Green Star
Synonyms in a broader sense
Medical: glaucoma
English: glaucoma
definition
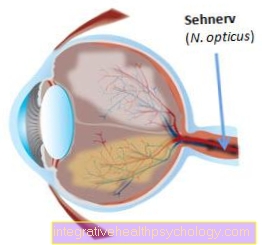
Green star (should no longer be used, however, as it can easily be confused with "cataract"). Green star is a generic term for a number of diseases that are associated with typical damage to the optic nerve papilla and the visual field.
The optic nerve papilla is the point in the eye where the nerve fibers exit or enter the brain. Typical changes in the eye that are typical of glaucoma are:
- individually increased intraocular pressure
- Visual field loss (scotoma)
(see also our topic examination of the visual field) - funnel-shaped indentation of the optic nerve papilla with breakdown of the nerve fibers (Papillary excavation)
A distinction is made between primary glaucomas (glaucoma) and secondary ones. Primary glaucomas (glaucoma) develop spontaneously, while secondary glaucomas are the result of other diseases.

Illustration glaucoma

Green star (glaucoma)
A - normal
Intraocular pressure
B -Increased
Intraocular pressure
- Dermis - Sclera
- Schlemm Canal
(Aqueous humor drainage) - Iris - iris
- Cornea - Cornea
- pupil
- Anterior chamber of the eye -
Camera anterior - Aqueous humor
(Flow direction) - Chamber angle -
Angulus irodocomealis - Radiation body -
Corpus ciliary - Aqueous humor production
- Vitreous - Corpus vitreum
- Eye lens - Lens
- Posterior chamber of the eye -
Camera posterior - Zanula fibers
- Drainage obstruction
- Intraocular pressure increases!
a - original
b - Earlier stage of the disease
c - Middle-stage disease
d - late stage disease
You can find an overview of all images from Dr-Gumpert under: medical images
Emergence of glaucoma
in the eye there is permanent internal pressure. On the one hand, this must not be too low, because otherwise the eye would collapse, and on the other hand, not too high, because otherwise the Optic nerve and the Retina Would suffer damage from it. The normal pressure is in the range of 10 mmHg to 21 mmHg.
The pressure is regulated by the aqueous humor. The aqueous humor is in the posterior chamber of the eye Ciliary body, an important structure behind the Iris (iris) produced.
From there it flows into the anterior chamber of the eye, in front of the iris, and then flows in the chamber angle through the so-called trabecular system (trabecular outflow) into the Schlemm Canal. A small part of the aqueous humor is also taken from the vessels of the Choroid (uvea) recorded (uveoscleral outflow). If this drainage is disturbed, it comes to Glaucoma / glaucoma.
Recognizing a green star
Classification of glaucoma
Since a glaucoma has different forms and glaucomas, a distinction is made between the following glaucomas:
Primary glaucoma
- Open-angle glaucoma:
Cartilage-related substance deposits in the trabecular system- Special forms: ocular high pressure (hypertension) and normal pressure glaucoma
- Angle closure glaucoma:
Relocation of the chamber angle due to a too narrow chamber angle or adhesions (goniosynechiae) - Subforms of angle closure glaucoma:
- Acute angle closure glaucoma:
Either a congenitally narrow chamber angle, farsightedness or a relatively large lens, e.g. the age lens. But the dilatation of the pupil, as is the case in the dark, or eye drops that enlarge the pupil, are also frequent triggers - Intermittent angle closure glaucoma:
Precursor of acute angle block glaucoma - Chronic angle closure glaucoma:
Bonding of the chamber angle, e.g. for not treating acute glaucoma in a timely manner - Congenital glaucoma:
Incorrect development of the trabecular structure
- Acute angle closure glaucoma:
Secondary glaucoma
- Neovascularization glaucoma (neovascularization = new blood vessels):
New blood vessels and connective tissue (fibro-vascular) membranes in the area of the chamber angle lead to an occlusion (often in diabetes mellitus or occlusion of central veins of the eye) - Pigment dispersion glaucoma:
Deposits of pigment in the chamber angle - Pseudoexfoliative glaucoma:
Fine fibrillar deposits (especially from the cialiar body) - Cortisone glaucoma:
Accumulation of mucous components (mucopolysaccharides) in the chamber angle, caused by high and long-term corticosteroid medication (cortisone treatment) - Inflammatory Glaucoma:
Fluid retention (edema) or deposits of inflammatory proteins in the chamber angle - Injury Glaucoma:
Torn or scarred angle of the chamber - Rieger syndrome, Axenfeld anomaly, Peter’s malformation:
Developmental disorders and malformations of the chamber angle
Primary open-angle glaucoma is the most common form of glaucoma (around 90 percent of all glaucomatous diseases). Important risk factors that influence the development of open-angle glaucoma are:
- an age over 65 years
- Diabetes (diabetes mellitus)
- certain cardiovascular diseases (condition after heart attack, heart failure)
- Nearsightedness and farsightedness (myopia)
- long-lasting (chronic) inflammation of the eye
- chronic cortisone ingestion
- frequent occurrence in the family (e.g. with parents, grandparents, etc.)
What are the symptoms of a glaucoma?
- Glaucoma attack / acute angle block
Suddenly severe pain occurs in the diseased eye and the half of the face on the same side. They are described as dull, oppressive, or deep-seated and are often initially mistaken for a headache attack. They may radiate into the entire face, teeth or even into the abdomen. Sometimes patients experience dizziness through the eyes
Read more on the topic:
- Eye pain
- Pain over the eye
- Corneal edema in the eye
The disease often causes nausea, malaise, and vomiting. In connection with the headache that occurs, a migraine attack can easily be thought of.
Typically, those affected report that they perceive their surroundings through a kind of fog or veil. In the dark, colored rings are seen around the light source.
In connection with glaucoma, the heart often beats too slowly (bradycardia) or irregularly (arrhythmically).
- Intermittent angle block
If patients are affected by a so-called intermittent angle block or glaucoma, the symptoms described appear in a milder form. The symptoms disappear spontaneously and return at a later point in time. For this reason, those affected often go to the ophthalmologist very late. Often, however, after the symptoms have increased and decreased several times, a complete attack of glaucoma occurs. So do not hesitate to consult your ophthalmologist even after observing the symptoms once!
- Open-angle glaucoma
Open-angle glaucoma is particularly problematic! Those affected usually only notice it in the terminal stages. Subjectively, there are no visual disturbances or pain. If visual disturbances occur, they are usually difficult to describe. Typically the loss of visual acuity is accidental, e.g. in everyday situations: While going to the cinema, an elderly lady notices that at first she cannot recognize an object that the actor is holding in his hand. Only on closer inspection can she see him clearly. During a subsequent visit to the ophthalmologist, the patient describes that she did not notice a 'blind spot' in her field of vision. However, if she closed her good eye, she would simply not perceive parts of her surroundings.
The following situation can also be typical of open-angle glaucoma: A man reports to his family doctor that he has had difficulty driving in the past few months. Several times he had not noticed parked cars on the left in time. Except for a few broken exterior mirrors, nothing happened. During the visual field examination, there were deficits in the left outer field of vision, so-called 'scotomas'. So finally the diagnosis of 'open-angle glaucoma' of the left eye was made. The symptoms of this form of glaucoma can be very hidden and subtle!
Learn what Scotomas what causes them and how to treat them.
- Congenital glaucoma
In the innate form of the glaucoma, the newborns stand out with their very large, 'beautiful' eyes. At the same time, the eyes water heavily and are sensitive to light. Babies often find it difficult to open their eyelids ('eyelid cramps').
- Secondary glaucoma
If there is another eye disease (e.g. circulatory disorders of the retina in the context of diabetes mellitus) that causes the glaucoma, it is secondary glaucoma. Symptoms vary depending on the type of secondary glaucoma and range from pain to visual disturbances.
Read more on the topic: Glaucoma symptoms
How is a glaucoma diagnosed?
The diagnosis of glaucoma includes examinations of intraocular pressure (tonometry), visual field (perimetry) and the fundus (ophthalmoscopy), with a special focus on the optic nerve optic disc.
The first evidence of glaucoma is intraocular pressure> 21 mmHg. But intraocular pressures in the normal range (10-21mmHg) can also cause glaucoma (see normal pressure glaucoma)!
The visual field examination is used to check the extent of the damage. At the primary open-angle glaucoma The visual field loss (scotoma) often develops very slowly, so that limitations are only perceived subjectively at a very late stage.
Finally, ophthalmoscopy allows the optic nerve papilla to be assessed. This is the point in the eye where the nerve fibers exit or enter the brain. Due to the increased intraocular pressure, or in normal pressure glaucoma also with statistically normal intraocular pressure, the papilla can be dented (papilla excavation). The extent of the indentation is closely related to the degree of damage. The larger the indentation, the greater the damage.
In further glaucoma examinations, the chamber angle at which the aqueous humor drains can also be examined. To do this, the doctor uses the slit lamp and so-called gonioscopy lenses, which are placed on the anesthetized cornea and with which it is possible to examine the angle of the chamber. This way, possible adhesions (goniosynechiae) can be discovered, which impede the drainage.
On one acute attack of glaucoma indicate the symptoms of glaucoma. Since the cause here is an "angle block", the angle assessment (gonioscopy) is particularly important.
The diagnosis of secondary glaucoma results on the one hand from the results of the eye examinations and on the other hand from the underlying disease that caused the glaucoma.
Therapy for glaucoma attacks / acute angle block, intermittent angle block:
In the event of a glaucoma attack, the increased intraocular pressure must first and foremost be reduced with the usual medication (see above). This is followed by an operation, even if the intraocular pressure has been successfully reduced! Doctors speak of an 'iridectomy': During the procedure, a small piece of the iris, usually in the upper part, is removed. This creates an artificial connection between the anterior and posterior chambers of the eye. The aqueous humor can flow directly into the anterior chamber and the angle block is bypassed.
In addition to this surgical procedure, there is also the option of laser treatment. A high-performance Nd: YAG laser is used to shoot a hole in the iris, creating a direct drainage into the anterior chamber of the eye. Laser iridectomy is particularly suitable for patients whose intraocular pressure has been lowered very successfully with medication, but also as a precautionary measure on the second eye. In addition, the laser method can be a real alternative for those affected whose general condition no longer allows conventional operations.
As a rule, the laser operation is carried out under local anesthesia of the eye. The classic glaucoma operation, on the other hand, can be performed under local or general anesthesia.
Therapy for congenital glaucoma
In the case of congenital glaucoma, medication is insufficient and the newborn must be operated on (filtration operation, trabeculectomy).
Therapy for secondary glaucoma:
If glaucoma develops due to another eye disease, the treatment of this eye disorder is the focus. Before doing this, of course, the intraocular pressure must be lowered using known methods.
Unfortunately, according to current research, the green star is not curable. However, modern medicine offers numerous possibilities to strongly influence the progression of the disease.
The first priority is the early detection of glaucoma. Because if the disease is noticed early, the chances of a largely stable, lifelong vision are very good. Up to now there are no studies as to whether nationwide glaucoma early detection makes sense and whether it is covered by health insurance companies. However, if there is an initial suspicion of glaucoma, such as a familial accumulation, personal risks (diabetes mellitus, long-term treatment with steroids such as cortisone, etc.) or if you even have typical symptoms, the health insurance will of course take over the necessary examinations. If in doubt, speak to your ophthalmologist about possible glaucoma screening! Those affected, however, have to be aware that they suffer from a chronic illness and therefore have to undergo ophthalmological treatment for their entire life. It is therefore all the more important to have a trustworthy ophthalmologist by your side. In addition to strictly adhering to the medication plan, it is important to observe the strict rules of conduct after surgery on the eye. In addition, the intraocular pressure must be measured by the ophthalmologist at tight time intervals.
An untreated glaucoma always leads to blindness.
Read more on the topic: Glaucoma surgery
Treating a glaucoma
How is a glaucoma treated?
When treating a glaucoma, these different therapies are used depending on the severity:
Therapy for open-angle glaucoma:
Therapy for open-angle glaucoma also aims to reduce intraocular pressure. Drug therapy usually comes first. For this purpose, the attending ophthalmologist sets a patient-specific 'target pressure': How high should the intraocular pressure be so that glaucoma damage can be prevented in the future? Personal risk factors, existing eye damage, life expectancy and the level of intraocular pressure at the time of the glaucoma attack must be taken into account in the calculation.
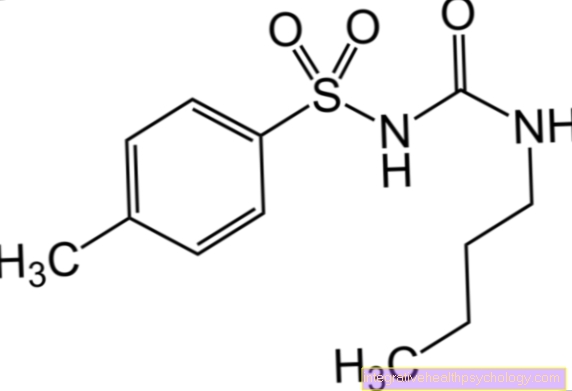
Eye drops with different active ingredients are suitable for lowering intraocular pressure. The five conventional groups of active substances include: prostaglandin derivatives, beta blockers, carbonic anhydrase inhibitors, sympathomimetics and parasympathomimetics. In order to check the success of a drug therapy, the intraocular pressure is controlled very carefully. The nurses in the eye clinic create a so-called 'daily pressure profile', where hourly changes are recorded. Often even a night measurement is carried out!
If the eye drops are not effective enough, the glaucoma must be operated on or treated with a laser.
During laser treatment, tiny points of light are shot very specifically at the trabecular structure of the chamber angle. This causes the tissue to scar and shrink. In this way, the narrow meshes of the trabecular network can widen and the aqueous humor flows off better. Unfortunately, the duration of the effect of this method is not always long-lasting.
Another possibility is what is known as 'cyclophotocoagulation'. There is a simple principle behind this complicated expression. The aqueous humor is formed by a special layer of cells in the eye, the ciliary epithelium. This cell layer is now attacked with an infrared laser and partly destroyed ('desolated'). As a result, it produces less aqueous humor and the intraocular pressure drops.
If both medication and laser therapy fail or are not an option, the final step can be eye surgery.
The following procedure may seem difficult to understand for the medical layperson at the beginning: During the filtration operation, a new drainage path is created under the conjunctiva. Many veins and lymph vessels run there, which can easily remove the aqueous humor. First, a small lid is cut into the dermis of the eyeball in the area of the trabecular structure. Then another opening is created directly through the trabecular network so that there is a connection to the anterior chamber of the eye. The previously prepared lid of the dermis is now placed on this opening and fixed. In this way, the flow of the anterior aqueous humor can be restricted.
Finally, the conjunctiva is closed tightly over it. The outflowing aqueous humor can slightly arch the conjunctiva forwards. The ophthalmologist then speaks of an ophthalmic pillow. Although the filtration method is very successful in reducing intraocular pressure, it is not entirely safe. Wound healing often causes major problems, as germs can easily get through the opened eyeball and scarring can occur. Therefore, metabolism-inhibiting drugs such as mitomycin C are applied to the wound during the operation.
The latest surgical techniques can lower intraocular pressure without opening the eyeball. This significantly reduces complications!
Preventing a glaucoma
What are the causes of glaucoma?
The causes of a glaucoma are diverse, but a common factor is an individually too high intraocular pressure.
As mentioned above, this comes about exclusively through a reduced outflow of aqueous humor. But pressure in the normal range can also lead to a form of glaucoma (normal pressure glaucoma). The cause of the glaucoma has not been researched in detail, so the previous definition was changed from “too high intraocular pressure” to “individually too high intraocular pressure”.
There are many different subforms of glaucoma (see classification), but what they have in common is the obstruction of the aqueous humor outflow.
Course of a green star
What is the prognosis of a green star?
Treated in time, the glaucoma can be stopped or at least slowed down.
The visual field damage can no longer be repaired (irreversible damage).
It also depends on the type of glaucoma. While that primary open-angle glaucoma develops slowly over the years, one can acute attack of glaucoma lead to blindness within a very short time.
In congenital (congenital) glaucoma, despite timely treatment, there is unfortunately often little damage that affects visual acuity.
Both Secondary glaucoma the prognosis depends on the underlying disease and its optimal treatment.
In particular, it can lead to damage to the optic nerve (optic atrophy). For more information on this topic, see Optic Atrophy.
Further questions about green stars
Related topics
More information on glaucoma:
- Glaucoma surgery
- Glaucoma symptoms
- Intraocular pressure measurement
- Examination of the visual field
- Cataract
- Eye surgery
- Pain behind the eye