Acute tonsillar angina
Synonyms
Tonsillitis, acute tonsillitis, streptococcal angina
definition
Angina tonsillaris is a mostly bacterial inflammation of the palatine tonsil (s) (lat. Tonsillae palatinae). The colloquial form "angina" should not be confused with other clinical pictures with similar names, e.g. Angina pectoris in acute coronary syndrome. In both cases, angina stands for the noticeable tightness in the throat (Tonsillar angina) or in the chest (Angina pectoralis).
The tonsils are a special type of lymph node, which explains why other lymph nodes in the neck drainage area can also be affected or swollen to a limited extent.

causes
As already mentioned, tonsillar angina is most often caused by bacterial infection. These bacteria are further developed types of the inhabitants of our normal oral flora. This means that the same bacteria (by name) are present in our mouth at all times, but they do not cause any disease. If there are mutations within the bacteria, so that they become more aggressive for us, it can lead to a disease that is transmitted from person to person.
Most often the streptococci are responsible for the development of tonsillar angina, more precisely: Streptococcus pyogenes (group A beta-hemolytic streptococci). Staphylococci, Haemophilus influenzae, pneumococci or even viruses (e.g. Epstein-Barr virus) are less common causes of angina tonsillaris. In the case of chronic tonsillar angina, there is most likely a mixed infection with different bacteria. Immunocompromised people can also develop tonsillar angina due to a fungal infection.
Since bacteria are the most common cause of tonsillar angina with around 99%, the details of this clinical picture will be discussed below, unless otherwise noted.
You can find out more about the topic here: Pus on tonsils
transmission
The angina tonsillaris is most likely about the saliva by means of coughing, sneezing, unclean hands than Droplet infection transfer.
The most common are children and Teenagers Affected by tonsillar angina, which is partly explained by the fact that they have a lot of contact with other children (kindergarten, school). On the other hand, the body's own immune system notice a group of bacteria that has once attacked it and build up a lifelong defense against precisely this group. After every angina tonsillaris gone through, the chances of re-infection decrease because the defense has increased.
After contact with the pathogen, it takes approx. 1-3 days until tonsillar angina manifests itself as a disease (incubation period).
Will the bacterial tonsillar angina successfully with antibiotic treated, it can be assumed that the patient 24 hours is no longer contagious after taking the first antibiotic.
Risk of contagion
Acute tonsillar angina is transmitted through a droplet infection.
This means that the infection takes place via tiny particles dissolved in the ambient air. This Air-particle-pathogen mixture (Aerosol) arises when speaking about exiting saliva or through Sneeze and to cough Of the patients. The pathogens then spread directly through the air. Contact persons of the sick person breathe in the ambient air with aerosol.
About the mucous membranes in the Mouth, nose and throat it comes to the pathogen absorption and subsequently with poor immune status or increased stress to the outbreak of the disease.
Since the pathogens are transported in the air, their spreading radius is relatively limited: Anyone standing more than about three meters away from the sick person has already exceeded the maximum transmission distance and will usually no longer be infected. The typical bacterial causative agent of acute tonsillar angina, the group A streptococci, reach the next patient this way. After diagnosis, however, with a suitable one Antibiotic therapy started, the still sick person is no longer contagious after about 24 hours. Even people who do not show any symptoms themselves can already be contagious to others: it usually takes some time for certain pathogens to multiply sufficiently to trigger the full picture of the infection (incubation period).
Nevertheless, potentially contagious pathogens are already present and can be transmitted. This incubation period is long for most forms of acute tonsillar angina one to three days.
Subdivision
Generally are acute, chronic, recurrent (recurring), unilateral and bilateral Differentiate forms of tonsillar angina.
The simplest form of tonsillar angina is one Redness and swelling the tonsils (catarrhal tonsillitis). However, the superimposition of fibrin as whitish coating into the depressions of the tonsils, which are called "Stipple"Are designated (follicular tonsillitis). In this case, if the patient opens his mouth, the swollen, reddened tonsils (Tonsillae palatinae) visible with whitish coatings and small mucosal defects.
Read more about the topic here: Swollen tonsils
If the surface is particularly pronounced and converges to form a large area, one speaks of one confluent or lacunar tonsillitis. In the case of tissue that has already died, one speaks of one necrotizing tonsillitis.
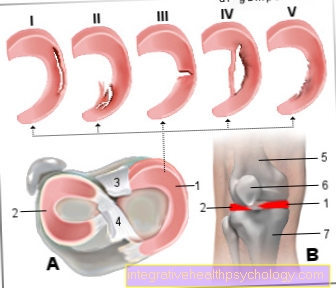
Figure tonsillitis

A - tonsillitis - Tonsilitis
B - Simple catharrhal angina -
Angina catarrhalis
C - throat findings in diphtheria
D - ulcers in bacterial
Forms of angina
- Palatine almond bay -
Tonsillar fossa - Hard palate -
Palatum durum - Posterior palatal arch -
Arcus palatopharyngeus - Anterior palatal arch -
Arcus palatoglossus - Palatine almond -
Palatine tonsil - Back of tongue -
Dorsum linguae - Uvula + soft palate
(Soft palate) -
Uvula palatina + palatum molle - Meandering -
Isthmus faucium - Throat (back wall) -
Pharynx
You can find an overview of all Dr-Gumpert images at: medical illustrations
Symptoms
Tonsillar angina usually begins with severe Sore throat up to difficulties swallowing, accompanied by high fever, a headache, Exhaustion. The pain often extends to the ear and spreads over swollen, sometimes painful lymph nodes in the jaw. Because of the often enormous swelling in the throat, the patient's speech sounds lumpy. The inflammatory secretion from the tonsils causes a bitter aftertaste when eating and drinking as it drains into the throat. Often times also occurs in the course of the strep throat Bad breath which the sick and fellow human beings perceive as unpleasant.
diagnosis
If one sees severely reddened tonsils with whitish coatings when looking into the throat, then after the differential diagnosis has been ruled out, tonsillar angina can be assumed.
This suspicion can be attributed to the Rapid streptococcal test be hardened. For that, a Throat swab taken and painted on a window of the test. If the test is positive, antibiosis is prescribed. If the test is negative, a bacterial culture of a throat swab can be created in case of doubt. However, the results can only be expected after days, which means that this verification method has lost its value.
A Blood collectionto display different inflammation values (BSG and CRP) or to rule out other diseases can be helpful in some cases. With Antibodies in the blood can only be expected after weeks, which means that testing for antibodies only makes sense in special cases.
therapy
At the beginning of the disease or in addition to drug treatment Camomile tea, Envelopes with essential oils or Healing earth Provide relief. Fresher ginger With honey and lemon as a hot drink or also Sage tea and salt water for gargling will help heal and reduce pain. In acute bacterial tonsillar angina there is usually one penicillin For 7-14 days prescribed. Alternatively, there are other antibiotics to choose from if you have allergies or other contraindications. If the pain or fever persists, appropriate medication such as Paracetamol or Ibuprofen be taken after consulting a doctor. Iodine-containing throat rinses for gargling and mucosal anesthetics can be used concomitantly. In the case of chronic tonsillar angina, a therapeutic attempt with antibiotics can be started. The last therapy option is the Almond removal (Tonsillectomy).
Antibiotic therapy for acute angina
Typically the triggers are acute Angina tonsillaris bacteria, mostly streptococci (Streptococcus pyogenes). It is very rarely found Viruses as Pathogen the classic acute tonsillar angina.
Because the pathogen bacteria purulent bacterial acute tonsillar angina should always be treated with an antibiotic. This should of course not be taken or prescribed lightly and carelessly, which is why a doctor must examine the oropharynx and then make a decision. Most of the time this is proven penicillin V prescribed for 7 days. If you are intolerant to penicillin, there are of course other alternatives.
Home remedies for acute tonsillar angina
To Treatment of acute tonsillar angina In addition to conventional drug therapy, there are also some well-proven ones Home remedies on: This is how flushing the throat or gargling with a disinfectant solution (e.g. sage, chamomile, ginger infused as tea and placed in a cool place) often provides relief and makes swallowing easier.
Also cold neck wraps counteract the inflammation in the throat and can thus relieve the pain. In general, everything that works well against pain and fever is recommended; These can be cold towels that lie on the forehead, but also leg wraps, herbal teas and of course a lot of rest. Many patients feel special Camomile tea as pleasant at acute tonsillar angina. Drinking plenty of fluids is beneficial for recovery. However, you shouldn't choose fruit juices if possible, as the acid they contain irritates the throat even more.
Cold drinks or normal ice cream relieve the difficulty swallowing. Food should be soft and only slightly or not at all seasoned. Also on that Smoke it is better to do without for some time.
Homeopathy for acute tonsillar angina
The homeopathic approach assumes that the acute tonsillar angia is only a symptom of a deeper underlying disease and consequently it must be treated as a direct cause
Against Sore throat are preparations like Aconitum napellus or Belladonna or Mercury corrosivus recommended.
However, the homeopathy numerous other alternatives. At the latest at the point in time when pus appears in the throat appears, you should urgently consult a doctor! Just one bacterial tonsillar angina is not to be underestimated and definitely has to go with one antibiotic that only a doctor can prescribe and prescribe. A wrong diagnosis or pure self-treatment can even hinder the healing process! However, there is nothing wrong with using homeopathy to support antibiosis at the patient's request.
Duration
Acute tonsillitis usually lasts a few days until the patient has recovered. Usually it is completely healed after about one to two weeks. Chronic tonsillar angina is when the symptoms persist for more than three months or even never go away.
The degree of risk of infection to others depends on the type of pathogen: while a bacterial tonsillar angina As mentioned, with proper antibiotic therapy, it is usually no longer contagious after one day, the risk of viral diseases, on the other hand, is usually much longer. The point in time at which there is no fever or symptoms is a good guide for estimating the end of the illness.
Complications
- Basic tongue tonsillitis: The rear end of the tongueThe direction of the throat is very swollen because the lymph nodes of the tongue are also affected. The making of Shortness of breath is possible due to the enormous narrowing of the throat, so that inpatient treatment may be necessary.
- Streptococcal gingivostomatitis: The entire oral mucosa is inflamed and partly painful Abscesses occupied, which also on the Lips can pass over.
- Secondary illnesses after streptococcal angina: After tonsillar angina there is a delayed Antigen-antibody reactioncausing inflammation of the kidneys (acute Glomerulonephritis), joints (acute rheumatic fever) or the heart (Endocarditis rheumatica).
Depending on the organ involvement, the internal treatment with additional antibiotic protection and, if necessary, removal of the tonsils must take place.
Other possible complications: Abscesses in the throat or in the oral cavity (Peritonsillar / retropharyngeal abscesses), Inflammation of the heart (Endocarditis, Myocarditis, Pericarditis), thrombosis the jugular vein (Jugular vein thrombosis), Blood poisoning (sepsis).
The acute tonsillar angina as a bacterial infection, unfortunately, it can rarely be sharply delimited, so that there are some potentially possible complications. Theoretically, the infection can spread to neighboring structures at any time.
If such a transfer occurs, abscesses are, for example, between the tonsils (Peritonsillar abscess) or in back of the throat (Retropharyngeal abscess) the result, up to and including throat phlegmon.
This more serious complication is a rapidly spreading inflammation of all the soft tissues in the neck area. She represents an instant OP indication dar; intraoperatively the infected tissue is removed as completely as possible under antibiotic therapy, rinsed and disinfected. Without such therapy, a throat phlegmon spreads further and further and can ultimately lead to death via generalized sepsis (blood poisoning).
Can also be a Neck phlegmon in the one on the neck Jugular vein break in and trigger a jugular vein thrombosis there. However, the risk of bacteria transferring is not only a local one, but also a systemic one: if the entry port is suitable, the bacteria enter the bloodstream. This causes severe blood poisoning and / or inflammation of other organs into which they enter the bloodstream.
For example, inflammations of the heart (endocarditis, myocarditis ...) or the kidneys are conceivable. In a few rare cases, acute tonsillar angina also causes serious problems.
For example, when the tonsils swell very much in the throat. This can then become more acute Shortness of breath to lead. Very rarely can one Streptococcal infection also trigger a post-infectious rheumatic fever, which is associated with severe joint pain and fatigue as well as fatigue. This occurs because antibodies are formed against the bacteria that caused the original infection. In rare cases, these also react with the body's own structures. The skin, heart, joints, and brain are most likely to be affected by this serious complication.
Differential diagnosis of tonsillar angina
- Acute viral pharyngitis: Similar symptoms, but no swelling / coating of the tonsils.
- Lateral cord angina: Inflammation of the lymph vessels in the throat, mostly on one side, no plaque on the tonsils.
- Scarlet fever: Additional rash (starting on the upper body), strongly reddened, dotted tongue ("Raspberry tongue“).
- diphtheria (very rare): The whitish deposits on the oral mucosa and the tonsils bleed when they are removed and are painful, sweetish halitosis, mucous membrane necrosis
- Glandular Pfeiffer fever (infectious mononucleosis): Especially central coatings on the tonsils, severe fever and fatigue, involvement of the spleen and liver possible.
Furthermore, there are special forms of tuberculosis, the Tonsil carcinoma, Herpes or syphilis to exclude related inflammation.
Chronic tonsillar angina
In chronic tonsillar angina (more often than 5 times a year in 2 consecutive years) the tonsils are due to the frequent inflammation pitted changed and scaled down. Purulent cell debris (Detritus) can therefore drain poorly and inflammation occurs again and again. This detritus is visible in the hollows of the tonsils, whereby the symptoms can be much less pronounced than in acute tonsillar angina.
Chronic tonsillar angina can also act as a "focus" for others chronic Inflammations / diseases such as the rheumatic fever, Iritis, psoriasis come into question. Chronic tonsillar angina should be ruled out if the above-mentioned diseases are not very successful.




.jpg)