WPW syndrome
definition
The name WPW syndrome stands for a disease known as Wolff-Parkinson-White syndrome. This is a disease from the group of cardiac arrhythmias. It is characterized by an additional pathway between the auricle and the ventricle, which is not present in a healthy heart.
It is a congenital disease that usually only manifests itself after the age of 20. About 0.1 to 0.3% of the population are affected.
Read more on the topic: Cardiac arrhythmias

Type a
WPW syndrome can be divided into type A and type B. The type assignment depends on the area in which the additional (accessory) duct is located. In type A there is an additional conduction path between the left atrium and the left ventricle. The distinction between type A and type B hardly plays a role in WPW syndrome these days.
Type B
The additional conduction path in type B of the WPW syndrome is located between the right atrium and the right ventricle. The conduction path is used in both type A and type B as Kent Bundle designated. Clinically, there is no significant difference between type A and type B. However, they differ from one another, for example, in their presentation in the ECG.
Causes of WPW Syndrome
As mentioned briefly above, the cause of the WPW syndrome is an additional conduction pathway in the heart. The heart works with the help of electrical excitation that is transmitted from one point to another. These electrical excitations ultimately ensure a synchronized contraction of the heart muscle, i.e. the heartbeat.
So that the excitation can get from one point to another, there are certain excitation conduction paths. The conduction of excitation from the atrium to the ventricle is achieved, for example, by the atrioventricular node (AV node) allows. In a healthy heart, it is the only path on which electrical impulses can travel from the atrium to the ventricle.
In the case of the WPW syndrome, in addition to the AV node, there is another such conduction pathway between the atrium and the ventricle. It is called Kent Bundle designated. In the WPW syndrome, the electrical impulses that were conducted via the AV node from the atrium to the ventricle can return to the ventricle via the Kent bundle and trigger a renewed - early - excitation there. This in turn leads to an early renewed excitation of the heart chamber and thus to an acceleration of the heartbeat (Tachycardia).
There are also variants in which the "normal" excitation via the Kent bundle from the atrium to the ventricle and the returning (retrograde) Excitation runs from the ventricle back to the atrium via the AV node.
Read more on the topic: Racing heart (tachycardia)
Is WPW Syndrome hereditary?
No. WPW syndrome is an abnormal condition in the heart that is congenital. However, it is not inheritable.
Diagnosis of WPW Syndrome
First of all, the anamnesis plays a decisive role. This usually gives the first clues to suspect the presence of a cardiac arrhythmia.
The ECG provides further important clues for the diagnosis. In addition to the normal EKG, a long-term EKG measurement over 24 hours or even 7 days may also be used.
An exercise ECG can also be used. Here, the affected person usually sits on a bicycle ergometer and is exposed to increasing physical stress while an ECG is being written at the same time.
An ultrasound scan of the heart (Echocardiography) is done frequently.
A very specific examination in WPW syndrome is the electrophysiological examination (EPU) in which the accessory pathway is examined more closely. A special type of cardiac catheter examination is carried out for this purpose. A therapeutic ablation is usually carried out during this electrophysiological examination.
Which ECG changes do you see in WPW syndrome?
The typical and pathognomonic (certainly indicating a WPW syndrome) EKG change is the so-called Delta wave. The excitation of the atrium is shown as a P-wave in the normal ECG. This is followed by ventricular excitation as a so-called QRS complex.
The Delta wave is a wave that lies directly in front of the QRS complex and, so to speak, merges into it. In the ECG, the WPW syndrome also shows a shortened PQ time (time between atrial excitation and ventricular excitation) and changes in the regression of excitation (ST segment and T wave).
WPW syndrome is characterized by sudden attacks with a racing heart (paroxysmal tachycardia) out. The attacks come out of nowhere and are usually not predictable by those affected. They can last from seconds to minutes, but also up to hours. The heartbeat can increase to over 200 beats per minute (normal heartbeat is between 60 and 100 beats per minute).
The tachycardia attack ends as suddenly as it started. In addition to the rapid heartbeat, you may feel unwell, sweaty and dizzy. In rare cases, WPW syndrome can lead to ventricular fibrillation, an acutely life-threatening cardiac arrhythmia. This leads to unconsciousness and the need for resuscitation.
You might also be interested in: Ventricular flutter and ventricular fibrillation
Therapy of the WPW syndrome
In some patients, an attack can be ended independently by so-called vagal maneuvers. Patients press in their stomach or drink a glass of cold water. In some cases, this can stop the seizures, but they keep coming back. Even acute drug therapy during the attack can bring it to an end, but is not a causal treatment.
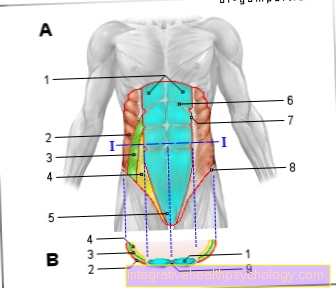
In some patients, attempts are made to establish prophylactic drug therapy, for example with beta blockers. Other antiarrhythmics can also be used here. However, the only causal treatment for the disease is radiofrequency catheter ablation. In this type of treatment, a catheter is inserted into the heart through the inguinal vein, usually as part of the electrophysiological examination.
There the accessory pathway is localized and measured. With the help of electricity, a strong heat is generated at the tip of the catheter with the help of the scars. This results in the affected tissue being eliminated. So the line path is permanently interrupted. This therapy is crowned with lasting success in about 90% of the cases.
You might also be interested in: Therapy of cardiac arrhythmias
When do i need an operation?
An operation in the strict sense of the word is not a treatment option for WPW syndrome. The high frequency ablation is not an operation but an invasive procedure. No skin incision is made and no anesthesia is necessary.
Beta blockers
Medicines from the group of beta blockers can be used as a therapeutic attempt in WPW syndrome. They slow down the conduction of excitation in the area of the AV node.
They have to be taken permanently for this. Beta blockers do not always help, however, so that ablation therapy is often recommended over time.
Who does ablation help?
Radiofrequency ablation is the treatment of choice for WPW syndrome. However, drug therapy can be tried first. However, especially in patients with an increased risk of ventricular fibrillation and sudden cardiac death and in athletes (see below), high-frequency ablation is recommended as the method of choice.
The success rate of the therapy method is relatively high at around 90%. The procedure itself does not require general anesthesia. Ablation treatment is usually not absolutely necessary for patients with WPW syndrome who do not have any symptoms.
How does life expectancy change with WPW syndrome?
WPW syndrome in itself does not change life expectancy.
Patients who suffer from WPW syndrome basically have no limited life expectancy. In addition, there is a causal therapy with high-frequency ablation, which in most cases can eliminate the cause of the disease and thus practically cure the disease. However, in rare cases, sudden cardiac death can occur.
How dangerous can WPW syndrome be?
WPW syndrome can be very dangerous in that it can induce atrial fibrillation in rather rare cases. In patients without WPW syndrome, atrial fibrillation is usually not extremely acute and life-threatening. In patients with WPW syndrome, however, atrial fibrillation can trigger ventricular fibrillation due to the second conduction pathway.
Ventricular fibrillation means that the heart becomes overly excited and beats so quickly that it only flickers and can no longer function effectively. Therefore, if left untreated, ventricular fibrillation is fatal. Immediate resuscitation with defibrillation is required.
Because of this complication, sudden cardiac death, WPW syndrome is a potentially life-threatening condition that requires treatment. The exact type of treatment depends on the symptoms and the risk profile of the person affected.
You might also be interested in: Consequences of cardiac arrhythmias
Can I do sports with WPW syndrome?
Patients who have WPW syndrome but are completely asymptomatic are allowed to exercise without restrictions. However, a cardiologist should regularly monitor the heart's findings. Particularly in the case of very young asymptomatic patients, an electrophysiological examination should be carried out for a more precise diagnosis before the sport is released.
An electrophysiological evaluation should also be performed on all patients with recurrent episodes of palpitations. High-frequency catheter ablation is usually recommended as the therapy of choice here. A resumption of (competitive) sport is usually possible 3-6 months after the successful ablation treatment.
Athletes who cannot be treated curatively by ablation and for whom drug therapy does not work and who suffer from recurrent attacks with palpitations should only exercise very moderately. In any case, all patients with WPW syndrome who do sport should first consult their treating cardiologist.
Read more on the topic: Can you do sports if you have an arrhythmia?