to a psychosomatic clinic, whereas a rehabilitation facility is more suitable for patients who are no longer acutely ill. Often, however, the transition is so fluid that hardly any differences can be made between the two institutions, especially when it comes to addictions or eating disorders. On the other hand, depression or post-traumatic stress disorders should best be treated in a psychosomatic clinic, as the opportunity to talk to a doctor is often more frequent because the doctors often visit the patient every morning.
Psychosomatic pain
Psychosomatic pain is pain that is real to the patient, but has no organic or physical cause.
Usually, pain has an indispensable protective function to warn people that they shouldn't do certain things anymore. For example, touching a hot stove top causes tremendous pain. This is a good thing, because otherwise you would touch the hot stove again and again and get burned.
Nevertheless, there is also pain that does not have a protective function and is therefore only stressful for the patient. This includes psychosomatic pain. In general, studies have shown that patients deal with pain differently. If a patient is particularly afraid of any pain, he will often feel the pain much more intense and worse than a patient who is not afraid of the pain. These different types of pain sensation seem to have something to do with the patient's attitudes and expectations. Since the pain is aggravated by fear or panic, it is called psychosomatic pain.
Often this is acute pain. However, psychosomatic pain can be chronic. For example, depression can lead to chronic back pain.
There is also a disease called hypochondria. This is the patient's belief that they are sick. Patients who suffer from hypochondria deal very intensively with their disease. In some cases this can go so far that the patient imagines the psychosomatic pain without it actually existing.
- Can you imagine pain?
- Persistent somatoform pain
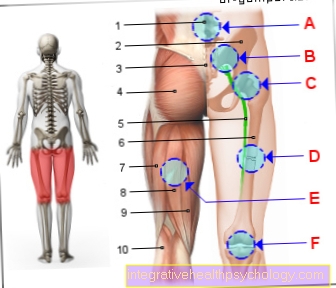
Psychosomatic back pain
Many patients now suffer from back pain. These can have various causes. The back pain is often due to the fact that many people have to sit for a long time (for example at work) and do too little sport to compensate.
However, there are also cases in which back pain is psychosomatic. Psychosomatic back pain is pain that has no recognizable physical cause. This means that neither a herniated disc nor the tense muscles are responsible for the patient suffering from back pain.
The cause here is an emotional or psychological problem that the patient has not yet solved. Mental health problems can manifest themselves through various physical symptoms. Among other things, it can lead to psychosomatic back pain. Here, the patient suffers from severe back pain, especially in stressful situations, without this pain being due to an acute physical event.
Psychosomatic back pain is particularly common in depressed patients. It is important here that the patient takes into account that the pain can also come from the fact that the patient is not moving enough due to his depression but is more likely to sit or lie down. This can lead to muscular tension, which is then not psychological, but is caused by poor posture of the body.
Furthermore, the tremendous fear of back pain can lead to the patient adopting a relieving posture, which then leads to nerve entrapment and muscle tension. An anxiety disorder can also lead to back pain and it is often difficult to differentiate where this pain is coming from. On the one hand, the pain can be triggered by fear alone, on the other hand, it can also be caused by a wrong relieving posture.
Psychosomatic back pain is therefore a so-called exclusion diagnosis. This means that the doctor first checks whether the back pain is not coming from the intervertebral disc, from nerve entrapment, from muscular tension or something similar. If no physical problems could be determined, but the patient suffers from mental problems, the diagnosis of psychosomatic back pain is made.
These articles might also interest you:
- Psychosomatic back pain
- Chronic back pain therapy - what works best?
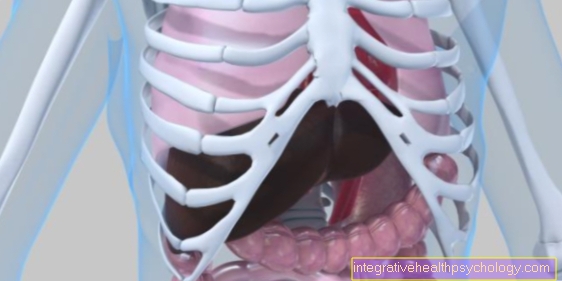
Psychosomatic diarrhea
The gastrointestinal tract (gastrointestinal tract) reacts particularly sensitively to mental problems of the patient. If a patient suffers from severe stress, part of the so-called autonomic nervous system is activated particularly strongly. This part of the autonomic nervous system is called the sympathetic nervous system. This ensures that the gastrointestinal tract becomes active and digests food faster.
In stressful situations, this can lead to patients suffering from diarrhea more quickly. Since this diarrhea has no organic cause, such as eating rotten food, it is called psychosomatic diarrhea. If a patient suffers particularly frequently from psychosomatic diarrhea, it may be that irritable bowel syndrome is to blame.
In general, however, psychosomatic diarrhea cannot only occur in stressful situations. Depression, anxiety disorders or post-traumatic stress disorders can also lead to impaired digestion.
It is important to differentiate between organically caused diarrhea and psychosomatic diarrhea. If blood deposits or mucus are added to the diarrhea or if the patient has the feeling that he can no longer keep any food with him, he should urgently go to a hospital and not dismiss the symptoms as psychosomatic.
In general, it is also very important to keep the exact definition of diarrhea in mind. Diarrhea is defined by the fact that the patient has to go to the toilet more than 3 times a day and that the stool is very fluid. Psychosomatic diarrhea, on the other hand, is often accompanied by an increased stool frequency, but usually only 2-3 times a day and only for a short period of time. As long as the patient pays attention to a balanced diet and sufficient fluid intake and the stool does not become bloody or persists, the patient usually has nothing to fear.
Nevertheless, the basic problem, i.e. the depression or the anxiety disorder, should be treated, otherwise the diarrhea cannot get better and will occur again and again in situations with increased stress.
Psychosomatic cough
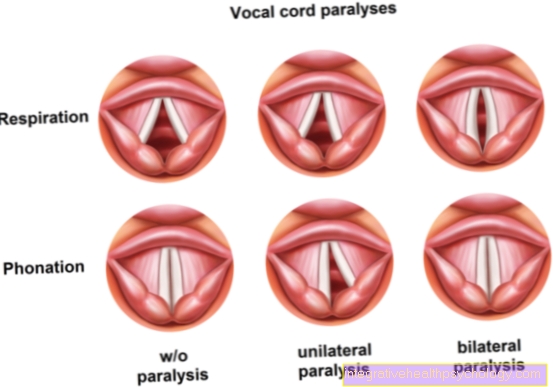
When one speaks of a psychosomatic cough, it is a psychogenic cough. In addition to the cough, patients often suffer from one too Tightness in the chest area, a burning sensation or pain that increases or is constant when you inhale.
Since the symptoms hardly differ from those of a classic cold, a discussion between the doctor and the patient, in which the patient describes his problems in detail, is of crucial importance. An acutely stressful event in the patient's life is often related to the sudden onset of a psychosomatic cough. In addition to acutely stressful events, it can also occur in a depression or at one Anxiety disorder develop a psychosomatic cough.
At Children it can occur after prolonged lung disease (for example whooping cough) In addition, they continue to cough for a long time after the disease has already been overcome. The reason for this is a so-called conditioning. For example, they have learned that every time they cough, they receive attention. This can cause the children to continue coughing long after the disease has passed. However, this psychosomatic cough usually disappears on its own after a few days, so psychotherapy is not necessary.
In rare cases a so-called Tic disorder lead to a psychosomatic cough. Here, the patient has the inner urge to cough immediately, without there being any physical cause. Tic disorders usually begin in childhood, but can also only manifest in adulthood.
Psychosomatic cough can usually be treated very well with the help of psychotherapy. However, the longer the patient suffers from the symptoms, the worse the prognosis. It is therefore advisable to see a psychotherapist as early as possible.
Psychosomatic bubble
A psychosomatic bubble is either an existing one Incontinence due to mental illness or a bladder disorder in which the urge to urinate is increased and the patient has symptoms similar to those of a cystitis.
Especially in the case of smaller children, although they have actually not been wetting the bed for years, they can suddenly go back to bed during acutely stressful events. This psychosomatic bladder disorder is also known as wetting and is to be understood as a warning. For example, it may be that the child is acutely overwhelmed at school and therefore develops great fear. This can cause the child to go back to bed at night. In adults it can also be caused by depression or anxiety disorders Wetting come, although these psychosomatic bladder disorders are more likely to occur in children.
In adults there is a so-called Irritable bladder. The patient has to go to the toilet extremely often and has a constant need to urinate. An irritable bladder can have many different causes, including one Prostate enlargement in men, but it can also be psychosomatic. The patient is often extremely afraid of possibly getting wet and therefore has to constantly go to the toilet. This psychosomatic bladder disorder occurs mainly in older people, with women and depressed patients being particularly affected.
In order to avoid a vicious cycle, the affected patients should seek professional help in the form of psychotherapy as early as possible. In dementia patients, too, there are often psychosomatic bladder disorders, in which the patients often wet themselves. Therapy is often difficult here and the symptoms can only be improved by wearing diapers