Basalioma on the ear
introduction
Numerous doctors and companies warn of skin cancer every summer. Mostly it is from the well-known "Black" skin cancer spoken, but also "White skin cancerto which that Squamous cell carcinoma and basal cell carcinoma (basal cell carcinoma) of the skin carries its risks. Although a basalioma metastasizes only in rare cases and is therefore rarely fatal, its destructive (destructive) growth can lead to disfigurement of the face, which is one of the Predilection sites for the development of a basalioma (e.g. on the ear).
definition

A basalioma is a skin tumor that consists of special cells in the epidermis (Epidermis), the so-called Basal cells, arise. A small, coarse one forms on the affected area over several months and years nodewhich often goes unnoticed for years. The basalioma is called the spinalioma (squamous cell carcinoma) White skin cancer and is mostly in contrast to the malicious black skin cancer (Melanoma) rarely fatal. Their slow, displacing growth is typical of basaliomas. Although they do not form metastases (daughter tumors), they grow infiltratively into adjacent tissue and destroy them. In the worst case, this can lead to disfigurement of the affected skin area (e.g. face or ear) or to the destruction of vital structures such as vessels and nerves. For this reason, doctors refer to the basalioma as a semi-malignant or “semi-malignant” tumor.
As with so many things in medicine, basalioma also has different manifestations that the tumor can take. But that is typical for every basalioma spherical, raised shape; the surface covered by vessels and a pearl-like edge hem. One manifestation of the basalioma on the ear is the solid or also nodular basalioma. This is a skin-colored, hemispherical tumor made up of small, tortuous blood vessels (called the Telangiectasia) is coated. Another form is that Cicatricating basalioma, which denotes an inwardly growing tumor with a dented center. Doctors also call this depression "Meltdown". Here, too, the pearl-like change at the edge of the tumor is typical. Another form of basalioma is that Scleroderma basalioma. This type of basalioma often goes undetected because it lacks the typical telangiectasia and pearl-like changes at the edge. The only abnormality here is one hardened, skin-colored surface. Other forms of basalioma are ulcerating basalioma (Rodent ulcer), which grows mainly in width and length, but not in depth, and the destructive basalioma (Ulcer terebans), which mainly grows in depth and often leads to bleeding due to the destruction of cartilage and bone tissue. Other forms are still that Pigmented basaliomawhich often appears heavily pigmented and knotty; and superficial basal cell carcinoma, which is common in elderly people with psoriasis who have been treated with arsenic. Typical here are sharply demarcated, red-brown skin changes.
frequency
Basalioma usually occurs only at an older age from around 60 years on. As one of the main causes of basalioma is a years of strong sunlight exposure is, nowadays, in the course of lifestyle change, more and more younger people who frequently visit solariums or spend hours sunbathing become ill. Especially people who have a genetic tendency to sunburn quickly are among them risk groups for basaliomas. This mostly includes people with fair skin, blonde or red hair and blue eyes, the so-called Celtic skin type. People who have worked outdoors for years (e.g. farm workers) and have been exposed to strong sunlight also often develop basal cell carcinoma or squamous cell carcinoma of the skin. Typically, the basalioma occurs in parts of the body that are difficult to protect from light. these are head, face and neck in over 80% of cases. Infestation on the forehead, scalp and ears is particularly typical. In Germany get sick every year approx. 130,000 people new from a basalioma.
Causes of a basalioma on the ear
One of the main causes of basalioma is one years of strong sunlight exposure with sunburn. Excessive exposure to sunlight causes Damage in the DNA of our skin cells, which leads to malignant degeneration. Often, however, these cells are recognized and destroyed by our body. This prevents the development of tumors. If these diseased cells still survive, tumor cells develop from them, which become one unstoppable tumor growth being able to lead. A Weakness of the immune system can facilitate this process.Other causes for the development of a basalioma are genetic predispositions, the skin type, scars that favor the development of a basalioma or a treatment with arsenic, which was previously used against psoriasis. Other skin diseases such as albinism or xeroderma pigmentosa are also associated with an increased risk of skin cancer. The latter is a rare genetic disease based on a chromosome defect and which is associated with a massive risk of skin degeneration when exposed to light. Even the smallest exposure to light can cause skin burns and wart-like structures, which degenerate over time and become skin cancer. Those affected, mostly children, must be consistently protected from light. For this reason, the disease also has the nickname: Moonlight sickness.
Symptoms of a basalioma of the ear
A typical symptom of the basalioma on the ear is the roughly pea-sized, hardened, hemispherical and painless elevation, on the surface of which there are thin, tortuous vessels, so-called Telangiectasia are located. Since basaliomas grow very slowly, they will only be noticed after many years. With increasing growth, the typical pearl-like edge is formed. This describes an edge wall made up of many small skin-colored to pearly-colored nodules that are strung together like a chain. Usually the basalioma is skin-colored, but like the pigmented basalioma, it can also appear brown to blackish. This in turn can lead to confusion with malignant melanoma (black skin cancer). The ulcer-like basal cell carcinoma usually appears in the form of a skin abrasion, the surface of which is covered with a crust and which does not heal even after many weeks, but rather increases in size. The flat-growing basalioma, on the other hand, is more reminiscent of eczema or psoriasis due to its red-brownish color. After a while, however, the typical bead-like border forms here too, which makes the diagnosis of a basalioma on the ear reliable.
Read more on this topic at: Symptoms of a basalioma
diagnosis
Due to its characteristic appearance, the diagnosis of basalioma in the ear is usually made clinically. However, a biopsy, i.e. a small tissue sample from the affected area, which is then examined under a microscope. Another possibility in the diagnosis of a basalioma is the photodynamic therapy (PDT). By means of PDT, the extent of the basalioma growth in depth can be determined. For this, the affected skin area is rubbed with a special cream and then with Wood light irradiated. The sick cells, which have been enriched with the active ingredient in the cream, then light up clearly visible.
Complications
If left untreated, the basalioma grows continuously into the depth and breadth of the skin. This can lead to the destruction of cartilage and bone tissue and skin areas. In the worst case, this results in severe disfigurement of the face or the destruction of vital structures in the head and neck area such as nerves and vessels. For this reason, even if basaliomas do not metastasize, always be subjected to treatment.
Therapy of a basalioma on the ear

A basalioma has a low rate of metastasis and can thus infiltrate and destructively grow into the neighboring tissue. This makes therapy of the basalioma necessary. Depending on the type, size and extent of the basalioma on the ear, as well as the age and state of health of the person affected, there are various therapy options. Because of its curative possibilities, surgery is the gold standard.
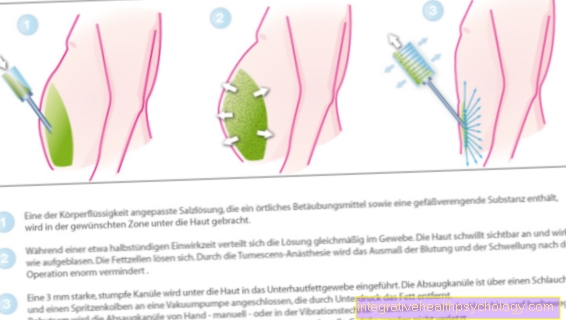
Operation of a basalioma
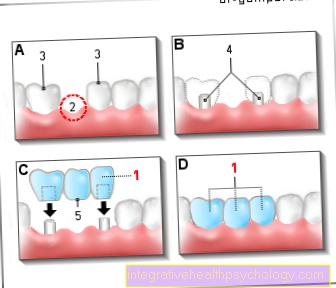
A basalioma can usually be removed quickly and easily by a dermatologist under local anesthesia. If there are recurrences, the basalioma is larger than 5mm, or if it grows in depth, an operation is usually carried out in 2 steps. First, the basalioma is removed with a certain safety margin, then the edges of the specimen are examined for suspicious tumor cells. If there are more tumor cells here, this indicates an incomplete removal of the basalioma, which makes a second operation necessary. Additional healthy tissue around the original basalioma is removed and examined again. In most cases, this can prevent recurrences, i.e. repeated basaliomas.
Radiation therapy for a basalioma
Another form of therapy for basalioma is radiation therapy. With this method, the affected skin area is irradiated with X-rays or proton radiation. This type of therapy is preferred especially for people of older age or poor general condition, for whom an operation would be too risky; for relapses or basal cell carcinomas that are difficult to access for an operation. This mainly affects basaliomas of the eyelids. For cosmetic reasons, radiation therapy is also preferred to surgery for basaliomas of the face. Possible side effects of radiation therapy can be a sunburn-like rash on the treated area, which can, however, be treated well with special creams.
Read more on this topic at: Therapy of a basalioma
Cyrotherapy / photodynamic therapy
Alternatives to radiation can also be the Cyrotherapy (Icing) or the Photodynamic Therapy be, in which special light-sensitive active ingredients are introduced into the skin and which destroy diseased tumor tissue under strong light irradiation, while the surrounding healthy tissue is spared. In kyrotherapy, the basalioma on the ear is frozen using liquid nitrogen. The disadvantage of this method, however, is the later appearance of skin changes, which are difficult to differentiate from a basalioma relapse.
Local immunotherapy and local chemotherapy (cream therapy)
Another, newer possibility of treating a basalioma is that superficial treatment means Imiquimod. Imiquimod is an active ingredient that causes the cell death of diseased tumor cells by means of a local inflammatory reaction and, on the other hand, stimulates the immune system, which helps to reject the tumor cells. Affected skin areas should be rubbed and treated with the Immiquimod cream five times a week for a total of 6 weeks. The treated skin will then redden and crust, which indicates a beginning healing process. In 80% of the cases, the skin would heal free of scars and recurrences after 2-3 months. Since this method is still very new and long-term results are lacking, recurrences after many years cannot be ruled out with certainty. In the meantime, however, therapy with imiquimod has already been approved for small, superficial basaliomas in the facial area, making it a good alternative to surgery.
Another alternative in the therapy of a basalioma is this local chemotherapy with 5-fluorouracil in the form of a cream. Again, the cream should be used for 4-6 weeks. The use of vismodegib is advisable in patients with aggressively growing basal cell carcinomas for whom neither surgery nor radiation is an option. The advantages of this therapy are currently still being discussed.
forecast
Since basaliomas on the ear grow very slowly and rarely metastasize, the forecast for this species from skin cancer good. In more than 90% of those affected, the course of the disease is favorable after therapy. An early operation usually offers the best prognosis with complete healing. In spite of everything but should nevertheless regular follow-up checks because basaliomas can still appear on the surgical scar or in completely different places even after several years.
Prevent
Since the number one cause of white skin cancer, or basal cell carcinoma, is years of exposure to sunlight, the most important method of preventing basal cell carcinoma is one adequate light protection. It should be done regularly Sun protection creams with high sun protection factors which avoid sunburn and thus photodamage to the skin. People with an increased risk of basaliomas (Celtic skin type, genetic desire) should regularly check their skin for basaliomas themselves. Particular attention should be paid to the ears, nose, forehead and scalp and a doctor should be consulted in the case of skin injuries that seem to heal poorly. Since July 1st, 2008 there has been an annual pension scheme for all persons aged 35 and over Skin cancer screening as a cash benefit. During this examination, the entire body is examined for abnormal skin changes.