Calf pain
introduction
The calf is a section of the lower leg that extends from the hollow of the knee to the heel and includes the rear lower leg muscles. This area is involved in many body movements. For those affected, calf pain is very uncomfortable pulling or stabbing pain that can occur with different natural movements and increased physical activity or at rest. In the case of severe pain, the person affected can be significantly restricted in everyday activities, which means a loss of quality of life.

The possible causes
In order to effectively investigate the cause, it is important to first differentiate precisely between the type of pain, the duration and the time it occurs.
In the case of acute and irregular calf pain, the symptoms of which improve after a few minutes, the muscular causes are usually responsible for the calf pain.This can be a muscle strain or a torn muscle fiber.
Muscle cramps can result from intense physical activity such as jogging or from excessive alcohol consumption. This shifts the body's electrolyte balance and, above all, a deficiency in the mineral magnesium can quickly trigger muscle cramps.
Regular and long-lasting calf cramps can be caused by overloading the muscles, by a high level of physical activity or by anatomical misalignments of the foot that place increased stress on the muscles.
Chronic nerve damage is rarely the cause of calf pain. This can be caused by compression of a spinal nerve root due to a herniated disc in the lumbar spine or degenerative processes in the spine. In this case, symptoms such as sensory disorders and reduced strength often occur.
A special case of load-dependent pain is the so-called lodge syndrome. There is always painful pulling in the calf, which is accompanied by sensory disorders such as tingling or numbness as well as tension and swelling of the affected area. Above all, competitive athletes and bodybuilders are affected, in whom the muscle volume increases significantly in a very short time.
Finally, when investigating the cause, the possibility of a circulatory disorder in the vessels of the lower leg should not be disregarded. This can be, for example, a peripheral arterial occlusive disease or venous congestion or inflammation.
PAD as the cause
PAOD is the abbreviation for the so-called peripheral arterial occlusive disease and describes a circulatory disorder in the legs.
Usually the cause of PAD is arteriosclerosis. The calcium deposits in the vessels are then so pronounced that no longer enough blood can penetrate into the lower areas of the leg. This results in a reduced blood flow, which causes a painful "ischemic pain". These pains occur particularly easily during physical exertion. Those affected then have to pause for a moment to allow enough blood to flow through the leg again.
The resulting pain is a special characteristic of being resistant to painkillers. Unfortunately, there is actually no treatment option for PAD.
For more information, read on here: PAOD.
Thrombosis as the cause
If the cause of the calf pain can be traced back to a vascular disease in the form of a deep vein thrombosis, therapy should be given as soon as possible in order to minimize the consequences of the disease. First, the administration of a blood-thinning agent such as aspirin is indicated, which inhibits blood clotting and facilitates the flow of blood around the constriction. So-called thrombolytics are used to specifically dissolve fresh thrombi.
Alternatively, a thrombus in the groin area can be surgically removed, for example. This procedure is called a thrombectomy.
After the thrombosis has been resolved with medication or removed surgically, prophylaxis is necessary. For this you can use drugs like Marcumar® or NOAK's. These inhibit proteins that are necessary for blood clotting.
Read more about the topic here: deep vein thrombosis.
The torn muscle fiber as the cause
A torn calf muscle is one of the most common sports injuries. The reason for this is an overload of the muscles; often as a result of insufficient warming of the muscles or as a result of overestimating oneself when coping with stress.
As already mentioned, the muscle fiber tear is one of the typical sports injuries and is accompanied by an acute shooting pain when the fiber is torn. Usually the existing action is canceled and the person concerned has to adopt a protective posture. The ruptured muscle fiber can be accompanied by bleeding of the muscle, which then shows up as a bruise.
The most effective treatment consists of the so-called PECH scheme (pausing, ice cooling, compression, (still) holding) and a subsequent break from exercise.
Find out more about the topic here: Torn muscle fiber
The calf strain as the cause
In contrast to a muscle fiber tear, the strain is not a real severing of muscle fibers, but merely an overstretching of the muscle fibers. The strained calf is also one of the common sports "injuries" and usually results from insufficient warming before sports or from a highly stressful movement during sports.
With a strained calf, pain also sets in suddenly, but it subsides in the following minutes. However, depending on the extent of the strain, sport can be resumed after a short break. Furthermore, a strain almost never leads to bleeding in the muscles, so that no hematoma (bruise) occurs.
More information on the topic Muscle strain you'll find here:
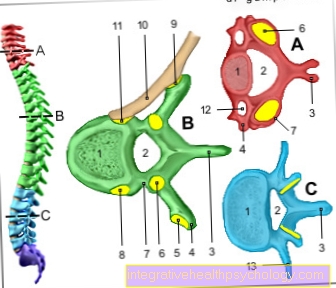
The L5 / S1 herniated disc as the cause
The herniated disc is one of the most common neurological diseases in our society and is usually a disease later in life. A herniated disc is also usually caused by a heavy load, in which the core of the disc presses on an outgoing nerve. T
Sensitivity disorders in so-called dermatomes are typical of a herniated disc. The corresponding dermatome for the outgoing nerves of segments L5 and S1 extends over the calf of the person concerned. The sensitivity disturbances in the calf area often manifest themselves in the form of pain that cannot really be controlled. Usually numbness or a tingling sensation are also associated.
Read on here: Herniated disc L5 / S1.
The Baker's cyst as the cause
A Baker's cyst is a bulging of the knee joint capsule towards the back of the knee. The cause of the cyst is usually an increased fluid production within the knee joint capsule. The causes for this can in turn be very diverse. Usually the reasons are inflammation, but there are also many known cases where the cause is not exactly known.
The pain that occurs with Baker's cysts is more likely to be located in the hollow of the knee than in the calf and occurs particularly during exercise or with bent knees. However, treating a Baker's cyst is quite simple, so the pain can be resolved quickly.
You can find more information here: The Baker's cyst
The compression stocking as the cause
The compression stocking is a form of therapy that is often used for people with so-called edema. So for people with water retention in the lower legs or for people whose blood vessels in the legs show flow disorders.
However, a common problem when buying stockings is that their size is not measured precisely, so patients are also provided with stockings that are too small or unsuitable, which can cause calf pain.
Another possibility is that patients are not putting their stockings on correctly. For example, do not pull them up completely or something similar. This also causes the stockings to sit incorrectly, which can lead to calf pain.
The symptoms
Symptoms vary depending on the underlying cause.
In the case of peripheral arterial occlusive disease (PAD), in addition to calf pain, which increases with exercise, symptoms such as wound healing disorders on the foot or ankle can be observed. A pulse is often no longer palpable here and the legs are cold and pale. With a PAD, several stages of the disease can be differentiated. From stage 2 the patient has pain when walking.
In the case of a thrombosis, on the other hand, the blood literally reaches the legs, but cannot flow back. The thrombosis clogs the vessels and hinders or slows down the reflux. Because of this, the leg swells. In addition, there is a bluish or reddish discoloration, overheating, a feeling of heaviness or tension and pain. Symptoms often improve when lying down.
In addition to the occlusion of the deep leg veins, inflammation of the superficial leg veins, a so-called thrombophlebitis, can occur, which causes severe pain in the calf. Varicose veins or even joint inflammation can also radiate into the calves and cause pain.
Overloading during sporting activities can also lead to hardening. This is due to the acidification of the muscles. However, this is a temporary symptom.
The muscle hardening as a symptom
Muscle hardening of the calf muscles usually results from prolonged overloading of the calf muscles, for example when running over a long distance.
The muscle hardening occurs with sudden onset of pain, which often only affects part of the calf muscles. In addition, the muscle hardening can only be felt within the calf, as usually only part of the muscle is hardened.
The muscle hardening could, however, spread further with continued exertion. In addition, the pain could worsen, as the permanent contraction of the muscles also leads to a partial circulatory disorder.
When does the calf pain occur?
Calf pain when walking / jogging
Calf pain when moving or exercising can have several causes, which can be either orthopedic or internal.
The orthopedic cause usually consists of a poor posture or misalignment of the leg or foot, which is particularly painful under load. Other reasons could be poor footwear or, for example, compression stockings that are too tight.
Another typical example of calf pain during exercise is calf cramps during exercise. They can result from a disturbed electrolyte balance in the blood or a simple overload of the muscles.
While this type of calf pain is directly related to movement, PAD, the peripheral arterial disease, is a different problem. In this disease, arteriosclerosis (calcification of the vessels) ensures that not enough blood can flow to the muscles. This results in what is known as ischemic pain for the patient. This pain usually gets better at rest, as the muscles require less blood.
Calf pain at rest
Calf pain at rest is rare but can occur. Calf cramps would be a typical example of this, as they do not necessarily have to occur during exercise, but can also arise during rest. Frequently, electrolyte disturbances in the blood are the cause of the development of calf cramps, which makes their treatment quite simple.
Furthermore, a very advanced tendinitis after excessive exercise can lead to pain at rest. However, complaints from physical activity must have preceded it. In rare cases, it can also be more exotic-looking diseases such as neuroboreliosis as a late consequence of a tick bite or a soft tissue tumor within the calf muscles.
Nocturnal calf pain
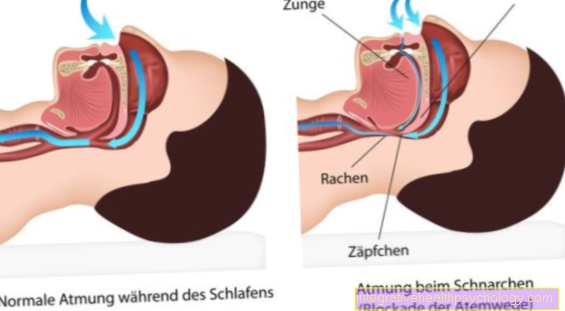
In connection with nighttime calf pain, pain is actually only reported for calf cramps. Another disorder of the calves, but also the rest of the leg muscles, is the restless legs syndrome.
Leg cramps are a typical phenomenon of old age, but they also occur in many young patients. A disturbed electrolyte balance is often the reason for the night cramps. Due to the accumulation of lactate in the muscle or the formation of tiny tears in the muscle fibers, the cramp can lead to a painful calf.
The restless legs syndrome is different. This is based on a disturbed nerve conduction, which triggers a tingling sensation in the legs. Only in rare cases is the feeling described as really painful. The cause of restless legs syndrome can usually not be clearly identified. However, it can be caused by certain medications, especially neuroleptics. A consultation with the doctor is therefore recommended in any case, especially since there are a number of drugs to treat this syndrome.
Read on here: Restless legs
Calf pain after a cramp
Calf pain after a cramp is something that everyone who has suffered from cramps has already experienced. There are basically two possibilities that can explain the pain even after the cramp. The first possibility is "sore muscles". As a result of the strong contraction, some small muscle fibers have torn, which then start to hurt.
The second explanation is based on the fact that the contracted muscle was insufficiently supplied with oxygen during the spasm. As a result, the muscle produces the energy it needs for involuntary contraction under anaerobic conditions, whereby lactic acid, the so-called lactate, is produced. If the lactate is too high, it causes a burning, uncomfortable feeling within the muscle until it has been sufficiently removed by the blood flow
Calf pain with flu
Calf pain is a typical symptom accompanying the flu or a flu-like infection. First and foremost, this is a positive sign because the body's immune system is now fighting the pathogens. This is due to the messenger substances of the immune system, which, in addition to having a pilot function for the immune cells, also make the body more sensitive to pain.
The calf pain or the general muscle pain will disappear as soon as you are on the road to recovery. Treatment with painkillers is potentially possible, but attention should then be paid to drinking a sufficient amount and potential stomach protection.
Find out more about the topic here: Flu symptoms.
Calf Pain During Pregnancy
Calf pain is a common phenomenon during pregnancy. Often it is calf cramps that plague expectant mothers. However, thrombosis can also be the reason for calf pain later in pregnancy. While leg cramps are mostly caused by a disturbance in the electrolyte balance and are very easy to treat, thromboses can be much more risky and should definitely be treated.
In the case of calf cramps, the substitution of magnesium and an occasional massage of the calf muscles are sufficient to prevent cramps.
In the case of thrombosis, however, it is essential to seek medical help. The thrombosis results from a protective mechanism of the body that makes the blood thicker shortly before birth so that uncontrollable bleeding does not occur during birth.
Here you will find everything to do with pregnancy.
What can be behind it if you have calf pain like sore muscles, but have not done any sport?
In this context, two main phenomena come into play. On the one hand, rheumatic muscle complaints can cause muscle pain similar to sore muscles. The cause of the pain, however, is to be seen in an autoimmune reaction of the body against itself. Not every rheumatoid sufferer gets muscle pain in the calf, but unexplained sore muscles-like calf pain could be an indication of the presence of a rheumatic disease.
The second potential factor are so-called statin-associated muscle symptoms, or SAMS for short. Statins are a group of drugs that belong to the lipid-lowering nucleus. They have the effect of synthesizing less cholesterol from the ingested dietary fats, which is why they are used by people with high cholesterol levels.
However, the SAMS are one of the common side effects of statins. Up to five percent of all statin patients complain of the above-mentioned statin-associated muscle symptoms, which often affect the calf muscles. The most extreme form of these symptoms is so-called rhabdomyolysis, which can lead to "muscle breakdown".
Find out all about the topic here: Rheumatism.
The diagnosis
In order to differentiate between the various causes of calf pain and to identify the problem of the affected patient, a targeted and precise anamnesis must first be carried out, in which the frequency, the posture and position of the patient and the physical activity during the occurrence of the pain, the localization, the accompanying symptoms and the impairment of the quality of life are respected.A detailed physical examination should then be carried out, focusing on the calf circumference, calf muscles, skin color, temperature and firmness of the tissue, and skin tension.
Additionally, the examining physician should test the patient's lower extremity reflexes to rule out a nerve disorder or damage. If nerve damage or a herniated disc is suspected, imaging, such as an MRI, may be necessary.
However, if the reflexes are intact and symptoms suggest a thrombosis, Doppler sonography may be performed. This can confirm the diagnosis of deep vein thrombosis.
The imaging
Imaging should be performed to confirm the diagnosis if the medical history and physical examination suggest a herniated disc or damage to nerves. In this case, an MRI is particularly suitable, since soft tissue, such as the intervertebral disc, is recorded in great detail.
An MRI or, even better, a CT scan can also be performed to rule out degenerative changes in the spine. In the case of degenerative changes, the spinal cord can be compressed, which can also lead to pain, numbness and a reduction in strength in the calf.
In addition, possible broken bones can also be detected by an X-ray or CT.
For more information, also read: MRI of the lumbar spine.
The sonography
If symptoms suggest PAD, Doppler sonography of the vessels can be performed. With a Doppler sonography possible bottlenecks can be determined well.
To do this, the examiner first measures the near-body pulses, such as the pulse in the groin, and then works his way along the vascular and nerve bundles in the direction of the foot. If the pulse is no longer recognizable on the foot, this can be a sign of PAOD.
However, the diagnosis of thrombosis cannot be adequately diagnosed by this method. Normal sonography is better for examining the deep veins in the leg. However, small thromboses cannot always be detected. An MRI with contrast agent is most suitable for this.
Find out more about the topic here: Doppler sonography.
The therapy
The therapy of calf pain depends on the cause and the accompanying symptoms.
In the case of minor muscle injuries such as strains or bruises, the first priority is to protect the calf muscles. In addition, symptom relief can be achieved through light pain medication, cooling, elevation and a slight external compression, for example through a stocking or bandage.
If the calf pain is caused by a torn muscle fiber, the same therapy is applied as for a strain. In addition, ointment dressings with anti-inflammatory substances and muscle relaxants can be prescribed. Treatment with manual lymphatic drainage can also lead to swelling of the injury area more quickly.
If, on the other hand, the calf pain occurs spasmodically after consuming alcohol or vigorous physical activity, a supply of minerals should be sufficient therapy. Magnesium can be given orally for this purpose.
Therapy for malpositions of the foot
If the calf pain is caused by chronic bad posture or foot misalignments, it is very important to correct them.
A combination of physiotherapy, posture training and insoles for the shoes can often be used to compensate for poor posture. However, if the arch of the foot is completely deformed, only surgical interventions will help to restore the correct load on the leg and, if necessary, to improve the calf pain.
For this reason, you should contact a doctor in the event of persistent calf pain so that he can find out the cause and correct any misalignments.
Therapy for a herniated disc
If a herniated disc of the lumbar spine is the cause of the calf pain, conservative therapy should be sought first. In particular, strengthening the back, trunk and abdominal muscles can help to relieve the spine and relieve nerve irritation.
Prior to the surgical removal of the intervertebral disc and the insertion of an artificial replacement, a local and targeted injection of anti-inflammatory and local anesthetic substances can relieve the pain.
Find out more about the topic here: Therapy of a herniated disc.
Can insoles help with calf pain?
Insoles cannot help with every type of calf pain. However, they are a therapy for postural calf pain that should be considered.
As a rule, insoles help to correct the position of the feet. If the foot position is changed in the sense of a sickle foot, there will inevitably also be a change in the muscle and ligament structures within the calf. This can result in greater signs of wear and tear, which are expressed as calf pain. Correcting the position of the feet brings the structures back to their original position so that they are no longer subject to greater wear and tear, can recover and the patient can return to freedom from pain.
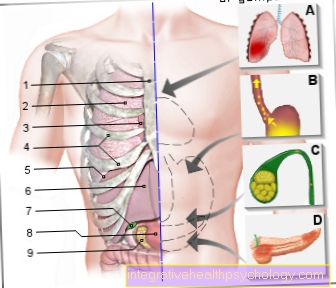
Complications
A particularly serious complication of calf pain can arise if the cause is a venous disease, such as a congestion from a deep vein thrombosis. If the thrombus detaches from its original location and is flushed with the bloodstream to the heart, it can get through the right heart into the lungs and block the small pulmonary vessels here.
This clinical picture is called pulmonary embolism. This results in an insufficient supply of oxygen and nutrients, which can lead to a pulmonary infarction. If larger vessels are obstructed, a congestion occurs that leads back to the heart and puts a lot of strain on it. This also leads to an insufficient supply of the heart, which can lead to heart failure. In the worst case, pulmonary embolism leads to death.
Another dangerous complication can arise from the herniated disc of the lumbar spine as a cause of calf pain. This can lead to chronic damage to nerves and vessels as well as instability of the spine and in the worst case, depending on the exit of the intervertebral disc, injuries to the spinal cord can occur.
In general, chronic calf pain is a significant decrease in quality of life and prevents the person from participating in many activities. A doctor should therefore always be consulted in the event of long-term and unexplained complaints.
The prophylactic measures
To prevent calf pain, it is important to find a balanced amount of exercise. Excessive and one-sided physical stress as well as too little activity and frequent static positions such as long periods of sitting should be avoided. It is also important to do a warm-up program before exercising so that the muscles can slowly become active.
As an alternative to the one-sided physical exertion of jogging, sports such as yoga or Pilates can help to strengthen the muscles and promote health. In addition, an existing incorrect posture can be corrected. In the case of clearly bad posture, additional physiotherapeutic measures should be taken. Correcting the misalignment through orthopedic measures should also be considered.
A balanced diet and avoidance of alcohol and cigarettes help against disturbances in the electrolyte balance, which can lead to short-term and acute leg cramps. These factors are also important to prevent the development or worsening of vascular diseases. Metabolic diseases such as diabetes mellitus or high blood pressure should also be regularly checked and therapeutically well adjusted in order to minimize complications due to vascular problems.
A BMI in the normal range helps to prevent overloading the joints. In addition, being overweight is often associated with increased blood lipid levels. However, these should be kept as low as possible in order to reduce the risk of atherosclerosis and prevent arterial occlusive disease.
When can you start exercising again?
This question depends primarily on the causes of the calf pain. If you have a cold, it is not a problem to do sports again after the cold is over.
However, if the reason for the calf pain is, for example, an Achilles tendon rupture, a good two months of relief should be planned for the next sporting activity.
Overall, it is a question that must be considered individually for each patient in order not to have an unnecessarily long or too short break in sports.



.jpg)














.jpg)