bronchial asthma
definition
Bronchial asthma is a chronic disease of the airways that leads to attacks of breathlessness and coughing.
In asthma, there is a repeated and sudden narrowing (obstruction) the airways. If asthma has persisted for a long time, there may also be a structural reorganization of the airways.

What are the typical symptoms of asthma?
- Attack-like shortness of breath
- Dry cough
- cough
- Dry noises when you exhale (so-called "stridor")
- Suffocation
- Chest tightness
- shortness of breath
- especially nocturnal symptoms
Read more on this topic at: Symptoms of bronchial asthma
Shortness of breath
In asthma, acute attacks of shortness of breath often occur. You have the feeling that you are no longer able to breathe properly because your airways cramp up. This mostly occurs at night or early in the morning. In addition, there are dry noises, especially when exhaling, which also lead to fear and thus increase the shortness of breath. During these attacks it is therefore very important to try to remain calm and to normalize breathing evenly and in a focused manner.
Read more on this topic at: Shortness of breath
Mucous bronchi
The cause of asthma is inflammation. This leads to an accumulation of many immune system cells in the lungs. As part of this inflammatory reaction, there is also an increased formation of slimy secretion that collects in the bronchi. It is therefore important to also take expectorant medication during treatment and cough up the mucus in a targeted manner.
Further information on the subject can be found at: Mucous bronchi
to cough
Coughing often occurs in asthma, often in attacks and in response to certain stimuli. Since asthma is often triggered by different triggers, the body reacts to these with sometimes violent irritable cough. These triggers include, for example, pollen, animal hair, house dust mites, or physical exertion. As the disease progresses, a chronic cough often develops, which becomes ubiquitous in everyday life.
These therapy options are available
- Avoidance of the triggering factor in allergic asthma
- Desensitization (preferably at an early age)
- Inhaled glucocorticoids (e.g. budesonide)
- Inhaled beta-sympathomimetics (e.g. Sabutamol)
- Leukotriene receptor antagonists (e.g. montelukast)
- Theophylline
- Tiotropium bromide
- Biologicals
Read more on this topic at:
- Therapy of asthma
- Emergency spray for asthma
When do i need cortisone?
Almost two years ago a new regimen was established in the therapy of asthma. This is a so-called step-by-step scheme that is used for long-term drug therapy. It is important to start with the lowest possible medication and to increase this depending on success and freedom from seizures.
Initially, only acute attacks are treated with the help of so-called beta-sympathomimetics. If these are not sufficient and an increasingly chronic cough is established, the patient will switch to long-term therapy in the next stage. This means that from now on, daily drug therapy is also recommended. The first drug used here is cortisone in inhalative form as a spray. The onset of action cannot be observed immediately. The full effect only unfolds after approx. 2 weeks. So it is not only purely therapeutic, but also protective in order to prevent the further progression of the disease. Cortisone should be inhaled twice a day, the dosage depends on the preparation.
Further information is available from: Cortisone therapy for asthma
These drugs are used
The drug therapy of asthma is very diverse and structured in a step-by-step scheme in which different drugs are combined with each other depending on the severity of the disease.
One group is formed by beta-sympathomimetics, which widen the airways and relax the muscles of the bronchi. These are available both as a short-acting form for acute attacks, and as a longer-acting form to increase control over asthma.
Cortisone also plays a big role as an anti-inflammatory drug. It is important that the therapeutic cortisone level first has to be built up over a few weeks so that it can work sufficiently.
Other drugs are theophylline, which dilates the airways, but is not suitable in an emergency, and leukotriene receptor antagonists such as Montelukast.
If all of these drugs are no longer sufficiently effective, so-called biologicals are used. These act very specifically in the body and specifically inhibit messenger substances that promote inflammation. They also have an anti-allergic effect. Examples are omalizumab or mepolizumab.
Read more on this topic at: Medicines for asthma
homeopathy
Many asthma sufferers regularly take homeopathic remedies to improve their symptoms. There are different preparations depending on the type of symptoms.
For spasmodic attacks of coughing, for example Lobelia inflata can be taken three times a day in the form of five globules. This will quench the cough and also reduce excessive breathing, i.e. hyperventilation. If there is an increased cough with sputum, which usually looks white and occurs mainly at night, potassium iodatum can also help as a five-fold dose of globules three times a day.
Sambucus nigra with five globules three times a day is recommended for sudden dyspnea with hoarseness. If you get the feeling of suffocation, Spongia can help with five globules three times a day. This preparation can also be effective for wheezing. Another homeopathic remedy that can be used for asthma (whether allergic or chronic), but also for COPD, is Ammi visnaga.This preparation should also be taken three times a day in the form of five globules.
Breathing exercises
In asthma, breathing exercises can have a supportive effect and reduce situations in which there is acute shortness of breath. An important element is the lip brake, where the lips lie on top of each other and the air is only pushed out through a small opening when you exhale. The coachman's seat, in which the arms are placed on the thighs while sitting, offers additional relief for the auxiliary breathing muscles.
Since attack-like coughing fits often occur in the context of asthma, it is important to control them and to remove as much mucus as possible from the lungs. For this purpose, a so-called bronchial toilet should be carried out every morning, as the mucus accumulates during sleep, especially at night with shallow breathing. To do this, you first take a deep breath. This is followed by a slight throat clearing and about half of the air is exhaled again. The leftover air can now be used to easily cough up the mucus. The whole thing should be repeated several times and integrated into everyday life.
To further strengthen the auxiliary breathing muscles, we recommend stretching exercises for the intercostal muscles and strengthening the diaphragm.
Further information on this topic can be found at: Breathing exercises
Causes, development and risk factors
Asthma is a repetitive and sudden narrowing (obstruction) the airways.
An asthma attack can be triggered by various stimuli that have no effect in a healthy lungs, but trigger an inflammatory reaction of the bronchial mucosa in an asthmatic.
The mucous membrane swells up and increasingly secretes a tough mucus. The bronchi become mucous and narrowed. In addition, the muscles of the smaller airways contract like a spasm, which makes breathing even more difficult. The oxygen supply to the lungs and thus to the body deteriorates; in extreme cases, a life-threatening condition can occur.
Read more on this topic at: Mucous bronchi
The development of bronchial asthma is a process that is influenced by many factors and in which, in addition to environmental factors, genetic predispositions are also involved. A distinction is made between exogenous allergic asthma and non-allergic asthma. Mixed forms are common.
The basis of exogenous allergic asthma is a faulty response of the immune system. Possible allergens are: house dust mites, mold, animal hair and dandruff, pollen and occupational allergens such as Flour for the baker.
Non-allergic asthma is triggered by a number of factors that do not mobilize the immune system: physical exertion, cold air, sometimes also moist and warm air, stress and emotions (laughing, crying, fear).
Most of the time, however, both forms occur together, since e.g. the constant inflammation of the airways in allergic asthma to bronchial overexcitability (Hyper-responsiveness), which means that even the smallest stimuli such as smoke, perfume or cold air are sensitive and the mucous membrane reacts in the manner described above.
Other special forms are exertion-induced asthma (Exercise asthma), which usually occurs in the relaxation phase after physical exertion, and drug-induced asthma, mainly triggered by painkillers that contain acetylsalicylic acid - ASA (aspirin) for short (part of most headache tablets).
In allergic asthma, a very specific dysregulation of the immune response (the body's own defense reaction) takes place, which is directed against substances that actually pose no danger to the body. In addition, most asthmatics have an increased blood level of IgE (I.mmoglobulin E.) on. IgE is a special antibody of the immune defense that serves as a messenger in the body to mediate an allergic reaction.
At the beginning of the disease, the triggering allergen to which the body reacts can sometimes still be determined. Usually, however, more and more triggering allergens are added over time, which is then referred to as an expansion of the allergy spectrum. The original stimulus can no longer be determined and avoiding the triggering allergens is becoming more and more difficult. not only do without a pet, but gradually also on spring walks and perfume.
Psychological factors also play a role. On the one hand, they can influence the extent of the disease, and on the other, they play an important role in coping with the disease.
Patients with bronchial asthma often have other diseases that are classified as atopic clinical pictures. Atopy is a genetically based willingness of the organism to react to various natural or artificial environmental stimuli with an excessive immune response. In addition to bronchial asthma, atopic diseases include e.g. also neurodermatitis or “hay fever”.
If the parents have atopic diseases, the child's risk of developing asthma is up to 50% higher.
Read more on this topic at: Causes of asthma
Patients who suffer from both asthma and cardiovascular problems should not take the medicine Korodin. Korodin is used to treat low blood pressure and heart failure. If they are hypersensitive to the drug, these patients experience difficulty breathing and asthma attacks. For more detailed information, read the topic under the article: Korodin drops
Can stress also trigger asthma?
The role of stress in the development of asthma has long been a very controversial issue. Nowadays it is mostly believed that stress in the form of mental conflict is not a cause of asthma. What is certain, however, is that stress can have an additional reinforcing effect on the development of asthma. However, a distinction must also be made between physical (i.e. physical) and psychological stress.
A clearly defined form of asthma is exertion asthma, which occurs during physical exertion, often especially during physical exertion in cold air.
In acute psychological stress there is often increased breathing (Hyperventilation), which in the long run can make breathing difficult. In order for an asthma illness to develop from this, however, other factors must also be added.
In many cases, however, several factors, such as cold, genetics, pollen and other environmental influences in combination play a decisive role in the development of asthma.
Asthma from Aspirin® / Ibuprofen
Asthma can be caused by a variety of causes. One of them are drugs, especially so-called NSAIDs (non-steroidal anti-inflammatory drugs), such as Aspirin® or ibuprofen. This form of asthma is also known as analgesic asthma, i.e. pain reliever asthma.
The full mechanisms behind this trigger are not yet fully understood. The most common assumption is that the long-term use of aspirin or ibuprofen, for example, shifts the balance between two important messenger substances. One is prostaglandin E2, which enlarges the airways and is only produced to a reduced extent by aspirin. The other substance is leukotrienes, which cause the airways to contract and are more produced when aspirin is taken for a long time. This shifts the equilibrium between these two substances in the direction of the leukotrienes and the airways are increasingly narrowed. Therefore, leukotriene antagonists are also common in therapy, as they precisely inhibit the leukotrienes.
Often the form of analgesic asthma is a chronic obstructive pulmonary disease, i.e. COPD, as a pre-existing condition.
Read more on this topic at: NSAIDs
Asthma from mold
Asthma can be caused by a variety of causes. It has not yet been clarified whether mold is a cause of its own. If there is an allergy to a type of mold, this can certainly contribute to the development of asthma. Studies have also shown that prolonged stay in damp rooms promotes the development of asthma. Therefore, if mold is discovered in an apartment, renovation should always be carried out.
Common cold asthma
A simple cold cannot develop into an asthma illness per se. Rather, a cold can intensify the symptoms of an already existing form of asthma, as the cold also weakens the airways and attacks them by viruses. This causes an increased inflammatory process in the lungs and the shortness of breath and coughing can intensify. In addition, a cold can trigger an acute attack of asthma with chest tightness and shortness of breath. Therefore, if you have asthma and an additional cold, you should always consult a doctor.
What is an asthma attack?
A severe asthma attack can result in what is known as an acute asthma attack. This is an acute, significant worsening of symptoms. The most present symptom is the increasing shortage of breath, it becomes more and more difficult to breathe and one begins to gasp. This, in turn, panics the body, making the shortness of breath even worse. Often those affected use their entire auxiliary breathing muscles by propping up their hands and standing, for example, in the so-called goalie position.
In addition, tachycardia, i.e. a significantly faster beating heart, anxiety, confusion and cyanosis, i.e. an insufficient supply of oxygen to the body, can cause breathing problems. So it is very important to calm the affected person down. Breathing exercises, such as the lip brake, the administration of oxygen and fast-acting drugs such as inhaled beta-sympathomimetics or intravenous cortisone preparations such as prednisolone, are quickly effective.
In some cases, the acute asthma attack cannot be sufficiently reduced despite proper therapy and the so-called status asthmaticus can occur, which can sometimes have life-threatening consequences. This is an absolute emergency that must be treated immediately in the hospital, since the shortness of breath can result in a pronounced lack of oxygen in the body.
For more information, see: Asthma attack
This is how asthma is diagnosed
Various diagnostic tools can be used depending on how the asthma developed. The anamnesis, i.e. the doctor-patient conversation, and the physical examination always play a central role in the initial assessment. In addition, blood tests can provide more information about the type and severity of the inflammation. The extent of the disease can be better assessed in the chest x-ray and there are numerous function tests of the lungs to determine the breathing capacity that is still present.
Further information on this topic is available at: How is asthma diagnosed?
These tests are there
The lung function test (also called "Lufu") and the methacholine provocation test are used in everyday life as tests to examine the lungs in asthma. With the lung function, different volumes are measured with the help of a special mouthpiece, the patient here e.g. you are asked to breathe in and out as deeply as you can. In the methacholine provocation test, the administration of methacholine (this causes the airways to contract) tests how strongly the lungs are irritated by this substance.
Read more on this topic at: Pulmonary function test in asthma
Consequences of asthma
If the disease is not treated properly or if treatment does not work, there is a risk of worsening asthma attacks, some of which can be life-threatening and require immediate medical treatment (status asthmaticus). On the other hand, long-term damage to the lungs and the cardiovascular system can occur.
The fundamental problem with an asthma attack is that the air can no longer leave the lungs, meaning that no fresh air can come in, even if during an attack it appears that the person concerned is “gasping for air”. In the long run, multiple asthma attacks can put such strain on the lungs that insufficient exhalation causes the lungs to over-inflate.
One speaks here of pulmonary emphysema. This leads to severe, irreversible impairment of lung function, which manifests itself in a drop in performance and reduced resilience for the patient. Another consequence of the overinflation of the lungs can be a weakness of the right heart - called cor pulmonale.
The reason for this is the constantly increased pressure in the lungs caused by the overinflation, which puts excessive strain on the right heart. All of these sequelae can be avoided with the right treatment. It is therefore all the more important that therapy is as early and consistent as possible.
Can you cure asthma?
Asthma is a chronic inflammatory disease. This means that the lung tissue is attacked and damaged by many different immune cells and messenger substances. Unfortunately, this process is not completely reversible in the long term and asthma cannot be cured. After diagnosing asthma, it is important to realize that this disease can last for a lifetime. However, nowadays asthma can also be treated very well and therefore a relatively normal life can be led despite everything. And in many cases the asthma subsides to such an extent that those affected are considered symptom-free. This can be observed especially when diagnosing children and adolescents.
The time of diagnosis is decisive. If asthma occurs in children, for example, only with exertion, this is often misinterpreted as unsportsmanlike conduct and a diagnosis is only made years later when the disease is already advanced.
What is the asthma triad?
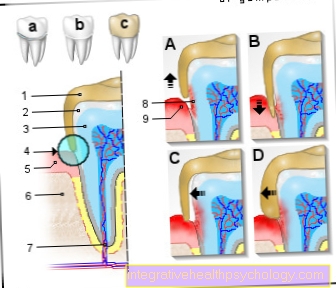
The asthma triad is understood to be the three elements that play a decisive role in the development of asthma. These include the so-called bronchospasm, i.e. the cramping of the airways (bronchi), and mucosal edema, i.e. the swelling of the mucous membranes due to increasing inflammation. The third factor is hypersecretion, i.e. the increased secretion of mucus from the cells of the lungs, which is caused by the inflammatory infiltration of the lungs.
Asthma and sport - what do I have to consider?
Many people think that if you have asthma you should exercise less. However, this is a big mistake, as the lungs can withstand less and less stress, which, however, the asthma disease itself definitely represents for the airways.
The decisive factor in sport is the way in which it is practiced. First of all, the type and intensity of the sport should be discussed with the doctor, as the latter in particular depends on how pronounced the asthma is and which medications are already being taken against it. Endurance sports such as running, swimming or dancing are particularly suitable. It is important to always listen to your body and to slow down if you are in pain. In order to get the lungs used to the strain, it makes sense to start the sport with slow and continuous training and then gradually increase it and adapt it to the individual breathing difficulties. In some cities in Germany there are now asthma sports groups or lung sports groups.
Which doctor treats bronchial asthma?
If you suspect you are suffering from asthma, you should see a doctor as soon as possible to clarify this diagnosis and, if it is available, to initiate appropriate therapy. Pulmonologists, so-called pulmonologists, are responsible for this. Some also have the additional qualification as pneumo-allergologist. If the asthma is an allergic asthma, for example due to house dust mites, an allergist can also be consulted. The referral can be issued by the family doctor.
How do I differentiate asthma from COPD?
Asthma and COPD are the two most common chronic diseases of the respiratory tract, but they differ in many important ways. While COPD only causes shortness of breath under exertion, in asthma it occurs as attacks and not necessarily through exertion (but this can also happen). In many cases, asthma is an allergic disease; this is almost never the case with COPD. Another important difference is the course of the disease. COPD is a downright progressive disease, while asthma can also temporarily stop the disease.
Read more on this topic at: COPD
What role does vitamin D play in asthma?
Like many other vitamins (for example vitamin C), vitamin D provides enormous support for the immune system. In recent years, research has focused more and more on vitamin D and there are now more and more studies on it. However, the exact mechanisms are not yet fully understood. Vitamin D is required as a messenger substance in many synthesis and metabolic processes in the body. With a sufficient vitamin D level, the body is strengthened accordingly, which can have a positive effect on certain diseases.
A study from Israel provided interesting results: in people with asthma with a low level of vitamin D, the disease worsened over time. Conversely, an increased level of vitamin D is associated with a significant improvement in symptoms in asthma. It is therefore recommended that you consume enough vitamin D. A regular stay in the sun is sufficient for this and you do not necessarily have to resort to food supplements directly. However, if this is desired, vitamin D3 is particularly recommended.
Can I use the sauna if I have asthma?
With asthma it is important to strengthen the immune system regularly. A visit to the sauna is very suitable for this, as it stimulates the body's circulation and metabolic processes. The warmth of the air promotes blood flow to the mucous membranes in the lungs as does the inhalation of water vapor or, depending on the sauna, other substances in the air. The relaxing effect on the muscles is also beneficial for the auxiliary breathing muscles, as they are particularly stressed in attacks of shortness of breath.
Frequency (epidemiology)
The incidence of bronchial asthma, like other allergic diseases, continues to rise sharply. In Germany around 10% of the child and 5% of the adult population are affected.
In children, bronchial asthma is one of the most common chronic diseases. If the parents have "atopic" diseases (e.g. allergies), the child's risk of developing asthma is up to 50% higher.
Differences between East and West Germany are now converging, whereas earlier a significantly lower incidence of bronchial asthma could be observed in East Germany, which supports the assumption that certain living conditions (e.g. increasing hygienization) support the occurrence of the disease .
Read more on this topic at: chronic disease
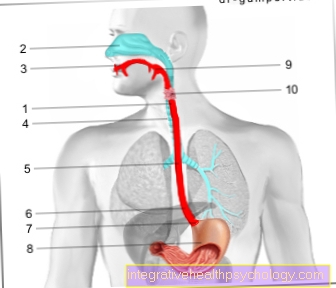
Lungs anatomy

Anatomy and location of the lungs
- right lung
- Windpipe (trachea)
- Tracheal bifurcation (Carina)
- left lung
In order to understand the processes in the body that underlie asthma, it is necessary to take a closer look at the human respiratory system. Breathing is a very complex process in which several structures are involved. In addition to the lungs, in which oxygen is absorbed from the air into the blood, the airways play a major role.
The air enters the windpipe (trachea) from the mouth or nose. The trachea branches in the chest into a right and a left side branch - called the main bronchus - and they lead to the left and right lungs. In the lungs, the two main bronchi continue to branch out and form smaller and smaller branches that ultimately lead to the alveoli, where gas exchange takes place. With each bifurcation, the diameter of the air-conducting bronchi becomes smaller.
You can think of the whole thing as an upside-down tree, on which the air bubbles hang like apples, which is why the whole thing is also called a bronchial tree. The task of the bronchial tree is not only to guide the air we breathe to the alveoli, it also ensures that the air is warmed, moistened and cleaned when it arrives there.
In order to perform these tasks, the bronchial system is covered with a special mucous membrane. It is very well supplied with blood, which leads to an exchange of heat between air and blood, covered with small hairs in which e.g. Pollen or grains of dust get caught and it secretes mucus, from which the air absorbs moisture as it passes. All of this literally happens in one breath. Under the mucous membrane of the airways there is a layer of muscle arranged in a ring.
It enables the body to regulate the diameter of the bronchi in a targeted manner. A narrowing is called an obstruction and a widening is called a dilatation. In a healthy state, the body sets this regulation e.g. when exposed to heavy stress that requires increased breathing, such as a continuous run / jogging. By widening the bronchi, the air gets more easily into the lungs, which ensures a better supply of oxygen.
Further information on the subject is available at: lung

Figure bronchi
- mucus
- Mucous membrane
- Musculature
Consequences of asthma (right figure)
- The bronchial muscles (3.) thicken
- The mucous membrane (2.) swells
- There is more and more tough mucus (1.)