Osteoarthritis of the shoulder
introduction
Osteoarthritis of the shoulder (Omarthrosis) is one of the shoulder diseases caused by wear and tear. Shoulder arthrosis is characterized by cartilage consumption in the main shoulder joint. In contrast to knee osteoarthritis and hip osteoarthritis, it occurs much less frequently. The reason for this is that the shoulder is not a weight-bearing joint. Your cartilaginous joint surfaces are not subjected to the same loads as on the knee joint or hip joint.

What are the symptoms of shoulder osteoarthritis?
The symptoms of shoulder osteoarthritis usually begin with shoulder pain after prolonged exposure to the arm. The pain from fatigue in the shoulder joint continues to increase and can also radiate into the rest of the arm. In addition, shoulder osteoarthritis can lead to increased pain when starting to move. These are caused by the fact that not enough synovial fluid has yet formed in the joint space, i.e. between the bones that form the joint. The synovial fluid is responsible for ensuring that the bones gently slide past each other when they move and do not rub against each other and thus wear out. It also supplies bones and cartilage with nutrients that are important for maintaining and rebuilding them.
At the beginning of a movement, the formation of synovial fluid is activated. Therefore, there is little synovial fluid between the bones at the beginning. If these have already been damaged by the osteoarthritis, rubbing against each other is very painful and can last for the entire duration of the movement, which is why it is referred to as permanent pain.
As the disease progresses, the pain becomes more and more persistent and can also occur at rest and at night. In addition, pronounced osteoarthritis is usually associated with restricted mobility. The cause of osteoarthritis is wear and tear and not inflammation.
Nevertheless, an existing shoulder osteoarthritis can become inflamed. This is called activated osteoarthritis. In addition to the pain, symptoms such as redness, swelling and warming of the shoulder joint occur here.
Read more on the topic: Symptoms of shoulder osteoarthritis
Pain
Pain is the most common symptom of shoulder osteoarthritis. The pain is most pronounced at the beginning and at the end of a load. They can occur not only in the shoulder itself, but also in the lower areas of the arm. The pain is particularly bad during movements such as splaying the arm or rotating, as the bones are pressed together particularly hard.
Appointment with a shoulder specialist

I would be happy to advise you!
Who am I?
My name is Carmen Heinz. I am a specialist in orthopedics and trauma surgery in the specialist team of .
The shoulder joint is one of the most complicated joints in the human body.
The treatment of the shoulder (rotator cuff, impingement syndrome, calcified shoulder (tendinosis calcarea, biceps tendon, etc.) therefore requires a lot of experience.
I treat a wide variety of shoulder diseases in a conservative way.
The aim of any therapy is treatment with full recovery without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
You can find more information about myself at Carmen Heinz.
Restriction of movement
Restriction of movement is a symptom of advanced shoulder osteoarthritis. In the joint, the adjacent bone surfaces are surrounded by a protective layer of cartilage. This cartilage layer is destroyed more and more in osteoarthritis, which increases the pressure on the bone. This causes the bone below the cartilage to thicken to keep it stable. The increased bone formation, however, leads to stiffening and restricted mobility. These become particularly evident when rotating the shoulder joint and spreading the arm outwards.
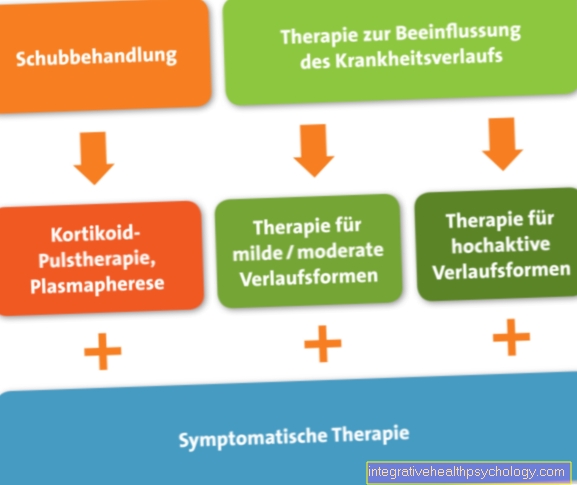
How is shoulder osteoarthritis treated?
As is so often the case, the therapy of shoulder osteoarthritis is differentiated into conservative and the operative part. Basically, conservative measures are preferable to operational ones.
Conservative therapy
By conservative (not operational) Measures cannot cure shoulder arthrosis. All related treatment measures aim at:
- a pain relief
- taining and improving joint mobility and
- Muscle strengthening
from. The aim is to maintain the function of the shoulder and to minimize the progression of shoulder arthrosis. Therapy options include:
- Painkiller (Analgesics)
- Non-steroidal anti-rheumatics (NSAIDs) - for pain therapy in particular inflammatory disease phase (e.g. diclofenac, ibuprofen, arcoxia)
- Cortisone - injected into the joint (intra-articular) or under the roof of the shoulder (subacromial) for strong anti-inflammatory properties
- Hyaluronic acid - Hyaluronic acids belong to the group of so-called chondroprotectives.
- Hyaluronic acid is a natural component of cartilage that is lost in osteoarthritis. If you inject hyaluronic acid directly into a joint damaged by osteoarthritis, the quality of the remaining cartilage improves, which has a positive effect on pain and mobility.
- Physiotherapy - to maintain joint mobility and muscle strengthening (active and passive movement exercises, stretching, manual therapy, isometric muscle building and much more)
- Physical therapies - cooling, pain relieving current applications, iontophoresis
- X-ray stimulation
What drugs help with treatment?
Pain medication can help in particular with shoulder osteoarthritis. It is very important to slowly increase the dosage of the medication and to start with lighter pain medication. In this way, if the pain increases, you have the option of increasing the dose and not exhausting the maximum dose at the beginning of the therapy.
In addition, permanent pain therapy should be avoided due to the strong side effects. For acute symptoms, drugs such as paracetamol, ibuprofen or diclofenac are started.
The latter two have the advantage that, in addition to relieving pain, they also have an anti-inflammatory effect and thus prevent inflammation of the affected joint. Diclofenac can also be applied directly to the affected area in the form of a cream known under the name Voltaren®. It moves into the relevant area and is particularly effective there. This can reduce side effects in other parts of the body. If these drugs are no longer sufficient, stronger pain relievers such as tramadol, which belongs to the group of opiates, are also used.
Operative therapy
The shoulder joint cleaning (Debridement) in the context of a shoulder joint specimen (arthroscopy) and possibly the simultaneous removal of the epidermal bursa can only achieve a certain degree of relief temporarily.
The gold standard (recommended therapy) in the surgical treatment of severe shoulder osteoarthritis is the endoprosthetic joint replacement (shoulder prosthesis).
The worn joint parts of the humerus head and the flat shoulder (Glenoid) replaced by artificial materials. In the last 20-30 years there has been great progress in shoulder prosthesis development. Modern shoulder prostheses can handle the complicated, individually varying anatomy (construction) emulate the shoulder, so that the surgeon has almost all options open to select the optimal prosthesis for the patient.
Permanent shoulder joint stiffening (Arthrodesis) and the replacement shoulder joint removal (Resection arthroplasty) are reserved for particularly complicated cases, for example after a failed joint replacement or bacterial infection (both very rare).
Read more on the topic: Surgery for shoulder osteoarthritis
Which exercises can help?
A few exercises can help with shoulder osteoarthritis. It should be noted that the joint must always be well prepared and warmed up before loading.This allows sufficient synovial fluid to form and further wear and tear on the cartilage is prevented.
The muscle groups of the shoulders, the back and the upper arm should be stressed in a targeted and careful manner, with as little as possible and, if at all, light weights being used at the beginning.
In the beginning, exercises such as pulling apart a terraband, circling, or raising and lowering your shoulders can help. Furthermore, exercises can be carried out in the four-footed position, in which the arms are alternately lifted and the shoulder is loaded and relieved.
Further exercises are, for example, push-ups against the wall, spreading your arms with very light weights or bringing your arms together behind your back, like tying an apron. For all exercises, it is advisable to learn them in the presence of a physiotherapist or a trained fitness trainer in order to prevent poor posture, which can worsen shoulder arthrosis.
In addition, it is important to note that with an activated shoulder arthrosis, i.e. an existing inflammation that manifests itself in the form of redness, swelling and warming, no exercises may be performed. The joint should be immobilized, cooled, and elevated.
Which sports are good for shoulder osteoarthritis?
For shoulder osteoarthritis, sports that involve slow, targeted movements of the joint and build up the muscles of the shoulder are particularly suitable. This includes, for example, fitness training with or without equipment.
Nordic walking with sticks can also be recommended, as the arms are specifically and carefully used here. In general, other endurance sports are also good for shoulder osteoarthritis. When carried out regularly, they lead to weight loss, which relieves all joints and thus has a positive effect on shoulder arthrosis. Swimming is also a very recommendable sport as it is very easy on the joints.
What degree of disability do you get for shoulder osteoarthritis?
In the case of shoulder osteoarthritis, the degree of disability depends on the degree of restricted mobility and stiffness. The mobility of the shoulder girdle is also crucial. If the arm can only be raised by 120 degrees and the ability to rotate and spread is restricted, there is a GdB / MdE degree of 10. In the case of severe restrictions, the GdB / MdE degree can be up to 50.
Cause and development of shoulder arthrosis
Known causes of shoulder arthrosis are mechanical overloads, damage to the rotator cuff (muscle and tendon sheaths that move and stabilize the shoulder joint), conditions after operations, inflammation and accidents. In most patients who suffer from shoulder osteoarthritis, however, the cause remains unclear. In these cases, one speaks of primary shoulder arthrosis or primary omarthrosis.
The complaints are rather uncharacteristic and manifest themselves in shoulder pain and restricted movement of the shoulder. The diagnosis is made by x-rays of the shoulder. Both conservative and surgical treatment methods (shoulder prosthesis) can be considered
Damage to the rotator cuff as causes of shoulder arthrosis
The rotator cuff describes several shoulder-encompassing muscles and tendons that move the shoulder joint and keep it in an optimal position for joint function. Defects of the rotator cuff lead to a muscular imbalance and loss of the stabilizing balance. The supraspinatus muscle under the roof of the shoulder is most frequently affected by injuries, most of which are caused by degeneration (wear) are caused, less often by an accident.
If the supraspinatus tendon is torn as the cause of shoulder arthrosis, the mechanics of the shoulder joint are severely disturbed. In the extreme case of a complete tear, the humerus head leaves its original position in the joint and rises up under the roof of the shoulder. This leads to incorrect loading of the shoulder joint cartilage, which leads to increased cartilage wear and ultimately to shoulder joint arthrosis. The final stage of this development is described by the term defect arthropathy, in which the head of the humerus comes into contact with the roof of the shoulder (Acromion) is coming.
The frequency peak of wear-related rotator cuff injuries is in the 4th and 5th decades of life.
Operations on the shoulder joint as causes of shoulder arthrosis
Operations on the shoulder can cause shoulder arthrosis if the shoulder balance is disturbed. The most important example here are operations to stabilize the anterior shoulder after shoulder joint dislocation (shoulder dislocation). The mostly necessary re-fixation of the joint lip (Labrum) and above all The gathering of the anterior shoulder capsule can lead to the humerus head being pushed backwards if the shoulder joint capsule is too shortened. As in the previous example, there is a disorder of the shoulder joint mechanics. In this case, the acetabular cartilage is overloaded (Glenoid) in the rear shoulder area.
Accidents as causes of shoulder osteoarthritis
Injuries to the joint-forming shoulder blade (e.g. Dislocation fractures of the glenoid with dislocations of the shoulder) or the head of the humerus can lead to irregularities in the cartilage surfaces or to joint misalignments. In both cases there is increased cartilage wear, which gradually develops into shoulder osteoarthritis.
Inflammation as a cause of shoulder osteoarthritis
Bacterial inflammation of the shoulder is rare and comes either through the spread of germs via the bloodstream (very rare) or caused by medical treatment measures (iatrogenic), e.g. after operations or injections. The shoulder joint can quickly be seriously damaged by the bacteria themselves and by the cartilage-damaging substances they produce.
The most common form of non-bacterial shoulder joint inflammation is chronic polyarthritis ("joint rheumatism"). The chronically inflamed synovial membrane proliferates into the joint cartilage and progressively destroys it.
The rare death of the humerus head due to loss of blood flow to the bone also leads to shoulder arthrosis when the cartilage-bearing part of the humerus head collapses.
Diagnosis of shoulder osteoarthritis
To diagnose shoulder osteoarthritis (Omarthrosis) you need x-ray images in 2 planes (a.-p. and axial). For anatomical reasons, the beam path of the X-ray tube must be positioned 30 ° outwards in order to just hit the shoulder joint gap. This is important in order to be able to recognize a narrowing of the joint space in the initial stage as a relatively early sign of osteoarthritis. Earlier than on the AP image (shoulder view from the front), the incipient narrowing of the joint space can be seen in the axial image (shoulder view from above with the arm raised to the side.)
In advanced cases, the typical radiological changes of osteoarthritis (joint wear) become apparent, which do not differ from other joints (e.g. knee osteoarthritis, hip osteoarthritis).
There is an increased white markings on the joint surfaces of the humerus head and shoulder joint portion (subchondral sclerotherapy) as an indication of bone overload in this area, as the cartilage buffer is no longer sufficiently available.
Bone attachments follow later (Osteophytes) on the humeral head and shoulder socket (glenoid). In the final stage, deformation (deformation) of the humeral head, which loses its spherical structure. At some point, the joint space can no longer be delimited if there is a complete loss of cartilage. If the rotator cuff is seriously damaged at the same time, the head of the humerus can slide upwards under the roof of the shoulder (Defect arthropathy), which can be seen well on the X-ray (eccentric omarthrosis).
With an ultrasound (Sonography) of the shoulder, shoulder arthrosis cannot be diagnosed. Sonography is important in the representation of the soft tissues (muscles, tendons, ligaments). It is of particular importance as a reliable diagnostic tool for the detection of rotator cuff defects (rotator cuff tear). Recognizing them is decisive for the further design of therapy.
In addition to osteoarthritis of the shoulder joint, there is usually further damage to the structures of the shoulder, especially the rotator cuff. For this purpose, diagnostics with the MRI of the shoulder joint has proven itself. When planning a shoulder prosthesis, the CT of the shoulder joint is more important.
You can find out more under our topic: MRI scan of the shoulder joint
frequency
Shoulder diseases caused by wear and tear are common. Diseases of the muscle and tendon structures of the shoulder joint (shoulder roof) are more common than shoulder arthrosis. The diseases of the rotator cuff tear, calcified shoulder (tendinosis calcarea) and the impingement syndrome should be mentioned in particular. Studies have shown that the frequency (prevalence) of shoulder complaints can be 8% and more. Changes in the main shoulder joint (glenohumeral joint) caused by wear and tear occur in around 30% of people.
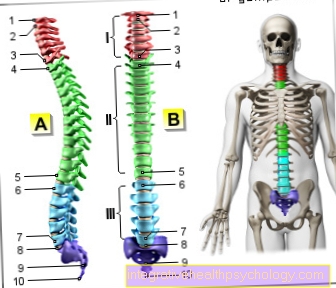
Anatomy of the shoulder
The shoulder joint (Glenohumeral joint) becomes from the humerus head (Humeral head) and the shoulder socket (Glenoid) of the shoulder blade (Scapula) educated. The head of the humerus has a joint surface 6 times larger than the corresponding surface of the joint socket.
The enormous range of motion of the shoulder joint that can be achieved in this way is only possible through the small bony joint guidance. In most other joints, the bony guidance is much stronger (e.g. hip joint). This lack of stability is compensated for by a complex muscle, tendon and ligament system. The precise interaction and the delicate balance of the muscles involved (especially the rotator cuff) ensure that the humerus head is correctly in contact with the shoulder joint socket in every arm position.

- Humerus head - Caput humeri
- Shoulder joint socket -
Glenoid Cavitas - Shoulder blade - Scapula
- Collarbone - Clavicle
- Shoulder corner - Acromion
- Shoulder-collarbone
Joint -
Articulatio acromioclavicularis - Deltoid - M. deltoideus
- Raven beak process -
Coracoid process - Raven beak extension shoulder corner
Tape -
Coracoacromiale ligament - Joint cavity -
C.avitas articularis - Fiber cartilage ring -
Glenoid labrum - Biceps, long head -
M. biceps brachii - Bursa -
Subacromial bursa - Upper arm shaft -
Corpus humeri
You can find an overview of all Dr-Gumpert images at: medical illustrations
Anatomy of the shoulder

- Humerus head
- Shoulder height (acromion)
- Shoulder joint
- Collarbone (clavicle)
- Raven bill process (Coracoid)
- Shoulder joint (glenohumeral joint)

.jpg)


















.jpg)





