Diverticulitis
Synonyms in a broader sense
- Diverticulosis
- Inflammation of the colon
English: diverticulitis
Definition of diverticulitis
Diverticula are protuberances in the intestinal wall in weak muscles. They cannot empty themselves because they have no muscles like the rest of the way Intestines. If such a protuberance is inflamed, it is called diverticulitis. One Diverticulitis the training always goes first Diverticula (Diverticulosis) ahead.

introduction
Diverticulum are protrusions of the intestinal wall. They don't consist of birth but develop over the years.
A preferred place to develop such protuberances is the Large intestine.
80 percent of diverticula occur in the sigma. The sigma is an S-shaped part of the large intestine. If the diverticula become inflamed, one speaks of diverticulitis. This happens about 25% of the time. A low-fiber diet has a negative influence on the development of these diverticula.
A healthy eating with lots of fruit, vegetables and whole grain products would be desirable. This not only stimulates digestion, but also binds bile acids. This type of diet is therefore also recommended for people with high cholesterol levels, since cholesterol can also be excreted with the bile acid.
Inflammation arise following through Clogging of feces. In addition to pain, the symptoms of diverticulitis also include defecation disorders. Diverticula are diagnosed in the Ultrasonic or as an incidental finding of a colonoscopy.
Inflamed diverticula are also recognized on ultrasound based on their thickened, inflamed wall. Of course, the symptoms that bring the patient to the doctor also play an important role.
These inflammations are treated with the help of Antibiotics. A surgery is usually only necessary for a breakthrough into the abdominal cavity.
Medical guidelines
In the medical guidelines the current scientific status about the causes and development of the disease, the typical symptoms and the most effective diagnostics including the safest, best and most modern therapy should be presented.
The guidelines serve the doctors as orientation and a central theme in diagnosis and therapy. However, there is no regulated obligation as a doctor to adhere to the recommendations.
The guidelines for diverticular disease / diverticulitis are expected to be finalized in December 2013.
Frequency (epidemiology)
Diverticulosis is a disease that occurs low fiber diet is due. The older people get, the more likely they are to develop such protrusions.
Initially, the diverticula are asymptomatic. Over time, however, symptomatic diverticulitis tends to develop if the diverticulum becomes inflamed.
In two-thirds of all cases, the diverticula form in the sigmoid colon (S-shaped part of the large intestine) and are usually only pseudodiverticula. They come more rarely in the Coecum (appendix in the medical sense, i.e. the beginning of the large intestine), but then they are mostly congenital true diverticula.
People in developed countries are more likely to develop diverticulitis than people in developing countries. The reason is the low-fiber diet that prevails in industrialized nations.
Are colonic diverticula (colon = Large intestine) present, 75 percent remain asymptomatic. Of the other 25 percent, 25 percent develop bleeding (about a third massive bleeding) and 75 percent develop diverticulitis.
Most of it remains straightforward. Just under a quarter then struggled with the symptoms.
Causes of Diverticulitis
Some of the causes of diverticula include, for example high pressure in the intestine constipation or weak muscles of the intestinal walls with age.
If stool builds up in these diverticula, it can cause inflammation. The stool that collects there is difficult to get out of the protuberances, as there is no peristalsis here. (peristalsis = Movement of the intestine by the wall muscles in order to transport the stool or chyme from the stomach to the anus.) This is how bacteria penetrate the intestinal wall. The inflammation keeps coming back and varies in severity.
Symptoms / complaints
About 80 percent of the cases are symptom-free diverticulosis. Only about 20 percent become symptomatic.
A distinction is made here between the symptoms
- a sigmoid diverticutitis (sigma = s-shaped part of the large intestine) and
- a coecum diverticulitis
Sigmoid diverticulitis (80%)
- spontaneous pain (usually left lower abdomen)
- irregular bowel movements (alternation between constipation and diarrhea)
- Possibly a pressure sensitive roller can be felt
- Blood count: inflammation parameters (ESR and CRP value) high
- fever
Coecum diverticulitis (20%)
- Pain in the right lower abdomen
The bowel evacuation disorders in diverticulitis are due to the swollen intestinal walls, which result in a narrowed intestinal lumen. If the inflammation keeps coming back, larger accumulations of pus (abscess) can occur in the small pelvis. Fever and increased inflammation parameters are very unspecific because they occur with any type of inflammation. Nevertheless, they are among the most common symptoms and can provide clues.
You might also be interested in: Abscess in the intestine
Signs of diverticulitis
The three classic signs of existing diverticulitis are:
- pain that occurs relatively suddenlywhich in most cases can be felt in the right lower abdomen,
- a increased body temperature such as
- a rise of white blood cells (Leukocytosis) and the Inflammation values (CRP) in the blood count.
The abdominal pain may radiate into the back and be caused by a spatially limited defense tension of the abdominal muscles (local peritonitis) in the painful abdominal area. However, the abdominal pain does not always necessarily have to be in the right lower abdomen (please refer: Lower abdominal pain), so that depending on the affected part of the colon, other abdominal regions can also become painful.
Other signs that can accompany this classic triad of symptoms of diverticulitis include nausea and vomiting, constipation or diarrhea as well as mucus or pus in the stool and difficult urination (dysuria).
Pain associated with diverticulitis
Depending on Diverticulitis severity can different forms of pain and other symptoms appear.
Generally found often dull, even pain in the left lower abdomenwhich in medical terminology as "Left side appendicitis“Are called because they dem Painful character of appendicitis (appendicitis), which usually occurs in the right lower abdomen, can resemble on the left. The pain does not necessarily have to occur in the left lower abdomen, but can in principle affect the whole Large intestine concern, which is rarely found.
In addition, the Diverticulitis also like " Appendicitis of the Elderly“Because it usually occurs in older people and has a lot in common with the symptoms of appendicitis (appendicitis).
Some of the pain can also radiate to the back.
If an intestinal perforation has already occurred in the area of an intestinal wall protuberance (diverticulum), even stronger, very sudden pain, accompanied by signs of inflammation such as Show fever, nausea, and vomiting.
Diagnosis of diverticulitis

Asymptomatic diverticulitis is usually only an incidental finding of a colonoscopy.
An inflammation of the diverticulum, however, can be based on:
- of symptoms / complaints
- the blood count (laboratory values)
- Ultrasound or
- roentgen
put.
The diverticula can be visualized in the ultrasound. If they are ignited, the wall is thickened. The diverticula can also be seen in computed tomography. With the help of contrast media, thickened walls can also be seen here. In very bad cases it may also be necessary to do an MRI of the abdomen.
A breakthrough in the inflamed protuberances could be recognized in the X-ray image by the so-called "free air". Free air is black. It is created by the leakage of air from the broken intestinal loops. The still prevailing peristalsis (movement of the bowel) pushes air out of the bowel.
This air always accumulates at the top. Depending on the patient's position during the X-ray, you can assess free air at certain points. Free air must be distinguished from air in the intestinal loops.
Read more on the topic: Ultrasound of the abdomen
Stages
To date, there is no uniform staging of diverticulitis. However, the is suitable for everyday clinical practice Classification according to Hansen and Stock. The findings of the clinical examination, the Colonoscopy or des Colon contrast enema and the Computed Tomography of the abdomen. The classification serves as the basis for stage-appropriate therapy.
- The Stage 0 denotes the Diverticulosis, so one Wall protuberancebut without inflammation. This stage is accordingly asymptomatic.
- The Stage 1 denotes an acute one uncomplicated Diverticulitis. This stage goes with Pain in the lower abdomen and maybe fever hand in hand. However, there is no risk of one Intestinal perforation and can usually outpatient be treated.
- The Stage 2 denotes the acute complicated Diverticulitis. This stage is further divided into types 2a, 2 B and 2c. Stage 2a describes a Peridiverticulitis. This means the inflammation is confined to the diverticulum. There is a local one Tenderness, a light one Defense tension in the area of inflammation, fever and a palpable resistance. in the Stage 2b the diverticulum has become one abscess, one fistula or a covered one perforation further developed. This means that the intestine is perforated in the affected area, but the inflammation has not yet spread to the abdomen. This stage goes with fever, one Peritonism and one Intestinal atony hand in hand. The Stage 2c denotes the free perforation of the diverticulum. The intestine is perforated and the contents of the intestine are emptied into the free abdominal cavity. This stage goes with the symptom of one acute abdomen hand in hand and is one life-threatening Situation that must be treated surgically as quickly as possible.
- The Stage 3 describes a chronic recurrent diverticulitis. This goes with recurring Lower abdominal pain, constipation (Constipation) and one Subileus hand in hand.
Hansen Stock
The classification according to Hansen and Stock serves to classify diverticulitis into three clinical stages and provides the basis for stage-adapted therapy.
This classification is based on the synopsis of the clinical examination, colonoscopy, abdominal CT scan and contrast enema examination of the colon.
Stage 0: There is only one Diverticulosis (multiple wall protuberances in the colon wall) without signs of inflammation, which does not cause any symptoms.
Stage 1: There is acute, uncomplicated diverticulitis without the risk of perforation, which can lead to pain in the lower abdomen and possibly fever.
Stage 2: There is an acute, complicated diverticulitis, which is divided into three sub-forms and carries the risk of perforation.
Stage 2a: Phlegmonous diverticulitis or peridiverticulitis (Inflammation of the immediate area around the diverticulum), which leads to local pressure pain and local defensive tension in the form of palpable resistance in the lower abdomen with accompanying fever.
Stage 2b: Abscessed diverticulitis is present here, often in a covered, perforated state, which is similar to the Stage 2a locally to a defensive tension / pressure pain, fever and also to a loss of tone of the intestinal muscles (Intestinal paralysis) in the affected part of the colon.
Stage 2c: There is a free intestinal breakthrough. Symptoms are those of an acute abdomen with diffuse peritonitis.
Stage 3: Here there is chronic, recurring diverticulitis, which can recurrently lead to lower abdominal pain and constipation symptoms, which can possibly end in a preliminary stage of an intestinal obstruction.
Classification
For one, between the symptomless Diverticulosis and the symptomatic Diverticulitis distinguished. Diverticulosis is a protrusion of the wall of the intestine and is not inflamed. it is very frequently and affects approx. 60% of all people> 70 years of age in the industrialized countries. Diverticular disease, also called symptomatic diverticulitis, is the inflammation of this wall protuberance and is again divided into stages depending on the severity of the inflammation.
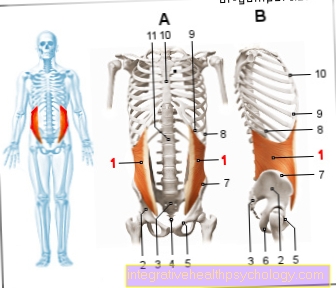
Furthermore, so-called Pseudodiverticulum differ from true diverticula. The pseudodiverticula (= false diverticulum) are in 2/3 of the cases in Sigma localized (lower part of the intestine). They arise from vascular gaps in the muscular intestinal wall and simply refer to a protrusion of the intestinal mucosa. The real diverticula, on the other hand, are very many less common and are often found in the area of the Coecum (Transition from Small intestine to Large intestine). This is an outgrowth of all layers of the intestinal wall.
Complications
Such an inflamed diverticulum can break open and the inflammation can spread to the abdominal cavity. Followed by peritonitis, this is probably the most serious complication and must be operated on immediately.
It can also too
- Bleeding
- Constipation or even
- Blood poisoning
come.
Also the training of Fistulas is possible. Fistulas are connections between two loops of intestine. However, these fistulas can also develop between the intestine and other organs. Fistulas between the intestine and the urinary bladder are also conceivable and sometimes occur. This is particularly common with Crohn's disease the case.
therapy

With a first, uncomplicated flare-up of diverticulitis, one goes first conservative, non-operational way. This usually consists of an inpatient stay, Food leave, venous administration of fluids (infusion) and Antibiotics. Until complete healing, unlike the Diverticulosis, on a low fiber diet be respected.
For crampy abdominal pain you can Antispasmodics be taken, e.g. Buscopan®. To Pain therapy can also Metamizole, Pethidine or Buprenorphine be used. Morphine itself should not be used for diverticulitis due to the increase in pressure in the intestine. To 65% this therapy is already sufficient for diverticulitis. Is after 24-48 hours If there is no improvement in this, surgical therapy can be considered.
If an inflammatory flare-up (diverticulitis) occurs for the second time, it is one planned operation to think about after the inflammation has healed. The operation is designed to reduce the risk of complications in the event of further attacks. Especially with boys Patient (under 40) and immunosuppressed risk patients there is a tendency to an early intervention due to the high probability of recurrence. In other patients, a third or fourth attack may pass before deciding to have an operation.
The highly inflamed intestinal sections can be surgically removed and the healthy parts can be joined together again: End-to-end connection (Anastomosis). Different surgical techniques are used depending on the extent and location of the defect. This is usually the case with uncomplicated diverticulitis Keyhole technology (laparoscopy) applied. Depending on the circumstances and the patient, the open abdominal surgery with a larger incision would be an advantage.
In case of a perforation (Rupture of a diverticulum, rupture of the intestine), Constrictions (Stenoses), Intestinal obstruction (Ileus), Abscesses (encapsulated collection of pus), or Fistulas (tubular connection) with and without Peritonitis (Peritonitis) immediate or prompt surgical therapy is recommended. When the diverticulum is perforated, a artificial anus (Colostomy) appropriate (Hartmann operation). This means that the upper section of the intestine is connected to the abdominal wall. The stool is then passed through an artificial hole in the abdominal wall into a bag attached to the outside of the abdomen. The lower section of the intestine, which lies further towards the anus, is initially closed. If the inflammation in the abdominal cavity has receded, both ends of the intestine can move back at the earliest 12-16 weeks reconnected to each other.
In particularly severe cases of pollution of the abdominal cavity, a programmed Abdominal irrigation (Abdominal lavage) to be required.
If a patient is not in a sufficiently good general condition, an abscess or perforation is a problem Ultrasound or CT-controlled drainage (drainage) of the inflammatory secretion possible. To 7-10 days In the better condition of the patient, the affected part of the colon can then be removed. Diverticulitis is a trigger sepsis (Blood poisoning), stabilization of the patient is the main priority. Surgical rehabilitation of the source of inflammation will follow as soon as possible. At Bleeding the extent must first be determined. Depending on the need, one can act on wait Emergency colonoscopy with hemostatic measures up to open emergency operating room be performed.
Appropriate nutrition should be ensured in all phases of the disease.
Antibiotics for diverticulitis
In addition to a strict diet and pain reliever drugs Antibiotics used. These are intended for the inflammation kill responsible germs. Since the exact germs can usually not be determined Broad spectrum antibiotics used. These are antibiotics that work against numerous different germs.In doing so, however, they have to meet certain requirements, as a special spectrum of germs can be found in the intestine. So the therapy must always be against both Anaerobes, as well as against gram negative bacteria be effective. This requires a certain combination of different antibiotics.
For example Metronidazole and a Fluoroquinolone (e.g. Ciprofloxacin) used. Metronidazole (Clont®) is only effective against gram-negative anaerobes, the fluoroquinolones are effective against gram-negative aerobes. This covers a wide range of possible pathogens. However, since it does not kill all germs, this combination is only used in the mild form of diverticulitis. Another possibility is that Amoxicillin with clavulanic acid or Ampicillin with sulbactam. These are each combinations of one penicillin with a Beta-lactamase inhibitors. This combination works against aerobes and anaerobes and is used in moderate diverticulitis, Stage 2a or 2 B used.
In the case of a stage 2c, so an open perforation in the abdominal cavity 3-way combinations out Ampicillin, Metronidazole and Ciprofloxacin used to capture the largest possible spectrum of germs. Also Imipenem or Meropenem are effective against aerobes and anaerobes and are considered to be in stage 2c Reserve antibitotic used. They inhibit the cell wall synthesis of the bacteria and are beta-lactamase-proof. However, their enteral absorption is very poor. Because of this, these antibiotics can only be over that vein administered.
Diet for diverticulitis

Nothing should be eaten during acute inflammation. If necessary, the calorie and nutritional requirements are supplemented via the vein as an infusion (parenteral nutrition). If the symptoms and signs of inflammation improve, a slow diet with tea, with or without sugar, broth or soup, and rusks can take place. The next step is liquid-passed food and white bread.
A low-fiber diet then applies for the next 1-2 weeks. This includes products made from white flour such as light-colored pasta, white bread, semolina, pudding powder, mashed potatoes, cooked vegetables (no raw vegetables), fruit without peel or seeds. Low-fat, boiled, steamed foods and foods prepared on aluminum foil are usually better tolerated during the inflammatory phases.
After the diverticulitis has completely healed, a basic diet is over high fiber Products advisable. This stimulates the work of the intestine and prevents constipation through its swelling properties. Lots of fiber is in fruit and raw vegetables, Legumes and Grain contain. 3-4 servings fresh fruit, 2 servings Vegetables as well 3-4 slices of whole grain bread or others whole grain products should be included in the daily menu. Nuts should be chopped up well and fruit kernels should not be eaten at all, as in the worst case these can settle in the diverticula and lead to inflammation. Since fiber swells, care must be taken to ensure adequate hydration. At least 1.5 - 2 liters should be drunk daily in order to be able to use the full function of the fiber.
alcohol
In the Development of diverticulitis hire increasing age, little physical exercise as well as a high meat consumption possible risk factors. alcohol however is currently Not held responsible for the development of diverticulitis as a special risk factor. However, a permanent overconsumption of alcoholic beverages (chronic alcohol abuse) the Attack the intestinal mucosa and harm.
Many patients also wonder what to do with drinking alcohol after a diagnosis of diverticulitis.
In addition to well-tolerated, light and high-fiber diet (legumes, whole grain products, unpeeled grains and unpeeled fruit), the Avoiding coffee, caffeinated drinks and alcohol an important therapeutic measure for diverticulitis.
Avoiding a lot of food that is difficult to digest, as well as alcohol, often describes an improvement in symptoms after a few days, as the bowel can calm down and the inflammation can heal.
prophylaxis
Prophylaxis can be used to the extent that one eats foods rich in fiber.
A high-fiber diet is achieved by consuming a lot of fruits, vegetables, whole grains, legumes and sunflower seeds. Brown rice also falls into this category. A healthy and balanced diet also includes sufficient fluid intake. An adult should drink around two to three liters per day.
Unfortunately, the instability of the muscular intestinal wall with increasing age cannot be influenced.
forecast
Acute diverticulitis can be treated well with medication and usually resolves quickly. Unfortunately, the cause, namely the formation of diverticula in general, cannot be dealt with with medication.
In general, it can be said that the age of the first illness plays a role. The sooner the diverticula cause symptoms, the sooner an operation will be needed. Even if inflammation occurs more frequently, the intestinal lumen (intestinal tube) narrows and operations are necessary. Like all other operations, this operation is of course associated with certain risks. Infection, bleeding or injury to neighboring organs are possible.