Colon cancer therapy
Note
All information given here is only of a general nature, tumor therapy always belongs in the hands of an experienced oncologist (tumor specialist)!
definition
The treatment of the patient requires intensive cooperation between the specialist departments of surgery, internal medicine, radiation therapy and pain therapy. During therapy, the previous tumor staging (assessment of the extent of the tumor) is used as an essential decision-making aid. For each tumor stage there are corresponding therapeutic guidelines that are taken into account.
Read more on the topic: Stages of colon cancer and their prognosis

What are the treatment options?
As one of the most common cancers in adults, colorectal cancer therapy is a major topic in medical research and is constantly being improved by new discoveries. The treatment of colon cancer is based on three pillars: the surgical removal of the tumor, chemotherapy and radiation (which is only used when the rectum is affected), which can be used alone or in combination.
Which method or combination is ultimately used for the individual patient is usually discussed in a panel of experts, the clinicopathological conference. Surgeons, radiologists, pathologists and oncologists advise each other on the basis of the patient's findings, the current guidelines and the current status of medical research.
A distinction is made between two approaches to the therapeutic approach: On the one hand, there is the curative approach, which aims at complete healing. This is to be distinguished from the palliative procedure, in which the alleviation of the tumor complaints is in the foreground due to the low healing prospects, without the direct aim of healing.
Types of therapy
Operative therapy
Surgical therapy is the most important pillar of intestinal cancer therapy, because in the best case it allows total removal of the tumor and thus healing. Care is taken to remove the entire tumor mass as far as possible, including a safe distance from healthy tissue so that no tumor cells remain. Lymph nodes into which the tumor may have spread will also be removed.
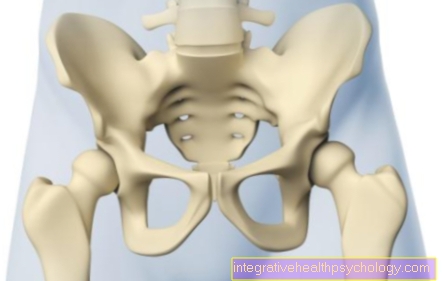
The extent of the operation depends on the location of the tumor, with only the affected section of the intestine being removed as a rule. Then the two remaining ends of the intestine are sewn together again, which is called Anastomosis referred to as. Rectal carcinoma (cancer of the rectum) is a special situation, since depending on the location of the tumor, the sphincter may also have to be removed, which may make it necessary to create an artificial intestinal outlet (anus praeter).
In some high-risk patients, it is advisable to completely remove the bowel (colectomy). Patients with longstanding ulcerative colitis and patients with familial poliposis coli are eligible. During this prophylactic operation, the sphincter muscle is always preserved so that stool continence is preserved. To determine the memory function of the rectum (rectum), a reservoir is formed from the attached piece of small intestine.
Read more on the subject at: Remove colon
All of these interventions can be carried out by opening the abdominal cavity through a large abdominal incision, or laparoscopically, whereby a camera and instruments are inserted into the abdominal cavity through several small incisions. Surgery can also help in patients who have no more prospects of a cure due to an advanced disease, for example by removing or bridging intestinal sections that have become overgrown by the tumor in order to save the patient unnecessary suffering.
Read more on the subject at: OP for colon cancer
chemotherapy
One pillar of colon cancer therapy is chemotherapy. Here, different preparations are usually used in combination with one another, which aim to kill the rapidly dividing tumor cells (cytostatics). Chemotherapy can be used in addition to operations or used alone if an operation is no longer possible or is not desired.
When combined, chemotherapy can be carried out as so-called neoadjuvant chemotherapy before the operation. This is intended to reduce the tumor mass in order to return inoperable tumors to an operable stage or to reduce the extent of the operation. In addition, neoadjuvant chemotherapy helps to reduce the risk of the tumor recurring later.
Chemotherapy can also be used after an operation, which is then referred to as adjuvant. The aim is to combat the cancer cells that still remain in the body and to treat small micrometastases that may have already formed but are not yet visible in the imaging.
Most chemotherapeutic agents are directed against rapidly dividing cells in a non-specific manner and therefore often have unpleasant side effects, as they also affect other rapidly dividing tissues in addition to the cancer cells. Common side effects include nausea, vomiting, diarrhea, loss of hair and reduced production of blood cells, which leads to anemia and a tendency to become infected, as the immune system is also weakened.
Chemotherapy is usually carried out on an outpatient basis so that no inpatient stay is necessary. Depending on the therapy regimen, the drugs are administered via the vein on one or two consecutive days. This procedure is usually repeated every 14 days, which is known as a cycle that is run through several times.
Read more on the subject at: Chemotherapy for colon cancer
radiotherapy
For tumors of the rectum, radiation therapy is still a possible treatment option. Here, high-energy rays, which are either secreted by radioactive substances or generated by special devices, are used to destroy tumor cells. This is done with the highest possible precision so that the tumor receives the majority of the harmful radiation dose.
Unfortunately, it cannot be completely avoided that surrounding tissue is also affected, which is why inflammation, nerve damage and thrombosis can occur in the adjacent vessels.
Radiation therapy, like chemotherapy, can also be used adjuvantly or neoadjuvantly. In the case of intestinal tumors above the rectum, radiation therapy is out of the question, as the position of the tumor inevitably varies due to bowel movements in the abdomen and therefore targeted radiation is not possible.
Read more on the subject at:
- radiotherapy
- Radiation therapy for colon cancer
Immunotherapy
Antibodies (the body's own defense substances) are used here, which are directed against various structures of the cancer cell and thus prevent them from growing. These antibodies are given in combination with cytostatics.
If curative therapy can no longer take place, palliative therapy for colon cancer is usually considered. This is primarily aimed at alleviating the symptoms and improving the patient's quality of life.
When is which method used?
The choice of therapy method depends mainly on the stage in which the disease is present. However, other factors also play a role, such as the age of the patient, any secondary illnesses, as well as the patient's ideas and wishes.
In the early stages without metastasis to the lymph nodes or other organs, surgery alone may be enough to treat the disease. If the tumor has already grown into deeper layers of the intestinal wall or has metastases in lymph nodes or other organs, subsequent chemotherapy is recommended 4 to 6 weeks after the operation. Even in tumors that are no longer operable, chemotherapy can delay the growth of the tumor.
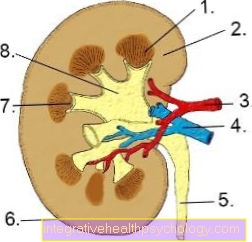
Therapy of metastases
Colon cancer is one of the few tumor diseases in which curative therapy is still possible even if metastases are present in the liver and lungs, provided that the metastasis has not progressed too far. The number, size and location of the liver or lung metastases are important here. If there are too many, too large or inoperable metastases, treatment can no longer be treated with a curative intention. In addition, the lungs or liver must be in a sufficiently good condition to be able to compensate for the loss of the healthy parts of the organs that were removed with the metastases.
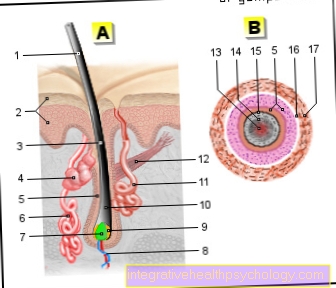
The method of choice here is surgical removal of the metastasis (s), but other methods are also used. One example is radiofrequency ablation, in which liver metastases can be destroyed by heat with the aid of high-frequency electrical surges through a probe. In any case, after a successful operation, adjuvant chemotherapy should also be carried out to reduce the risk of further metastases.
The regular follow-up examinations should also be taken very seriously in order to be able to take therapeutic measures at an early stage if metastases occur.
Read more on the subject at: Metastases in colon cancer
How can pain be treated?
Nowadays, long-term pain therapy with one or more drugs is recommended for tumor-related pain. The therapy is individually tailored to the patient and aims to achieve lasting freedom from pain for the patient. It is therefore important to take the medication at regular intervals in order to achieve an even effective level.
This so-called basic medication is supplemented by a pain reliever that is taken as required, which can be taken acutely in the event of sudden severe pain, known as tumor breakthrough pain. In pain therapy, according to the WHO (World Health Organization) grading scheme, mild painkillers are used first. If these are not enough to control the pain, stronger pain relievers may be used until a combination and dose is found that can successfully control the pain.
In addition to the classic painkillers, other drugs can also be used as support, such as antidepressants (support the effect of painkillers) or anticonvulsant drugs (Anticonvulsants), which also have pain relieving properties.
Furthermore, possible side effects of some drugs must be taken into account. Especially when taking morphine preparations, constipation often occurs, which must be treated with laxative measures.
Read more on the subject at: Colon cancer pain
What complications do colon cancer therapies have?
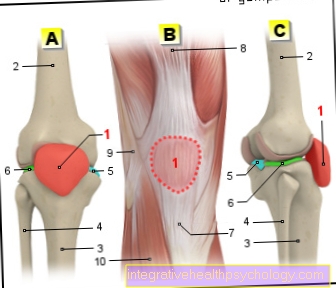
The most common complication of colon cancer is sudden (acute) bowel obstruction (Ileus), which is caused by a severe narrowing of the intestine by the tumor. Therapeutically, the intestinal passage has to be quickly restored surgically.
Another complication is the breakthrough of the tumor through the intestinal wall (perforation). As a result, bacteria can escape into the abdominal cavity, which in turn leads to life-threatening brook fur inflammation (Peritonitis) leads. Urgent surgical procedures are necessary for this complication as well.
Less common complications result from the tumor growing into neighboring organs. In some cases this results in tubular ducts between two hollow organs, the so-called fistulas, e.g. into the bladder or uterus.
Side effects of therapy for colon cancer
Depending on the type of therapy, different side effects can arise in the treatment of colon cancer. For example, the operation can lead to major losses of sections of the intestine with subsequent digestive problems or the creation of an artificial anus.
When treated with chemotherapy, nausea, vomiting, loss of appetite and hair loss, as well as increased susceptibility to infections due to the drop in white blood cells (Leukocytes), Anemia (lack of red blood cells) and increased tendency to bleed (lack of blood platelets).
However, the side effects do not occur in every patient or to the same extent and can be very different.
How long does treatment for colon cancer take?
Depending on the type of cancer, the stage of the cancer, the condition and age of the patient, and the type of therapy, the duration of the treatment can vary. The cancer is usually removed surgically first. Depending on the stage of the cancer, chemotherapy can then follow after the tumor has been removed. This can vary greatly in duration depending on the number of cycles.
For cancer of the rectum (Rectal cancer) In addition to the operation, radiation or combined radiation and chemotherapy may be necessary, whereby the exact duration of these treatments is determined individually and cannot be generalized.
Follow-up care after treatment for colorectal cancer
Since 30% of colon cancer diseases lead to local tumor outbreaks in the following 2 years (Relapses), it is important to create a consistent aftercare plan.
Quarterly checks for hidden blood in the stool (haemoccult tests) are carried out and the tumor markers are checked. Hidden blood in the stool and a rise in tumor markers are suspicious for tumor recurrence.
An ultrasound (Sonography) of the liver and a chest x-ray (Chest x-ray) are used to detect metastases in the liver and lungs.
A colonoscopy (Colonoscopy) should be performed 6 and 12 months after primary therapy (surgery), then every 3 years.
Guidelines
Colon cancer therapy differs depending on the stage of the cancer, the age of the patient and other circumstances.
In stages I-III the therapeutic intention is curative (curative). The operation of the cancerous growth (tumor) represents a central treatment step. In the very early stage (stage I), the operation of the cancer alone is often sufficient. In more advanced stages, the operation is followed by so-called chemotherapy. This chemotherapy can consist of different drugs (chemotherapeutic agents) and aims at a flare-up (Relapse) to prevent cancer and to combat possible colonization.
Depending on the type of tumor, the treatment of colorectal cancer can be expanded with so-called antibody therapy. In some patients, chemotherapy is also required before the operation (neoadjuvant) very helpful. This is supposed to curb the growth of the cancer and shrink it so that the success of the operation can be increased.
In the case of cancer of the rectum (rectum) the tumor can also be treated with radiation therapy or combined radiation / chemotherapy.
Therapy of the IV stage of cancer, which is caused by remote settlements (Metastases) of the tumor can either be curative (curative) with removal of the mother cancer and the colonization (Metastases) or be treated with additional chemotherapy, or, if healing is no longer possible, through pain-relieving forms of therapy (surgery, drug therapy).