Fall in old age
introduction
In the course of demographic development, Germany's population structure has been changing for decades. Due to falling birth rates and increasing life expectancy, the generation ratio is shifting in favor of the elderly.
According to a study by the Federal Institute for Building, Urban Affairs and Spatial Research, the average age in Germany will rise from currently 43 to 47 in 2030, and the 80-year-old population is expected to increase by 60% by 2030. The increase in the proportion of older people in the total population presents science and politics with new, major challenges.
Prevention (prophylaxis) and rehabilitation of the elderly will become increasingly important in the health and care system (rise in costs, care shortages, lack of assisted housing, etc.).
Dangers / complications of falling in old age
taining independence with the best possible health and quality of life is one of the great goals of today's senior citizens. However, increasing life expectancy is often associated with multiple physical limitations. In addition to the fear of illness or dementia, the elderly's concern that they will experience permanent limitation through a fall with injury and its consequences (possible disability, restriction of self-determined life, reduction in life expectancy) is a particular focus.
Around 30% of those over 60 years of age fall several times a year, with 80 year olds the risk of falling is already 50%. The risk of injury to seniors from falling in old age depends on various factors:
- Dizziness and imbalance
- Heart disease link
- dizziness
- Eye problems
- osteoporosis
- reduced strength, agility and responsiveness
- lack of or excessive self-confidence
are the most common causes of falls in old age.
The most feared complication in a fall in old age is the femoral neck fracture, which can often lead to disability or, in the worst case, death as a result of complications after surgery and lying down.
Fear of falling in old age
Only the fear of a fall, fueled by media information, personal experiences or "falling experiences" among friends or family can do considerable uncertainty of seniors in everyday activities trigger.
The term "Post Fall Syndrome“Describes the Interaction between fear and fallafter those affected have already experienced a fall trauma (accident) with or without consequences. The one resulting from the traumatic experience Uncertainty leads to
- uneconomical, anxious movements
- Avoidance strategies and reduced everyday activities (Crowds, climbing stairs, hiking or high-risk household chores)
- Muscle breakdown (as a result of inactivity)
- Reduction in coordination and reaction performance
and consequently a further increase in the risk of falling in old age. One develops Fear and Avoidance Spiral With Loss of functional skills, self-confidence and independence.
More likely from those through fears overcautious seniors distinguish the “young at heart” who stand by excessive willingness to take risks and Overestimation of their physical performance distinguish. You lead high-risk senior sports and do repairs, gardening and household chores on ladders yourself. This behavior on the one hand promotes physical and mental fitness and mobility, but on the other hand also includes increased risk a fall in old age.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- - orthopedic surgeons
14
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see - Orthopedists.
Prevention of falls in old age
Avoiding falls is a tightrope walk between excessive caution and risk-taking.
The best possible prevention to avoid a fall in old age involves targeted physical activity and adaptation of the public and private environment to the needs of older people.
1. Prevention in public spaces
- Apartments suitable for senior citizens
- Marking public stairs
- Sufficient lighting
- Snow clearing and spreading on icy roads
- Lowering of curbs
- Avoiding cobblestones
- Signal lights (optical and acoustic)
- Handrails on dangerous roads
- Auxiliary handles on stairs, toilets and raised toilets in public buildings and restaurants
2. Prevention in the household
- Avoiding tripping hazards (objects lying around, smooth, wet floors)
- Sufficient lighting everywhere
- sure-footed footwear inside and outside the home
- Walking aids + stepladders within easy reach
- Raised toilet seat
- Auxiliary handles on stairs, toilets, shower
- Handrails in long hallways
- Stable seating furniture with armrests, senior beds
- Vitamin D intake
- sufficient amount of water to drink (1-2l fluid intake daily)
- Installation of a home emergency call system
- Organization of external support
- Fall prevention exercise program
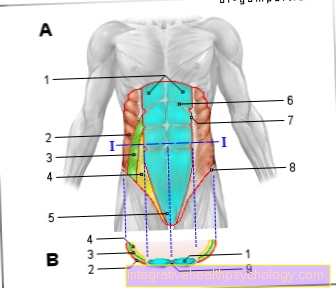
Balance regulation
Keeping your balance means that Center of gravity above a support surface (e.g. the feet) despite the most varied, not always predictable, external influences to control.
1. Controllable, predictable influences consciously performed activities such as lifting one leg to take a step, bending over from a standing position, reaching for a distant object, or climbing a ladder. To this predictable influences can we set / prepare (Anticipation, proactive balance regulation); we shifting controls our weight on one leg to lift the other leg.
2. For unpredictable interference is the reactive balance regulation from of utmost importance. (E.g. misjudging a distance, a push from behind or black ice can throw us off balance.)
The body responds to Interference of balance with different answers:
- spontaneous increase in muscle activity in legs and trunk (to keep the body's center of gravity in balance)
- Compensation steps
- reflex-like grasping for a firm hold
In the elderly come aground slowed down support and defense reflexes this Reactions often delayed. It also succeeds on the ground lack of leg strength and mobility mostly not catching a fall in old age.
Medical basics of balance regulation
In the Controlling Our Balance our brain relies on messages from interlocking equilibrium systems:
- somatosensory system (Tactile information about muscles, tendons and joints)
- vestibular system (Balance organ in the inner ear)
- visual system (Visual inspection of the eyes)
1. Somatosensory system:
By processing the Information from skin, muscles and joint receptors, whose measuring sensors are distributed over the entire body (in addition to the sensory organs eyes, nose, mouth and ears) the somatosensory system enables Perception of pressure, touch, vibration, pain and temperature.
It has tight anatomical and functional interrelationships with the motor system (annoy, Joints, Muscles). All sensations apart from Seen, Smell, Taste and Listen are recorded by the somatosensory system and converted into perceptions. In collaboration with a specific Proportion of the cerebral cortex, whose main task is the Acquisition of movement information is, will three-dimensional structures recognized, Movement information captured and the position of the body, the arm and hand positions in space are determined and perceived without looking.
2. Vestibular system:
The vestibular system consists of the Vestibular organ (Balance organ= Semicircular canals, ventricle and sacculus) im Inner ear. It measures that Spin of the head in all planes, Head tilt and head position to the body and in space, as well as horizontal acceleration (faster walking) and Up and down movements (Jump).
This information is reported to the brain and in different brain regions, especially the Kleinhirn processed, which at Error messages Initiates reactions to control balance. This is followed by another Feedback to the vestibular systemwhether the correction of the balance has been carried out successfully.
3. Visual system:
The visual system includes that eye With Retina and Optic nerve, as well as the associated brain areas. The visual system acts in constant exchange with the other equilibrium systems.
At Disturbances in the somatosensory and vestibular system those affected have to know about the compensate visual system. You look for fixed points with your eyes in everyday life in order to compensate for the restricted balance regulation. This Compensation over the eyes is not efficient enough and hires Balance risk in many everyday activities.
Diagnosis of falls in old age
The Assessment of the individual risk of falling he follows by doctor and physiotherapist:
The investigation begins with a detailed Questioning the patient to the current situation and history. (Taking the anamnesis)
Balance test procedure:
1. Berg balance scale:
In order to be able to assess balance and the risk of falling and to develop a treatment concept based on the test results, the mountain balance scale can be used. It will Balance in different everyday situations examined.
The movement transitions are assessed:
- from lying in the seat
- from seat to stand
- Standing with a large or small support surface (with eyes closed)
- Starting and stopping
- Picking up objects
- Turning around while standing
- One-legged stance
Based on the test results, the assess exact balance deficits and narrow it down into different areas. According to a certain point scheme, the Assess the risk of falling. The Exercise program becomes according to the deficits and put together as individually as possible.
Repeat the test to assess the risk of falling in old age after 3 months performed balance and strength training.
2. Stand-up test:
The time and security that a person needs is assessed by 5x in a row getting up from an ordinary chair with no hands supported. This test should also as a comparison criterion after 3 months of balance and strength training can be used to measure success and to stimulate motivation.
3. Stand tests:
During the standing tests, the following exercises must be performed with different frequencies and repetitions:
- Stand barefoot with feet closed / 10 sec. Stand barefoot when one foot is slightly forward / 10 sec.
- Stand barefoot when both feet are one behind the other (quotes) / 10sec.
- Stand barefoot on one leg / 30sec.
- Stand with your eyes closed
Let us assess whether the person is able to perform the various stance positions and about the Time to hold. A follow-up test should be carried out after 3 months of the exercise program.
4. Strength test:
In the strength tests, the Muscles of the trunk and the legs examined. [link strength training] A Repetition The strength tests should also be used to prevent falls in old age after 3 months to confirm the training success.
Therapy for falls in old age
1. Exercise program to reduce the risk of falls:
In physiotherapy, the Fall prevention (Reduction of the risk of falling) a broad field of work and a increasing challenge represent. Information and advice, as well as the placement of a preventive exercise program can be done either individually or in groups.
Individual treatment is particularly recommended for those affected who already a fall with consequences have suffered, such as patients after Femoral neck fracturethat with osteosynthesis or Hip TEP (artificial hip joint) have been treated. Elderly people due to Hearing-sight or mental impairment are no longer able to Include instructions in the group and implement them should also be supervised in individual treatment.
The exercise program includes Balance exercises, strength training, and reaction training.
2. Fitness training
Fitness training is understood as part of an exercise program to prevent falls in old age
- Brisk walks of 30-45 minutes a day if possible.
- Nordic walking
- Climb stairs
- Doing shopping on foot with the shopping trolley
- Gardening or walking around the garden
- Forest walks on uneven ground
The Exercise program and daily fitness training Like brushing your teeth, it should become a regular routine of everyday life.
- You should use the exercise program that you have learned in individual treatment or in a group, 3 times / week regularlyg, where you can spread the exercises over the day.
- You don't have to do all of the exercises in one workout, you continue to exercise each with a different focus.
- Treat yourself Breaks between the individual exercisesin which you can breathe calmly and deeply. These breaks can be done while sitting, the breathing exercises e.g. in the driver's seat.-photo
- Ever longer and more continuous As you do your exercise program, the easier it will be for you to do it. Initially possible complaints such as Feeling of stiffness in the muscles after the exercises disappear with increasing strength and fitness.
- Take care of your safety! During the balance exercises, a fixed object (armrest, railing) should be within reach. At You should sit down if you feel dizzy. If you have chest pain or shortness of breath during exercise, please contact your doctor.
After approx. 3 month training can a significant reduction in the risk of falling (between 30 and 50% is stated in various studies). Of the Success depends on age and the existing physical limitations.
3. Balance exercises to prevent falls:
- Do the exercise slow and controlled out
- Watch out for even breathing
- Perform each Exercise for 20-30 seconds with 3 repetitions out
- Place them after each exercise approx. 10-20s Take a break
Exercises in bed and standing for balance training

Starting position
Lie on your side on the right in bed
Exercise execution
fast rolling from right to left and back
Starting position
Lie on your back in bed
Exercise execution
Roll to the right or left side and sit on the edge of the bed, the way back is also done on the side
Exercise thumb look


Starting position
Sit on the edge of the bed
Exercise execution
Extend your arm with your thumb raised and move it in different directions (up / down, right / left), gaze fixation exercises: follow the thumb movement with your eyes
Sidebend exercise

Starting position
Sit on the edge of the bed with your feet up (hands are folded behind the head, elbows are pushed outwards)
Exercise execution
Upper body side tilt from right to left (like a clock pendulum)
Exercise rotation

Starting position
Sit on the edge of the bed with your feet up (hands are folded behind the head, elbows are pushed outwards)
Exercise execution
Rotational movements of the head and upper body to the right / left
Exercise on the edge of the bed
Starting position
Sit on the edge of the bed, feet up on the floor
Exercise execution
Shift the weight of the upper body with outstretched arms forwards, backwards and to the side. Increase: the feet do not stand up (be careful when shifting weight forward)

Stand up with a stool

Starting position: Sit on the edge of the bed with your feet up, your hands supported on a stool or chair
Execution of the exercise: getting up from the edge of the bed with support of the arms by shifting weight forward
Exercise Pezziball

Starting position: sitting on a Pezzi ball
Exercise execution: extend arms to the side, shift weight forwards, backwards, to the side
Exercise weight shift


Starting position: upright, hip-width stance
Exercise execution:
- running in place with open / closed eyes
- Turn around on the spot with small steps, eyes open (progression: eyes closed)
- with closed eyes 20-30sec. stand; Toe stand, 20-30sec. hold (increase: close eyes briefly)
- Shift your body weight from behind on your heels, forwards on your toes and back, with your arms in the countermovement (to secure an armchair within reach)
Exercise on one leg

Starting position: upright, hip-width stance
Execution of the exercise: shift body weight to the right / left leg, lift the free foot slightly, hold it for no longer than 30 seconds (armchair!) (Increase: stretch your arms towards the ceiling)
Exercise cross step


Starting position: from a standing position
Execution of the exercise: shift body weight to the right / left leg, spread the free leg outwards, then cross over the other leg, (armchair!)
Pick up exercise object
Starting position: standing upright, a chair nearby to support you
Exercise execution: go into the step position, support with one hand on the chair, with your free hand pick up an object from the floor

Exercise Air Pad

Starting position: status on various documents
Exercise execution: mats, foam cushions, air pad, tilting board, spinning top, mini trampoline, (safety device!) Increase: closed eyes
Also: swings in the rocking chair
Strength training to prevent falls in old age
The special strength training for Fall prevention includes exercises for the leg and core muscles. Many older people have trouble performing exercises on the floor should they rest on Restrict sitting and standing exercises. Still it is necessary to practice getting up from the floor after a fall (link).
The goal of strength training are 3 sets of 8 repetitions with breaks of 1-2 minutes between passes
- Do the exercises evenly slow the effort to exhale is to strive for without holding your breath
- If you're with Exercise weights, these should be chosen so that at Repeat 6,7,8 a feeling of effort occurs
- Dynamic exercises (while moving) are better than static (Holding work against a resistance)
Training the quadriceps muscle

Starting position: sitting upright on a stool, feet hip-width apart
Execution of the exercise: alternately stretch the legs forwards (increase: use a weight cuff)
Abduction training

Starting position: sitting upright on a stool, feet hip-width apart
Execution of the exercise: alternately climb over a high fence with the right / left leg (increase: weight cuff)
Weight-shift training

Starting position: sitting upright on a stool, feet hip-width apart
Execution of the exercise: Shift the upper body to the right / left until one leg is lifted
Training with shifting your weight backwards

Starting position: sitting upright on a stool, feet hip-width apart
Exercise execution: stretch your arms forward, shift your upper body backwards, while continuing to breathe
Training the obliques

Starting position: sitting upright on a stool, feet hip-width apart
Exercise execution: stretch arms to the right / left in front, shift the upper body to the back to the side, while continuing to breathe
Training of the oblique back muscles while sitting

Starting position: sitting on a stool, hands folded behind the neck
Exercise execution: stretch the upper body, push the elbows outwards, shift the upper body in a stretched manner forwards and backwards
Exercise lifting a weight


Starting position: sitting upright on a chair, feet wide open
Execution of the exercise: bend forward, pick up a ball (light weight) from the floor and stretch it up over your head
Getting up from the stool

Starting position: sitting upright on a chair, feet wide open
Exercise execution: press the hands on the chair, lift the buttocks
Stand up with a stool

Starting position: sitting upright on a chair, feet wide open
Exercise execution: get up from the chair with or without supporting your hands, and very slowly sit down again (armchair!)
Exercise secure stance

Starting position: upright, hip-width stand (supported on armchair)
Execution of the exercise: Shift body weight onto one leg, spread the other leg to the side, the leg should be guided to the side (not forwards) and the tip of the foot should not be turned outwards (increase: weight cuff)
Exercise with a weight cuff

Starting position: upright, hip-width stand (supported on armchair)
Exercise execution: Shift body weight onto one leg, lift the free leg forward and stretch it backwards (increase: weight cuff)
Exercise squats

Starting position: Stand with legs slightly open, feet slightly turned outwards
Exercise execution: light squats, opening the thighs outwards, knee joints should not look beyond the feet (armchair! Nearby)
Exercise lunge

Starting position: lunge
Exercise execution: bend the front leg and straighten it again
Exercise squat on the wall

Starting position
Stand against a wall with your legs open
Exercise execution
slowly crouch down, the position 20sec. hold while breathing calmly
Further exercises / Galileo training
Also, walking slowly up and down stairs can help.
In addition, Galileo training can also be useful.
Preventive training

1. Walking training to prevent falls in old age:
- Walk forwards, backwards, sideways, with cross strides
- walk in one line
- Climb over small obstacles
- Walking on uneven ground such as mats, lawn, pasture, forest path, up and down inclines
- emphasizes slow climbing up and down stairs
- Running on the treadmill
2. Walking training for fall prevention with a partner:
-
Partner stands behind the practitioner, guiding the practitioner by tapping on the shoulder from behind, e.g. Tap on both shoulders = forwards, tap right / left = right / left curve, light pull on both shoulders = go backwards, a pat on the back = stop
-
The partner and the practitioner stand opposite each other, the palms of the hands touch each other, the practitioner follows the partner forwards, backwards, and sideways by gently touching the palms
-
The partner and the practitioner stand opposite each other, the practitioner should push the partner away when the palms of the hands contact, the partner gives resistance to the forward movement
- The practitioner stands freely in the room, the partner tries to throw the patient off balance by gently pushing them from different directions, the practitioner defends his position
Important: Backup during the exercises is done by the partner!
3.Reaction training to prevent falls:
- Catch the ball while standing (legs wide open to closed)
- "Goalkeeper training" while standing
- Start walking, stopping, turning around, sitting down and standing up when called
- Change of tempo and direction after music
- Task 1-5
- forward,
- walk backwards,
- sit down, stand up,
- fetch an item and take it away
- Up / down stairs ...) and on command (e.g. task 3) do it as quickly as possible
Getting up after a fall



- Slide on your buttocks to a solid object (armchair, sofa)
- Turn on your knees
- Support yourself with both hands and slowly get up
- Sit on the armchair or sofa (wait until the horror and dizziness are over)
- If it is not possible to get up on your own, possibly call an assistant, use the emergency call