Sickle Cell Anemia - How Dangerous Is It Really?
definition
Sickle cell anemia is a genetic disease of the blood or, more precisely, of the red blood cells (Erythrocytes).
There are two different forms depending on the inheritance: a so-called heterozygous and homozygous Shape. The forms are based on a disturbed form of the erythrocytes. When there is a lack of oxygen, these take on a sickle-like shape, which gives the disease its name.

causes
The cause of sickle cell anemia is genetics / inheritance. It is about a autosomal codominant hereditary diseasei.e. that its genetic equivalents are not on the sex chromosomes, i.e. one affected parent is sufficient to pass the disease on to their child.
The exact cause lies in the exchange (more precisely: point mutation) of a single amino acid: the amino acid glutamate is replaced by the amino acid valine.
Glutamate, along with many other amino acids, is part of the protein hemoglobin, which is known to be the oxygen carrier on red blood cells (erythrocytes). The intended spatial shape of the hemoglobin is not achieved through the use of the "wrong" amino acid valine. The result is a changed hemoglobin, called HbS (hemoglobin of sickle cell anemia).
As a substitute, another hemoglobin is also formed: HbF (fetal hemoglobin), which is actually only formed in the fetal period of an unborn child. It has a higher affinity for oxygen and serves as a compensating replacement for oxygen transport.
The hemoglobin molecules of sickle cell patients at the end of production consist of 20% HbF and 80% HbS. This leads to a loss of elasticity in the erythrocytes, but their flexibility is essential when they pass through the smallest of blood vessels.
If a person has the disease from both parents, both copies of the corresponding gene for hemoglobin are affected. He is a so-called homozygous carrier. In these people, 100% of all hemoglobins are changed and even minimal changes in oxygen levels in the blood cause them to assume a sickle shape.
In the case of a heterozygous carrier, only one parent was sick or passed the disease on. A severe lack of oxygen is required here for the hemoglobin and thus the erythrocytes to change.
Regardless of whether the carrier is homozygous or heterozygous, the mechanism of the disease is the same: as soon as a molecule takes on the wrong shape, it is broken down. This can happen in the blood vessels or in the spleen (see hemolysis). This means that those affected have fewer erythrocytes in total in their blood (anemia = anemia), so their oxygen supply in the body through the blood is not guaranteed.
You can find out how anemia makes itself felt in our article Anemia - these are the signs!
diagnosis
Several methods can detect the sickle cell shape of red blood cells. The easiest way to do this is by looking at it: if you spread a drop of blood on a glass slide and seal it against air, the affected erythrocytes take on the sickle shape (sickle cells or Drepanocytes called). Also so-called target cells or Target cells can be e.g. recognize in this form of anemia: they have a concentrated red color in the center and generally indicate a loss of function of the cells. This form can also occur with other anemias and is therefore not specific.
Most accurate is a chemical process with the complicated name of high pressure liquid chromatography. This is able to separate different molecules and compare them with one another. The changed hemoglobin molecule HbS can be identified.
Occurrence
Sickle cell anemia occurs mainly in Africa and the eastern Mediterranean.
In Germany it is practically non-existent, and if it does, then it occurs with refugees or people with a migration background. In 2010 it was ascertained that there were around 1000-1500 sickle cell patients in Germany, mainly from Turkey, Italy, Greece, North and Central Africa, the Middle East and India.
The spatial restriction is likely due to a selection advantage due to malaria.
frequency
Sickle cell anemia is the most common corpuscular (blood cell) anemia worldwide, presumably also because of the selection advantage.
Depending on the level of development in the country, malaria can also be fatal. In 2004, a record 1.8 million malaria deaths was estimated.
Special feature of malaria
It was first discovered by researchers in the 1940s that in the areas where the severe form of malaria (Malaria tropcians) occurred, many people had "different blood".
Malaria is a parasitic disease caused by the Anopheles mosquito is transmitted. The plasmodia (parasites) first attack the liver, then the red blood cells and continue to multiply in them. In people with sickle cell anemia, the plasmodia in the erythrocytes does not multiply. Exact causes are not known to this day. In this context, a person with sickle cell anemia can claim to be (partially) resistant to malaria.
You can find out more information about the dangerous infectious disease malaria and how you can protect yourself in our article Malaria!
Concomitant symptoms
The clinical picture of the complaints depends on whether the sufferer has a homozygous or heterozygous Carrier is.
In the case of the homozygous form, one can generally speak of the more severe form. Even in childhood, patients suffer from hemolytic crises and organ infarctions due to circulatory disorders.
A hemolytic crisis is a complication of hemolytic anemia. Hemolytic simply means that the blood dissolves and anemia the resulting quantitative anemia. If a hemolytic crisis occurs, this means a massively excessive breakdown of red blood cells, which is usually due to viral infections. It is a life-threatening condition with fever, chills, shock symptoms (including drop in blood pressure, paleness, rapid heart rate) and jaundice (jaundice). Intensive medical care is required here (see therapy).
Organ infarctions can also occur in homozygous carriers. Vascular occlusions can occur all over the body. The most common organs affected are the spleen, kidney, central nervous system, and bones.The spleen in particular, as an organ of blood breakdown, is particularly affected in hemolytic diseases. If there are repeated vascular occlusions (infarcts), the spleen increasingly loses its function and shrinks.
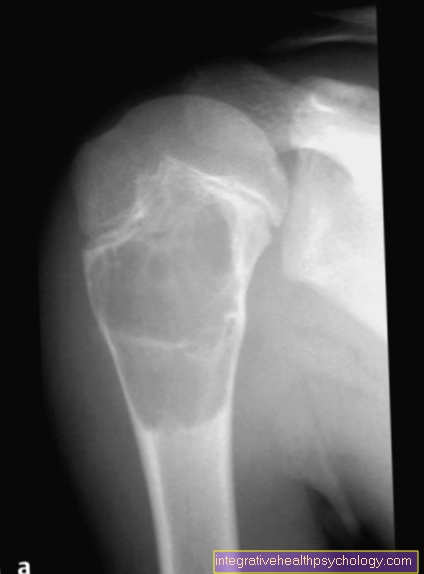
The kidney as a filter organ can be affected just as easily: this clinical picture then corresponds to a "chronic glomerulonephritis" (permanently inflammatory state of the smallest filter subunits of the kidney). With regard to the bones, the femoral head and the humerus should be mentioned: like any other organ, they require an adequate blood supply. If this is not guaranteed, aspeptic bone necrosis occurs (death of the tissue without responsible pathogens).
Classic strokes can occur in the brain. The bone marrow is also affected by the changed shape of the erythrocytes: for example after infection with the Parvovirus B19 (Rubella) there may be a short-term shortage of erythrocytes.
The clinical picture of heterozygous carriers is quite different: mostly those affected do not notice anything about their illness, as it is milder. They decompensate only in extreme stressful situations, which can be all the more dangerous when they occur for the first time. These physical emergency conditions can be extreme sporting activity, pregnancy, an operation and, in particular, connection to a heart-lung machine.
You can find out which symptoms hemolytic anemia still has in our article Hemolytic anemia!
therapy
In homozygous carriers, an attempt can be made to integrate the cultivation of normal erythrocytes in the body with an allogeneic stem cell transplant. For this, the blood-forming stem cells are transferred to a sibling or a stranger, which then take over the (correct) blood formation.
This is also done, for example, in the case of malignant diseases of the blood such as leukemia.
Overall, a person affected should avoid a lack of oxygen and, in the event of a hemolytic crisis, receive adequate intensive care. This also includes, for example, sufficient fluid substitution or a blood transfusion (in order to ensure the transport of oxygen in the blood again).
You can find out more information about a stem cell transplant, what the risks are and what the costs are in our article Stem cell transplant.
forecast
In principle, sickle cell anemia is an incurable disease due to its genetic cause. Only the attempt at stem cell transplantation can be undertaken. Depending on the level of development in the country of the person affected, people have a lower life expectancy. The hemolytic crises caused by infections, for example, are most likely to lead to death from organ failure.
Regular vaccinations and prompt care in the hospital help improve the prognosis.
Special features in pregnancy
Only homozygous patients have problems during pregnancy due to their sickle cell anemia: First and foremost, the increased risk of thrombosis should be mentioned, but this does not require any drug treatment such as anticoagulation (anticoagulation), but only close monitoring (twice as often as in healthy people).
Patients with sickle cell anemia show no increased risk of miscarriage or premature birth; the children only have a lower birth weight compared to the average.
An absolute contraindication (counter-recommendations) for pregnancy is if the person concerned has already suffered severe complications from their illness such as strokes and chronic insufficiency of the heart, lungs or kidneys.
Furthermore, it has been observed in sickle cell patients that, for unknown reasons, they experience certain episodes of pain during pregnancy. Here analgesic (pain-relieving) therapy is used, as with other pregnant women. The number of studies on pregnant sickle cell patients and their children is still incomplete and will require further extensive research in the future.
More on this: Thrombosis in Pregnancy
Which drugs are contraindicated?
In principle, all drugs that increase the viscosity of the blood or impair the oxygen supply should be avoided. Sickle cell patients, for example, should avoid using contraceptives that contain estrogen, as these increase their risk of thrombosis.
Drugs that act on the autonomic nervous system and constrict blood vessels (Vasoconstrictors) or decrease the oxygen exchange area in the lungs (Parasympathomimetics, Sympatholytics; e.g. determine Beta blockers) should also be avoided.
What should you watch out for during anesthesia?
A heart-lung machine is used in operative management when the heart and / or lungs have a malfunction that requires surgery and they have to be operated on or even have to be transplanted. I.e. It can be assumed that the affected body was already in a relative oxygen deficiency state before the operation, ergo the sick erythrocytes have assumed their sickle cell shape under oxygen deficiency.
The greatest danger is the haemolytic crisis: after connection to the heart-lung machine, damaged blood cells are removed through a filter. It is important to ensure that the sickle cell anemia causes more blood cells to be filtered than in healthy people.
Strict monitoring of the balance between oxygen carriers (erythrocytes) and other components (proteins, plasma) is necessary. This can be achieved, for example, via transfusions (red blood cell concentrates, EK’s for short).
The fact that the blood cells suffer little mechanical damage as they flow through the heart-lung machine should also not be neglected. This fact is also taken into account in healthy people (i.e. patients not suffering from sickle cell anemia) and the viscosity of the blood is particularly monitored anyway.
Under strict operating theater management, sickle cell anemia can also be connected to a heart-lung machine, but should be accompanied by experienced transfusion and intensive care physicians and only take place if there are no other therapeutic options.