Shoulder dislocation
definition
A shoulder dislocation (also shoulder dislocation or shoulder dislocation) is a usually very painful displacement of the shoulder joint.
The shoulder joint consists of the socket of the shoulder blade (Scapula) and the head of the humerus (Humerus), which only lie very loosely on top of each other in order to allow maximum mobility and rotation. The joint is held primarily by a device made of ligaments and muscles.

If there is a large external force, it can give way to the pressure and the head of the humerus is displaced. Then it loses contact with the shoulder blade and normal movement of the shoulder is no longer possible. A shoulder dislocation should always be corrected by a specialist
One can distinguish shoulder dislocations in terms of their mechanism of origin. So there are:
- Traumatic shoulder dislocation as a result of a direct accident
- One speaks of a post-traumatic recurrent dislocation when, after a primarily purely traumatic shoulder dislocation, recurring dislocations occur even with minor trauma
- Atraumatic shoulder dislocation, also called habitual shoulder dislocation. Here, the shoulder joint pops out repeatedly without any trauma, for example when performing habitual movements. The causes for the development of habitual shoulder dislocations are genetic. Congenital acetabular dysplasias or congenital slack ligaments, etc. can be cited as an example of this.
Treatment of a shoulder dislocation
Appointment with a shoulder specialist

I would be happy to advise you!
Who am I?
My name is Carmen Heinz. I am a specialist in orthopedics and trauma surgery in the specialist team of .
The shoulder joint is one of the most complicated joints in the human body.
The treatment of the shoulder (rotator cuff, impingement syndrome, calcified shoulder (tendinosis calcarea, biceps tendon, etc.) therefore requires a lot of experience.
I treat a wide variety of shoulder diseases in a conservative way.
The aim of any therapy is treatment with full recovery without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
You can find more information about myself at Carmen Heinz.
Conservative therapy - reduction of the shoulder
A shoulder dislocation is always a hospital case. In no case should you try to ball the shoulder back in yourself, as this could damage surrounding structures.
Conservative therapy for shoulder dislocation does not require surgery on the shoulder. Depending on the extent of the injury that accompanies the dislocation of the shoulder, conservative therapy is sufficient to treat the shoulder and achieve a very good result.
Basically, the shoulder must first be adjusted. Avoid jerky movements. It is also important to talk to the patient and explain the work steps to him in order to take away any fear. As a rule, the patient has brief pain when straightening. A subsequent freedom from pain is a sign of a successful reduction.
- In the Hippocratic reduction, the patient lies on his back, the doctor puts his heel in the armpit of the patient and pulls on his arm. The doctor's foot pushes the patient's upper arm head outwards, whereupon the patient slides back into the socket.
- The reduction according to Arlt, however, is carried out while sitting. Here the patient's arm is placed over a chair back padded with a cushion. Then the doctor pulls on the patient's arm, whereupon the back of the chair is supposed to push the head of the humerus upwards, which also slides back into the socket.
Before performing any of these procedures, the patient must always be given pain relievers and possibly muscle relaxants.
Read more about this topic under: Therapy of shoulder dislocation
Risks when straightening the shoulder
The adjustment of a dislocated shoulder must be carried out by qualified personnel, as people without the necessary experience can harm the patient. On the one hand, there is a misconception that adjusting should be carried out using rough force and jerky movements. But this is not the case at all, as this increases the risk of injuring blood vessels and nerves. On the other hand, it inflicts avoidable pain on the patient. After the arm has been repositioned and immobilized for several days, intensive physiotherapeutic treatment is necessary. This can accelerate the healing of the soft tissue damage caused by the dislocation and counteract a stiffening of the shoulder joint.
When do you need an operation?
An operation makes sense in two constellations. If nerves, vessels, ligaments or bones etc. have been damaged by a rough application of force, an operation is recommended to treat any damage. In the case of a conservative reduction, fractures or vascular tears would be left untreated. The other need for surgery is for recurrent dislocations. Frequent dislocations destabilize the shoulder joint, which is why the risk of further dislocations increases steadily. The operation restores stability to the joint.
- Course of the operation
With the advancement of medicine, one can now operate the shoulder with the smallest of operations. In a so-called arthroscopic procedure, the shoulder is provided with three millimeter-sized holes through which a mini camera and special instruments are guided. The injured structures can then be restored using these utensils. Splintered bone parts are placed in their original position and stretched ligaments are tightened to prevent renewed dislocation.
If a shoulder dislocation has to be operated on, a jointoscopy is usually the first step (Arthroscopy) carried out. In this minimally invasive surgical method, the shoulder is provided with three millimeter-sized holes through which a mini camera and special instruments are guided. The injured structures can then be restored using these utensils. Splintered bone parts are placed in their original position and stretched ligaments are tightened to prevent renewed dislocation. In this way, any damage that may have occurred in the joint during the dislocation can be assessed. Depending on how severe the damage to the joint is, different surgical methods are used. Recently, the minimally invasive method of performing shoulder dislocation surgery has become increasingly popular. When the shoulder is dislocated, the ligaments of the shoulder joint and the joint capsule are often damaged. The attending surgeon fixes the ligamentous apparatus back on the edge of the joint socket and tries to tighten a loosened capsule.
More on the topic of reasons and procedure for a shoulder dislocation.
Whether an operation makes sense in an individual case depends on the extent of the injuries to the joint and the surrounding ligaments and tendons. If no structures have been injured and if it was a one-time dislocation, an operation can often be prevented.
- The advantages of an operation are that damage to the joint and the ligament system can be reliably repaired and a renewed dislocation of the shoulder can be avoided.
- Disadvantages of surgery can arise when complications arise. For this reason, the shoulder should only be operated on if the treating orthopedic surgeon or trauma surgeon indicates that it should be performed. An infection of the joint is a risk of the operation, which leads to another operation or long-term treatment. Since the procedure is usually carried out using a minimally invasive technique, large blood losses or nerve injuries usually do not occur. A stiff shoulder often occurs after the operation, which can be prevented by intensive physiotherapy and active training during the follow-up treatment.
Read more on the topic: Arthroscopy complications
Aftercare
It is especially important that the therapy does not end after the operation of a shoulder dislocation. The follow-up treatment is at least as relevant as the operation itself in order to achieve good function of the shoulder joint and mobility in the shoulder. The shoulder is usually immobilized first with a sling. Even slight movements may and should be carried out without strain, but intensive physiotherapy usually does not begin until about 3 weeks after the operation. This is essential so that complete mobility in the joint is regained and there is no frozen shoulder. The time it takes for the disease to heal should therefore include follow-up treatment. Including follow-up treatment, depending on the extent of the injury, it can often take 6-8 weeks until the shoulder is fully functional again.
Pain that occurs as part of the follow-up treatment of an operation after shoulder dislocation is to a certain extent to be regarded as normal. It may be that pain that occurs after prolonged immobilization is caused by a frozen shoulder. The treatment of pain that occurs with a shoulder dislocation should be discussed with the attending physician. Often, taking so-called NSAIDs such as ibuprofen or diclofenac is enough to significantly alleviate the symptoms.
Physiotherapy / physiotherapy
Physiotherapy is primarily used to keep the shoulder in shape after a treated dislocation in order to prevent functional restrictions. A distinction is made between exercises that strengthen the muscles and those that make the shoulder more flexible. A typical strengthening exercise is the forearm support. You take the push-up position, with the difference that you put your forearms on the floor instead of your hands. An exercise that promotes mobility is rotating your arms in alternating directions. In physiotherapy, these and similar exercises are performed under supervision.
Exercises
After the reduction of the dislocation, it is important to carry out exercises for the shoulder joint, since immobilization of the joint can quickly lead to stiffening of the joint. The type of exercise depends on the extent of the damage to the joint and the therapy being performed.
Read more on the topic: Frozen shoulder
If only conservative therapy was necessary, the shoulder repositioned and the muscular and ligamentous apparatus of the shoulder intact, physiotherapy can be started immediately. Strength-building training therapy on machines as they are known from the gym, but also free movements with dumbbells or elastic bands are options to increase shoulder strength. Exercises with straps or dumbbells in particular can also be performed from home if the treating physiotherapist has explained how to perform the exercise.
Read more on the topic: Exercises in strength training, strength training without equipment - tips for at home
If the shoulder has been stabilized again with an operation, no intensive exercises should initially take place. While only light pendulum exercises of the arm should be done for the first three weeks, the intensity should be increased afterwards. The physiotherapist and the treating orthopedic surgeon / trauma surgeon should discuss how much the joint can be loaded. Doing exercises on your own is also recommended to prevent frozen shoulder.
bandage
Depending on the extent of the injury, it can make sense to wear a bandage for some time, which relieves and stabilizes the shoulder joint. A bandage has an enormous healing effect in treating shoulder dislocations. There are a number of different products from different manufacturers. The so-called Gilchrist bandage is used most often. Most of the dressings available have in common that the affected arm is fixed to the trunk while the elbow is flexed. The shoulder joint is restricted in its movement by the bandage, but a certain movement is usually still possible. Bandages are usually comfortable to wear. The bandage may be removed for personal hygiene.
Kinesio tapes
One way to fix the shoulder joint and to increase the stability and strength in the joint is to use a kinesio tape. Kinesiotape is an elastic, stable tape that can hold the head of the humerus in the socket during the follow-up treatment of a shoulder dislocation and support the muscles that stabilize the shoulder. To ensure the correct application of the kinesio tape, an experienced physiotherapist or the treating orthopedic surgeon or trauma surgeon should apply the bandage.
Read more on the topic: Tape dressing, taping a torn ligament
Complications of a shoulder dislocation
Several unintended complications can occur with a shoulder dislocation. A common occurrence that a shoulder dislocation can bring about is a re-dislocation of the shoulder. Since the ligaments and muscles have been worn out or weakened, they can no longer hold the bone stable and no longer secure it in its basic position. The effects of forces or movements that previously did not cause any problems can lead to a dislocation. The great danger here is that the greater the number of dislocations, the greater the risk of a new dislocation, with the result that the patient is in an almost ever deeper downward spiral, unless something is done about it. A shoulder dislocation can also damage the surrounding tissue. Cartilage and / or bone damage are known complications that can occur. Since nerves and vessels also run in the shoulder area, they can be damaged during dislocation. The result is movement and sensitivity disorders in the shoulder and upper arm.
Labrum tear
The joint lip, the so-called "Glenoid labrum“, Are bulge-like ligaments around the joint socket. They serve to hold the humerus head mechanically in the joint socket. The labrum tear is a possible complication that can occur with a shoulder dislocation. The ligaments do not tear, but detach from the edge of the joint socket. Of course, this only happens when the force is very strong. As the labrum is detached, it loses its stabilizing effect. Treating a torn labrum involves reattaching it to the edge of the joint socket in an operation and thus restoring the shoulder joint to its original stability.
Total healing time
A shoulder dislocation does not usually heal on its own and should therefore always be corrected by a doctor. As a rule, the shoulder must be spared for 4-6 weeks. From this time onwards a slow mobilization begins. It is estimated that after 7 weeks the shoulder can be used again without any symptoms and fully functional. It should be noted, however, that heavy loads on the shoulder, such as those that occur during sports, must not be carried out after 7 weeks, as there is an increased risk of renewed dislocation.
However, the time required for healing depends heavily on the severity of the dislocation. During this time, careful exercise and physiotherapy can already be started in order to prevent a breakdown of the muscles and to minimize the risk of a renewed dislocation. Regeneration can take much longer after an operative reduction.
How long can you not do sports?
After a shoulder dislocation, it is strongly recommended not to exercise for up to six months after the event. To ensure complete healing, it is imperative to adhere to this guideline, as the risk of dislocation is far too high. Since each shoulder dislocation is individual, the doctor has the last word in each case. It may well be that he allows you to be more active in sports. Of course, it also depends on which sport is being practiced.
forecast
- For traumatic (recurrent) shoulder dislocations
- The likelihood of a recurrent (= renewed) dislocation is greater, the younger the patient and the greater their physical activity.
- The restrictions due to the individually different extent of joint involvement of a dislocation and the associated different type and duration of the therapeutic measures carried out play a major role with regard to the risk of further dislocation, so that only the treating physician can make the individual prognosis.
- in atraumatic, habitual shoulder dislocations
- The probability of a recurrence is greatly increased, since the repositioning and the subsequent treatment - if not performed surgically - did not cause any changes with regard to the partially congenital cause
Prevention
- Adequate immobilization and consistent physiotherapy after the first dislocation
- Adaptation of physical / sporting activities, if necessary avoiding stress on the shoulders
- Possibly. also early surgical reconstruction to prevent reluxations
Symptoms of a shoulder dislocation
The most obvious symptom of an acute shoulder dislocation is severe pain in the shoulder area. Every movement of the arm leads to further severe pain, which is why an affected person will hardly move the arm and tries to keep it as still as possible. Next, swelling and bruising will usually be noticeable and the shoulder will lose more mobility due to the swelling. A shoulder dislocation is often visible through the skin. The acromion protrudes clearly and the head of the humerus is palpable. Since nerves run along the head of the humerus, a dislocation can damage them, which can lead to numbness or similar sensory disorders in the shoulder and arm. Another obvious symptom is a flattened contour of the deltoid muscle with a visible pit on it. The pit comes from the fact that due to the empty joint socket due to the missing humerus head there is a hole at the point and is visible in a depression.
Read more about this under: Shoulder pain
Pain
The pain of a dislocation of the shoulder that has just occurred is severe and usually almost unbearable. The pain persists until the shoulder dislocation has been treated. This includes repositioning the joint or giving pain medication. If the reduction is successful, there should basically be no more pain as the cause of the pain has been eliminated. During an acute dislocation, it is almost impossible to move the upper arm without pain. Because of this, the arm is placed in a kind of relieving posture that usually looks bizarre to outsiders. If the pain persists despite treatment, it should be checked whether there is a side effect, such as damage to nerves, vessels or ligaments.
Pain that occurs as part of the follow-up treatment of an operation after shoulder dislocation is to a certain extent to be regarded as normal. It may be that pain that occurs after prolonged immobilization is caused by a frozen shoulder. The treatment of pain that occurs with a shoulder dislocation should be discussed with the attending physician. Often, taking so-called NSAIDs such as ibruprofen or dicofenac is sufficient to significantly alleviate the symptoms.
Duration of pain
The pain when the shoulder is dislocated is greatest when the shoulder is dislocated. The pain intensity is relatively strong, which is why a dislocation is immediately noticeable. As soon as the shoulder is back in position, the pain subsides, unless structures such as vessels or bones were affected during the dislocation. Persistent pain in the shoulder may indicate this is the case and may indicate the need for additional diagnostic measures. The pain of an acute dislocation can be minimized by administering painkillers. If the treatment is successful, there should be no more pain.
Other accompanying symptoms
Another symptom that can occur with a shoulder dislocation is nerve irritation. This creates a tingly feeling and possibly numbness in the affected area.
In addition, the movement of the shoulder is severely restricted because the head of the humerus and the socket joint of the shoulder blade no longer interlock. Usually a bruise and swelling can be seen on the shoulder and a dent in the bone contour can be felt or sometimes also visible.
If the shoulder is dislocated, there is a risk of injuring the surrounding structures. Above all, the muscles and tendons of the supporting apparatus are threatened. If these tear, surgical intervention may be necessary. The biceps tendon also runs near the shoulder joint and can be damaged. In addition, nearby blood vessels and nerves are at risk.
How does a shoulder dislocation occur?
As already briefly described above, there are different causes for the occurrence of a shoulder dislocation.
Most often, however, a levering movement of the upper arm with simultaneous external rotation is seen, in which the arm moves away from the body. In the case of a shoulder dislocation, the head of the humerus usually jumps forward (luxatio axillaryis) or forward (luxatio subcoracoidea). Dislocations to the rear are rather untypical. Very rarely does a shoulder dislocate when the arm is extended upwards. As a rule, shoulder dislocations have traumatic causes: falls, sports, bicycle or other traffic accidents should be mentioned in this regard.
The more rarely occurring habitual (habitual) shoulder dislocations (see above) lead to a dislocation without adequate trauma (minor trauma) due to individual circumstances (e.g. congenital acetabular dysplasia).
Diagnosis of shoulder dislocation
The diagnosis of shoulder dislocation primarily includes the clinical examination. However, depending on the severity, this can be difficult under certain circumstances. Especially with Distortions (Twists) and Subluxations (incomplete dislocation) the anamnesis is therefore very indicative in order to differentiate between the various forms of severity.
During the clinical examination, the doctor feels the shoulder and, in the event of a dislocation, can feel the empty joint socket, the protruding bony roof of the shoulder and the dislocated head of the humerus. If you try to carefully straighten the dislocated arm again, it jumps back into the wrong position, which is known as "resilient fixation". In addition, possible accompanying injuries such as damage to a nerve should be covered by the examination.
Necessary technical investigations
- X-ray of the shoulder in 2 planes to delimit the type and to determine any accompanying bone injuries. An X-ray can also be used to determine whether there are causes for the dislocation (e.g. dysplasia, etc.).
In individual cases, useful technical investigations
- Sonography (especially to rule out a rotator cuff lesion)
- Special x-ray images, e.g .: Velpeau image (relationship between humeral head and socket), ventrodorsal 60 ° internal rotation image (Hill-Sachs image), socket profile image
- MRI of the shoulder joint
- CT (possibly air arthro CT)
What do you see in an MRI?
Diagnosis by means of an MRI is of central importance in many injuries. The importance is based on the fact that the extent of the injury can best be determined with an MRI, since an MRI image shows joints and soft tissues very well. As a result, the treatment planning can be optimally determined. An MRI can reveal bony injuries, such as a notch in the back of the head of the humerus. A special focus is on the joint lip. This is a ligament ring that lies around the socket. A detachment of this joint lip can be clearly seen in the MRI. An important criterion is also the assessment of the condition of the biceps tendon and the nerves running there.
Read more on this topic at: MRI of the shoulder joint
What are the causes of shoulder dislocation?
The distinction between a traumatic and an atraumatic shoulder dislocation has already been pointed out. The respective causes for the emergence of the two forms of Shoulder dislocation are described in more detail below.
The post-traumatic recurrent shoulder dislocation presupposes a traumatic first dislocation and can therefore be assessed as a partial form of traumatic shoulder dislocation.
Traumatic (accident-related) shoulder dislocation
The causes of a traumatic shoulder dislocation are, for example:
- Accidents or
- Force effects
For example, it occurs most often as a result of a fall: When trying to catch yourself with your arm, the shoulder joint is suddenly exposed to great pressure and may be rotated unfavorably. Because of this, the ligament and muscle supporting apparatus can no longer hold the joint and it becomes dislocated.
Something similar can happen in some sports, for example tennis, skiing and handball.
Depending on the direction of the force and thus the dislocation, a distinction is made between anterior, posterior and lower shoulder dislocation, with the anterior being by far the most common. A classic cause of a front shoulder dislocation is a fall backwards in which the arm hits the ground unhappily.
While sports accidents are the most common cause of shoulder dislocations in young people, the risk of falling is a major risk for older people. In addition, the stability of ligaments and muscles in the body often decreases over the years. Previous dislocations are also a risk factor, since the ligamentous apparatus lends itself out over time.
Post-traumatic recurrent shoulder dislocation
The causes and injury mechanisms of the post-traumatic recurrent shoulder dislocation are considered to be largely clarified. Due to their designation, they are considered "recurrent“, So that a traumatic (accident-related) initial dislocation must have already occurred, which may also U. not healed as planned.
The most common causes of post-traumatic recurrent shoulder dislocation are:
- Remaining damage after initial traumatic dislocation, which usually first occurs in adulthood.
- Cartilaginous / bony Bankart lesion (= Tear of the glenoid labrum in the context of an anterior shoulder dislocation)
- Hill-Sachs lesion (= Impression on the dorsolateral (towards the back, lateral) edge of the humeral head; in the case of habitual dislocation)
- Weakness of the capsule-ligament apparatus
- Loss of Proprioception (= Loss of perception and control of the body's position in space; impaired sensitivity)
- Muscle weakness despite adequate rehabilitation
Habitual (multidirectional) shoulder dislocation
In the area of habitual shoulder dislocation, both the etiology and the development of the disease have not yet been adequately clarified. Classically, there is an initial dislocation within this subgroup, which is usually processus coracoidia (= Raven beak headset), is directed forward and down. A habitual first dislocation occurs predominantly in children to adolescents. As a rule, instability remains, which is usually very painless. In addition, certain factors are assumed that can have a positive effect on the development of a habitual shoulder dislocation:
- Anomalies in the area of the capsular ligament apparatus
- Changed collagen cross-linking or composition of the capsule
- Dysplasia of the shoulder socket (insufficient position of the socket)
- Increased inclination of the socket towards the front, reduced rotation of the humeral head towards the rear
- congenital connective tissue weakness
- Ehlers-Danlos syndrome (hyperelasticity, increased vulnerability and impaired wound healing of the skin, overextension of the joints with a tendency to dislocate; hereditary symptoms)
- Marfan syndrome (hereditary disease, special connective tissue disease: changes in the eyes, habit and the cardiovascular system)
- Muscular disorder
anatomy
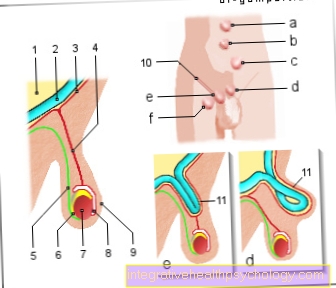
The Shoulder joint (= Articulatio humeri) lies between the humeral head and the joint socket (Cavitas glenoidales) of the shoulder blade. Due to the shape of the joint, it is one of the most flexible joints in the entire body. This form of the joints is called: BALL JOINTS.
The relatively large range of motion of the shoulder joint is due to its anatomy. The shoulder socket, for example, is quite small compared to the humeral head. In addition, the muscles and joint capsules allow a lot of play due to their relatively loose tension.
At first glance, a relatively large range of motion does not appear to have any disadvantages. The greater the freedom of movement, the more opportunities a person has to move. If, however, traumatic events occur or if there are individual (innate) causes, it is all the easier for a "atraumatic ”(habitual) dislocation.
Healthy shoulder joint
- Humerus head (Humerus)
- Shoulder height (Acromion)
- Shoulder joint
- Collarbone (Clavicle)
- Raven beak extension (Coracoid)
- Shoulder joint (Glenohumeral joint)
classification
Since there are different forms of shoulder dislocation, one tries to classify them as clearly as possible. So far there is no generally valid form of classification. They are described in terms of cause and direction of the dislocation, as well as in terms of shape and degree. The following criteria therefore appear in combination with one another in order to describe the respective dislocation.
Pathogenesis (cause):
- Traumatic
- unidirectional
- Atraumatic
- The following forms of dislocation can occur in the context of an atraumatic shoulder dislocation:
- Habitually unidirectional
- Habitually arbitrary
- Habitually multidirectional
Locations of the Shoulder dislocation:
- Anterior-inferior (front-lower) = luxatio subcoracoidea
- posterior-superior (back-top)
- Combinations
Severity of Shoulder dislocation:
- Grade I (distortion):
- strain
- The capsule and muscles are intact
- Some fiber cracks can be found
- Grade II (subluxation):
- Partial muscle lesion
- Capsule rupture or capsule detachment
- Grade III (dislocation):
- Capsular ligament lesions are always present
- Usually the dislocation occurs forwards (in about 96% of all cases)
Epidemiology
The shoulder dislocation as such occurs very rarely. One goes from 15 per 100,000 patients annually out.
perspective
An expansion or improvement of the arthroscopic techniques can be expected.
Medium- and long-term results of the arthroscopic operations as well as the laser techniques remain to be seen.
Studies have yet to prove whether early reconstruction after the initial dislocation has an impact on the recurrence rate.