Appendicitis
Synonyms in a broader sense
- appendicitis
- Appendicitis
- Inflammation of the appendix
- Appendix inflammation
- Pregnancy appendicitis
- Periappendicitis
introduction
Appendicitis is an inflammation of the appendix (appendix vermiformis) of the appendix (cecum). The term appendicitis is therefore not medically correct because it is not the appendix itself that is inflamed, but the appendix of the appendix. Correctly, one should speak of appendicitis.
The "appendicitis" presents with pain in the right lower abdomen, nausea, vomiting and fever. Even now, the diagnosis is still a challenge for doctors and requires quick action in the form of an operative appendectomy (appendectomy). A dreaded and serious complication of appendicitis is the perforation of the appendix, which can be associated with life-threatening inflammation of the peritoneum (peritonitis).

frequency
7% of the population go through acute appendicitis once in their lifetime. It occurs with a frequency of 100 cases per year per 100,000 inhabitants and is 50% that most common cause for suddenly onset strong ones stomach pain (Acute abdomen). The peak of appendicitis is between the 10 and 30 years of age, but schoolchildren are most often ill. Infants and the elderly get sick less often and often have an atypical course, so that the disease is diagnosed later and complications occur more often. Generally the mortality (Lethality) of appendicitis <1%. Appendicitis, which is complicated by peritonitis, has a significantly higher rate Lethality from 6-10%. An early diagnosis is therefore of great importance.
Causes of appendicitis
The blueprint of the appendix is almost predetermined for the development of inflammation. The appendix has a low ability to swell and its small inner diameter (lumen) is predestined for constipation. The importance of the numerous lymphatic tissue in the appendix has not yet been clarified. Appendicitis can be caused by occlusions of the appendix caused by hard feces (fecal stones), kinking of the appendix, strands of scars (brides) and external pressure (tumors and flatulence). Foreign bodies such as cherry, melon, grape seeds can also cause a blockage. Often, local or general infections (viral, bacterial) can cause appendicitis to break out (local decompensation). Examples include tonsillitis, flu, measles, chickenpox or scarlet fever, which mostly affect children.
In very rare cases, parasites such as roundworms can be the cause of appendicitis (appendicitis) be. The bacteria that cause a purulent inflammation when the appendix is blocked are E-coli, preteus, enterococci and belong to the normal intestinal flora. Gastrointestinal flu (gastroenteritis) can also be a possible cause. In very rare cases, Crohn's disease can cause appendicitis.
Read more on the topic: Causes of appendicitis
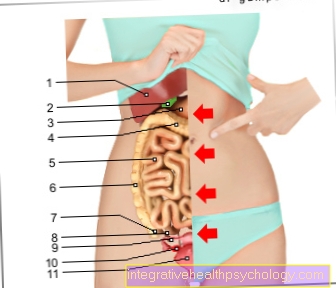
Illustration of appendicitis
- Appendix -
Caecum - Colon, ascending part -
Ascending colon - End part of the ileum -
Ileum, pars terminalis - Free tape strip -
Taenia libera - Appendix -
Appendix vermiformis
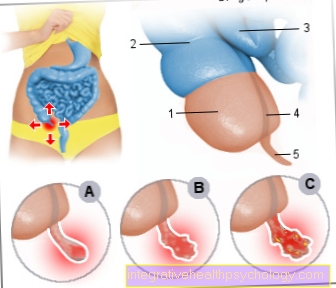
Appendix inflammation -
Appendicitis
A - Catarrhal stage
(The appendix is
swollen, reddened
and painful)
B - Seropurulent stage
(Transition stage between A and C)
C - Destructive stage
- Ulcerophlegmonosa appendicitis -
The mucous membrane shows ulcers.
Beginning of tissue destruction
- Appendicitis empyematosa -
Pus forms in the appendix
- Appendicitis gangrenosa -
The appendix slowly dies.
Gangrene develops
(Tissue destruction)
You can find an overview of all Dr-Gumpert images at: medical illustrations
Symptoms of appendicitis
There are several signs of appendicitis.
In full health, these usually appear very quickly and continue to get worse.
The easiest to spot and first sign is that the person has a stomach ache. These mostly severe pain typically begin around the navel or a little above on the right side, which is initially misinterpreted as stomach pain.
In a short time this pain will then shift to the lower right. This phenomenon is called "Wandering pain" designated.
Position dependency is typical of the pain associated with appendicitis.
This means that, for example, the pain gets worse when jumping, which is explained by the fact that the inflamed and irritated appendix also moves in the abdominal cavity (Concussion pain).
A side difference, i.e. a difference in pain intensity from right to left, also speaks for appendicitis.
To the medical professional, there are some clinical signs that continue to indicate appendicitis.
One of them is the so-called letting go pain. If you press the abdominal wall deeply with two fingers on the left side, i.e. the side opposite the appendix, and let go abruptly, the patient's right side hurts.
The phenomenon known as psoas stretching pain is also typical. When the patient bends the right leg against resistance in the hip joint, it causes severe pain in the right lower abdomen.
The reason for this is the tension in the muscle that lifts the leg and has become very sensitive to pain due to the inflammation. This is interesting for the layman, since the same principle causes pain during normal walking.
For example, pain in the right lower abdomen when walking can indicate appendicitis. A sign that a relative or you can see and feel yourself is tension in the abdominal muscles over the appendicitis (Defense tension).
However, a non-existent sign does not exclude appendicitis any more than an existing one certainly indicates it.
The signs must always be seen in context with other symptoms and the information provided by the sick person.
So there are other signs of appendicitis. Since appendicitis occurs in close proximity to the digestive organs of the stomach, small and large intestines, additional important information is provided nausea and Vomit.
The inflammation and the messenger substances released thereby irritate neighboring nerve fibers and trigger these symptoms. With every appendicitis they appear parallel to the pain.
As a result, many of those affected get involved Loss of appetite observe.
Appendicitis occurs as an objectively measurable sign fever which does not occur, for example, with digestive problems and indicates an inflammatory process.
The temperature is not infrequently 39 degrees Celsius or higher. When measuring fever in the context of appendicitis is often a Temperature difference observed between the rectal and axillary temperature of over 1 degree Celsius, which can also be a sign.
This can be increased Pulse rate to be measured (Tachycardia).
Along with the fever, there is an increased, extremely strong one sweat especially at night, which can be the first sign of appendicitis for outsiders.
It is important to know that almost every appendicitis in young people is associated with a fever. However, it can happen that older people get sick without having a fever.
A possibly occurring Stool retention can be interpreted as an additional sign of appendicitis.
The digestive tract is equipped with a widely branched nervous system, which controls its processes relatively independently. Inflammation affects it and can lead to constipation.
As a difference to this, the opposite is also possible, in which the patient over Diarrhea complains.
What makes it difficult to properly assess the signs is that the location of the appendix in the abdominal cavity can vary from person to person.
Most of them carry it in the right lower abdomen. However, the appendix can also lie in the middle or on the left and even migrate across the horizontal navel line.
This knowledge should be taken into account especially in pregnant patients. Any pain that occurs will otherwise be misinterpreted because of the unusual location.
All these typical signs, without which almost no appendicitis occurs in children and adolescents, are often only seen in a weakened form in older patients.
Some don't even appear.
Appendicitis can occur at any age, but the main age of the disease is school age. A frequency peak can be seen between the ages of five and twelve. The younger the child, the greater the risk of a breakthrough (perforation), so that a small child often has a breakthrough when they are admitted to the clinic.
The classic symptom course of appendicitis with pain in the umbilical area, which in connection with nausea, vomiting and an increase in body temperature moves to the right lower abdomen within a few hours, can also occur in children.
However, especially in children, many deviations from these classic symptoms are possible, which is why it is often more difficult for the examiner to make a reliable diagnosis. Children are more likely to have diarrhea, a high fever, an early deterioration in their general condition, and loss of appetite. In principle, a doctor should be consulted immediately if a child complains of spasmodic pain in the right lower abdomen that lasts longer than three hours, as appendicitis can lead to a dangerous breakthrough. In some cases, however, the onset of symptoms can also occur in the child, which is why even severe pain is not a sure sign of acute appendicitis.
In addition to these clinical, noticeable signs, suspected appendicitis is investigated using other methods. When a blood sample is determined in the laboratory, for example, signs of inflammation such as CRP and white blood cells are increased.
Read more on the topic: Symptoms of appendicitis
Appendicitis and fever
Fever is the body's reaction to the presence of unwanted pathogens. The body temperature increases as the immune system is activated more intensely. Fever is not uncommon in appendicitis, especially in children and adolescents. In older people, fever and other symptoms such as pain and vomiting are less likely to occur with appendicitis. Typically, the fever measured rectally is significantly higher than the temperature under the armpit. The temperature difference is at least one degree Celsius. However, the fever is rarely higher than 39 degrees Celsius. It can also lead to an increased heart rate and night sweats.
Read more on the topic: Abdominal pain and fever
Signs of appendicitis
Appendicitis can announce itself very differently. The signs of acute appendicitis are not always necessarily characteristic of the disease, which is why the differentiation from other causes of the symptoms can sometimes be difficult.
In pregnant women, pain in the right upper abdomen can be a sign of appendicitis. In older people, the symptoms are often not very pronounced, making it difficult to diagnose appendicitis. Often there is also inflammation of the ureter, which can lead to an erroneous diagnosis of an isolated ureter inflammation.
A major symptom of the disease is the clinical symptom change. At first there is pain in the area of the belly button (periumbilical) and in the epigastric region.
Within a few hours, the localization of the pain changes to the right lower abdomen. In many cases, nausea and vomiting occur, and loss of appetite can also be a sign of appendicitis. In more advanced stages of the disease, bowel paralysis (paralytic ileus) come. As with any inflammation, appendicitis can raise the body temperature up to 39 degrees Celsius. Often there is a temperature difference between the measurement in the crook of the arm and the anus. As a result of the fever, the heart rate may increase (Increased heart rate, tachycardia) come.
Read more on the topic: Signs of appendicitis
When should i see a doctor?
If there are signs of appendicitis, a doctor should be consulted as soon as possible. The longer you wait, the higher the risk of a breakthrough and inflammation of the entire abdomen. In children and adolescents between the ages of 9 and 15, with whom appendicitis occurs most frequently, a possible appendicitis should be considered and acted accordingly when the symptoms are concerned.
Read more on the topic: Abdominal pain in children
Recognize appendicitis
Identifying appendicitis is not always easy. There are some typical symptoms that indicate appendicitis, but in many cases there is also an atypical course that makes a diagnosis difficult.
Symptoms of appendicitis often start relatively suddenly within 12 to 24 hours. At the beginning there is often a pain in the area of the belly button, which then moves to the right lower abdomen within a few hours. In many cases there is general malaise, vomiting, nausea and an increase in body temperature. In some cases, appendicitis can be recognized by the fact that there is a temperature difference between the armpit and the anus.
Also constipation, diarrhea or Loss of appetite can speak for appendicitis. Which are often very unclear Upper abdominal discomfort can easily be used for typical complaints one Inflammation of the stomach lining being held. An appendicitis can often be recognized by the fact that a so-called shock pain occurs in the lower abdomen. This increases the pain if the person concerned hops on one leg, for example. Also, in many cases there is Pain on the move, especially when lifting the right leg, there is an increase in pain in the right lower abdomen. For this reason, you can often get a Relieving posture recognize that those affected want to move as little as possible in order to avoid the pain.
At Children and older people It is often even more difficult to recognize appendicitis because, for example, children often experience untypical pain. Older people, on the other hand, often show a mild course of symptoms without fever and without severe pain.
In principle, a doctor should be consulted in the case of persistent, unclear abdominal complaints. For one too experienced examiner It may not be easy to recognize appendicitis immediately. Because of this, there are a number of Testing and Investigations, which make it easier to recognize the disease and can rule out other causes of the symptoms.
Examining the abdomen can provide some evidence of appendicitis. So it often happens in certain places on the stomach Tenderness or to a typical Pain amplification with certain movements. This physical exam in conjunction with a Body temperature measurement, a medical laboratory finding and a Ultrasound examination make it easier to recognize acute appendicitis. Nevertheless, in some cases appendicitis cannot be ruled out with certainty despite unclear symptoms, which is why in these cases it is still considered Precaution a surgical removal of the appendix takes place to prevent possible complications.
What is the difference between appendicitis and appendicitis?
If the appendix is irritated, the appendix or appendix can be irritated for various reasons. Since there are many cells of the immune system in the appendix, infections can quickly develop there due to pathogens. If the appendix is irritated, pain usually occurs in the right lower abdomen, similar to appendicitis. Appendicitis follows irritation if the causes of inflammation persist. If the appendix is irritated, the lower abdomen is usually very tender on pressure.
In the case of appendicitis, on the other hand, typical examinations can be carried out, for example the "contralateral pain of letting go". During this examination, the examiner presses his fingers into the left lower abdomen and when the patient is released, the right lower abdomen is very painful with appendicitis. With appendicitis, the symptoms can be more pronounced than with appendicitis. In addition to pain, there may be nausea, vomiting or fever.
It is advisable to consult a doctor and clarify the cause of the symptoms. With appendicitis there is a risk of a breakthrough in which the inflammatory material gets into the abdomen and can cause an infection of the entire abdominal cavity.
What is chronic appendicitis?
When speaking of appendicitis, acute appendicitis (appendicitis) meant. This must be differentiated from chronic appendicitis. In the case of chronic appendicitis, small acute appendicitis occurs again and again, but it heals by itself. Symptoms are repeated slight pain in the right lower abdomen, impaired digestion and malaise.
However, the repeated slight inflammation can lead to adhesions and sticking in the area around the appendix. If these adhesions are very pronounced, parts of the intestine can become trapped. This creates a mechanical closure of the intestinal passage and digestion and transport in the intestine come to a standstill.
Read more on the topic: Intestinal obstruction - causes, symptoms, therapy, prognosis
With chronic appendicitis there is no risk of a breakthrough, as the inflammation heals up again and again. Accordingly, no surgery is necessary. However, if the intestinal obstruction occurs due to the adhesions, it may have to be treated surgically.
Appendicitis pain
In appendicitis, in addition to the other symptoms, the main focus is on the pain essential psychological stress mean in the patient.
Pain is the first and most important sign of this condition.
For the doctor they are extremely important, since the type and occurrence of the pain are of great importance for the further procedure and the diagnosis.
Appendicitis has a few typical Pain phenomenathat are also used in diagnostics.
The pain usually starts around the belly button or near the stomach. From there they descend to the right lower abdomen within 12 to 24 hours. This as "wandering pain"Phenomenon is characteristic of appendicitis.
The pain can be very severe at the beginning, but it usually starts moderate and increases sharply in the first few hours. They can also subside again and then reappear in the lower abdomen.
Other typical pains associated with appendicitis are described below.
First of all, there is the pain of letting go. (so.).
This maneuver is part of any examination for suspected appendicitis. Furthermore, stroking the large intestine against the natural direction of the food in the direction of the appendix causes severe pain, since here the intestinal contents are pushed back and the appendix hurts due to stretching.
Pain when walking is also often described. This is due to the tension in the muscle that lifts the leg, which is located near the appendicitis and activates the irritated nerve fibers when tensioned.
Due to the different anatomical types of location in the abdomen that the appendix can have, pain is also observed in places other than the right lower abdomen.
While pain is a key symptom of appendicitis, it also occurs with a variety of other events.
However, if the typical pain occurs and it gets worse, a doctor should be consulted, as time is an important factor in the prognosis of appendicitis.
Do you have any other questions about appendicitis pain? Read more about this at: Appendicitis pain
Where is the pain localized?
In appendicitis, the pain usually migrates from the middle upper abdomen just above the navel to the right lower abdomen. However, depending on the position of the appendix, the pain can also be localized in other regions of the abdomen. The appendix can slip behind the appendix and be found there in an ascending position, in which case the pain is more likely to manifest itself in the right flank or back than in the right lower abdomen. The appendix can seldom lie deeper than normal, then the pain is more in the pelvis and pelvic organs can be irritated. If the appendix is higher than normal, the pain is more likely to occur in the right upper abdomen.
Read more on the topic:
- Abdominal pain in the middle
- Lower abdominal pain
- Upper abdominal pain
Back pain
In some cases, appendicitis can cause back pain. Depending on the position of the appendix, the pain can radiate to the lower area of the right back. In the course of the disease, the pain can also move from the upper abdomen to the lower back region.
Read more on the topic: When abdominal pain and back pain occur together
Can you have appendicitis without pain?
Appendicitis can also be mild or without pain. It may be that the person concerned only feels a slight pulling in the lower abdomen or pain only occurs when pressure is applied to the abdomen. This is especially the case with the elderly. However, appendicitis usually begins with pain in the middle upper abdomen a little above the navel, which then migrates to the right lower abdomen. The pain can be felt differently depending on the person.
Read more on the topic: Pulling in the lower abdomen - these are the causes!
Diarrhea associated with appendicitis
diarrhea (Diarrhea) is a typical symptom at a variety of Gastrointestinal diseases. One speaks of diarrhea if watery, ungrounded or mushy stools occur more than three times a day. The leading cause of diarrhea are Viruses (e.g. "Abdominal influenza"or traveler's diarrhea). Also Medication, food or certain diseases like inflammatory bowel disease can cause diarrhea.
Even acute appendicitis can lead to diarrhea. In contrast to the other causes of diarrhea, typical symptoms of appendicitis often occur at the same time. Painthat initially appear in the navel area and quickly migrate to the right lower abdomen, as well as nausea and Vomit, fever, Loss of appetite and a deterioration in general well-being in connection with diarrhea can indicate acute appendicitis. Diarrhea is not a classic symptom of appendicitis, however, as the condition is common atypical symptoms appendicitis should be considered even if diarrhea is acute.
diagnosis
A typical or "classic" combination of symptoms is very rare in appendicitis. Often there are diffuse complaints that initially do not allow a clear diagnosis. The history (anamnesis) of the person concerned is an important criterion for the diagnosis of appendicitis. Typically, the history is relatively short, with brief periods of abdominal pain, nausea, and vomiting reported.
Since appendicitis is a relatively common disease, it can be considered as a diagnosis if only a few, but typical symptoms appear. A physical exam will then be performed. This can corroborate suspicion of appendicitis very quickly, as there are a number of tests and examinations that indicate the disease.
If the physical exam shows nothing abnormal, there is a high probability that appendicitis can be ruled out. In addition, a laboratory test is carried out for the diagnosis, in which, for example, in appendicitis almost always an increase in white blood cells (Leukocytosis) can be determined. The body temperature is measured and, if possible, an ultrasound examination (Sonography) carried out. A thickened appendix can often be seen on sonography, which could indicate appendicitis. However, even with an inconspicuous ultrasound examination, acute appendicitis cannot be completely ruled out.
Rather, sonography serves to exclude other diseases that can cause symptoms similar to appendicitis, including kidney stones and other diseases of the kidney and ureter as well as gynecological diseases. The most common is a so-called "gastrointestinal flu" (gastroenteritis) as an alternative diagnosis. But also various other diseases must be ruled out before the diagnosis of "appendicitis", especially before the indication for an operation is made.
In particularly bad cases, an MRI of the abdomen may also be necessary.
Read more on the topic: Diagnosis of appendicitis, ultrasound of the abdomen
Tests for suspected appendicitis
There are a number of tests that can be done to confirm suspicion of appendicitis. A clear diagnosis cannot be determined by these tests and in some cases a negative test does not rule out appendicitis.
For example, this is a simple test Hop on one leg. If you have appendicitis, the shock from jumping can cause a Amplification of pain come in the belly.
There are also a number of different ones Pressure pointsthat are palpated during the clinical examination of the abdomen. When touching certain areas of the lower abdomen (Mc Burney Point, Lanz Point) in the case of appendicitis, severe pain is often triggered.
Most often it is appendicitis located on the right. The so-called Blumberg test pressure is exerted on the lower abdomen on the left side with the examiner's hand and suddenly released again. The test is positive and can indicate appendicitis if pain develops on the right side of the appendix.
In some people, the appendix is also folded back. In the case of inflammation, pain occurs when the right leg is flexed in the hip joint against resistance. This test (so-called psoas stretch pain) can also provide indications of appendicitis. The Ten Horn test can be done in men by actively pulling down the testicle. If there is then pain in the right lower abdomen (Mc-Burney point), the test is positive.
The Old age appendicitis is rarely found at 5-10% and is characterized by one creeping course out. Because of the frequent carryover rate, peritonitis is particularly common in this group of patients.
An appendicitis during the pregnancy is particularly difficult to see, as the appendix and appendix move upwards as the uterus grows. This means that depending on the month of pregnancy, the appendix pain at an atypical location (right upper abdomen) localized, which can lead to misdiagnosis.
Appendicitis During Pregnancy - What To Do?
Caution should be exercised with abdominal pain during pregnancy. The tricky thing about appendicitis during pregnancy is that the symptoms can easily be mistaken for pregnancy symptoms. In the event of abdominal pain, vomiting, nausea and fever during pregnancy, a doctor should definitely be consulted. Symptoms such as loss of appetite, paleness, or sweating may also occur.
Read more on the topic: Abdominal pain in pregnancy
Usually the pressure sensitivity, which is a clear sign of appendicitis in other people, is not present in pregnant women. The position of the appendix can also change during pregnancy, especially towards the end of pregnancy. Accordingly, the pain is no longer in the right lower abdomen, but rather in the right upper abdomen.
Read more on the topic: Appendicitis in Pregnancy
As with most appendicitis, surgical removal of the appendix is the treatment of choice. If the surgical treatment is delayed too long, there is a risk of a breakthrough and inflammation of the entire abdominal cavity, which can be life-threatening. There are two surgical methods, either minimally invasive using three small skin incisions or an open operation. Nowadays the operation is mostly minimally invasive. There is always a basic risk of complications during an operation, but the risk of appendicectomy for both mother and child is low.
Read more on the topic: Anesthesia during pregnancy - important information
Duration of appendicitis
The duration of appendicitis can vary from person to person. For some, appendicitis begins with slight pain in the upper abdomen, while for others, severe pain starts at the beginning. Depending on the severity of the discomfort, you may wait to see a doctor at the beginning. In this case, the duration depends on how quickly the person concerned visits a doctor and how quickly he or she initiates the next steps after clarifying the cause.
An inflamed appendix should be surgically removed. The operation takes about 20 to 30 minutes, depending on whether it is open or minimally invasive. If no surgery is performed, appendicitis can take 48 hours from the onset of symptoms to the breakthrough or death of the appendix tissue. However, this duration also varies from person to person.
Also read: Duration of appendix irritation
How long have you been sick with appendicitis?
The length of the disease duration depends on the time of diagnosis. If the symptoms of appendicitis are present, a doctor should definitely be consulted. The longer the visit to the doctor is delayed, the more unpleasant the symptoms and the higher the risk of life-threatening peritonitis.
Surgical removal of the appendix is usually useful. After the operation, the affected person often recovers quickly. From the second day after the operation, diet with light foods is usually possible again. The length of stay in hospital is usually three to five days. Depending on the surgical method, two to six weeks of rest are important.
Read more on the topic: Post-operative care
The operation for appendicitis
Appendicitis does not always have to be treated with surgery. In principle, a wait-and-see, conservative treatment with observance of bed rest, the administration of antibiotics, laboratory tests and a temporary abstinence from food (Food leave) possible. This procedure is intended to avoid unnecessary surgical interventions, but there is a fundamental risk of aggravation and further progression (Aggravation) the disease.
However, if acute appendicitis cannot be ruled out with sufficient certainty, an operation is generally indicated. Of course, an operation under general anesthesia is always associated with a risk of complications. However, this risk is considered to be lower than the removal of the appendix in acute appendicitis.
In an appendix operation, perforation (breakthrough) of the appendix released into the free abdominal cavity. The intestinal walls of the appendix are torn due to the death of tissue (necrosis). The intestinal contents flooded with germs can spill into the abdominal cavity and there an often life-threatening peritonitis (Peritonitis) cause. The occurrence of such peritonitis without surgery is associated with a mortality rate (Lethality) of up to 30 percent, which is why the indication for an operation in acute appendicitis is very generous in order to prevent this consequential damage.
Read also on this topic Ruptured appendix
The operation of appendicitis is called appendectomy, which means the removal of the appendix on the appendix. There are two different surgical techniques, a distinction is made between conventional and laparoscopic appendectomy.
In conventional surgery, the surgical approach is selected using a so-called alternating incision on the right lower abdomen. First, after a short oblique incision of the skin, the fibers of the abdominal muscles are pushed apart according to their direction of fiber orientation and the peritoneum is opened. Opening the abdominal cavity through an incision in the abdominal wall is known as a laparotomy. The surgeon has direct access to the internal organs and can perform the operation under direct vision.
The second surgical technique, which is known as laparoscopy or minimally invasive surgery, differs from this. For laparoscopy, only a minimal skin incision (about one centimeter long) just below the navel and two even smaller so-called "Work access"on the lower abdomen. Using the keyhole principle, special devices to which a video camera and a light source are connected can be inserted into the abdomen and the operation can be carried out. The smaller cuts and injuries in this approach usually result in less pain after the operation and also for a faster recovery.
Incisional hernias are less common after laparoscopy compared to the conventional method (Incisional hernias) and the rate of wound healing disorders is lower. Disadvantages in some cases are the poor clarity of the surgical field and the delayed accessibility in the event of a threatening complication such as heavy bleeding in the surgical area. In addition, the need for equipment is lower in conventional surgery (the costs for the two procedures differ only minimally).
After access to the inflamed appendix has been established, the operation proceeds very similarly for both surgical techniques. First, the blood supply to the appendix is interrupted and the appendix is severed and removed at the transition to the appendix. If there is severe inflammation of the appendix, a temporary drain can be placed to drain the wound secretion from the abdomen.
Typical complications associated with appendectomy, in addition to the general risks from the anesthesia, are, for example, a defect (insufficiency) the suture on the intestine, which causes purulent peritonitis or abscess (Pus cavity) can come. Furthermore, wound infections can occur, especially if the appendix ruptures and pathogens are spread into the abdominal cavity as a result. There is a risk of adhesions, which can occasionally lead to a bowel obstruction (Ileus) can lead. The operation can also lead to bleeding and injuries to the ureter, intestines or other neighboring organs.
The prospect of healing (forecast) is very good for an appendix operation. In the case of a non-perforated (openwork) Appendicitis, the mortality rate is below 0.001 percent and is therefore very low. If the inflammation has already perforated, the mortality rate is around one percent due to the increased risk of complications.
If acute appendicitis is suspected, the operation should be carried out as early as possible. An operation should be carried out within about 48 hours to prevent the inflammation from breaking through. In most cases, there are no further risks for those affected by surgery within the first 48 hours of illness.
Read more on the topic: Appendicitis surgery and therapy for appendicitis
Variations in the position of the appendix
Variants of the appendix:
- Regular
- Paracecal: To the right of the appendix
- Retrocecal: Behind the appendix on which Iliopsoas muscle lying on top
- Paraileal: Turned up in the direction of the ilium (ileum)
- In small Basin: Very long appendix, reaching into the small basin
- Cecum depression: The appendix and appendix lies in the small pelvis
- Zecum high stand: The appendix with appendix lies in the right upper abdomen
- (pregnancy)
- Situs inversus: Very rare anomaly of the human body in which all organs are mirror-inverted in the body. The appendix is thus in the left lower abdomen.
Course of appendicitis
Typical appendicitis can be divided into stages of inflammation:
1. Catarrhal stage: the appendix is swollen, red and painful. There is no pus yet and this stage is still fully reversible (reversible).
2. Seropurulent satdium: This is a transition stage between 1 and 3
3. Destructive stage: 3 stages are distinguished:
- Ulcerophlegmonosa appendicitis: The mucous membrane shows ulcers. Beginning of tissue destruction.
- Appendicitis empyematosa: pus forms in the appendix
- Appendicitis gangrenosa: The appendix slowly dies. A gangrene (tissue destruction) develops.
If there is an obstacle to emptying in the appendix, the secretion and feces build up in it.
The appendix swells, turns red, and the first painful event occurs. The first symptoms of appendicitis develop within 12-24 hours.
The bacteria occurring in the appendix can then multiply strongly in the standing secretion. Due to the swelling of the appendix, the blood vessels are gradually squeezed, so that an insufficient supply of oxygen is created for the tissue. The tissue slowly dies and the bacteria can break through the mucosal barrier.
When, after about 48 hours, they pass through the last layer of the intestinal wall, the serosa, the surrounding peritoneum (peritoneum) infected with (periappendicitis, local peritonitis) which then spreads throughout the peritoneum (peritoneum) can spread.
Read more on the topic: Gangrene
Complications
Appendicitis is a life-threatening condition and should be diagnosed and treated as soon as possible.Some serious complications can arise from delayed diagnosis of appendicitis.
- Free perforation: In the case of a damaged intestinal wall and severe swelling, the appendix wall can break through and the contents penetrate into the abdominal cavity (peritoneum). The bacteria released in this way can cause severe diffuse inflammation of the peritoneum (peritonitis).
- Perityphlitic abscess: If the perforation cannot spread any further due to the surrounding adhesions, a pus cavity develops in the vicinity of the worm cot.
- Conglomerate tumor: This is not a real tumor ("cancer"). The inflammation can cause the surrounding structures such as the appendix, large mesh (greater omentum) and loops of the small intestine to stick together to form a tumor.
- Abscesses: If pus forms in the abdominal cavity, encapsulated abscess cavities (pus cavities) can develop. Predestined locations for abscesses are between the loops of the small intestine (interenteric), under the (diaphragmatic subphrenic), under the liver (subhepatic) and especially in the so-called Douglas space. In women, this space lies between the rectum and the uterus.
- Thrombophlebitis of the portal vein: If the inflammation of the peritoneum spreads to the portal vein system, phlebitis develops, which is often associated with thrombus formation in the portal vein.
- Paralytic ileus: In the case of inflammation of the abdominal cavity (peritonitis), reflex intestinal paralysis can occur. As a result, bowel movements (peristalsis) can no longer be performed. A transport stop of the intestinal contents occurs, a so-called ileus.
You might also be interested in:
- Abscess in the intestine
- Ruptured appendix
When do i need antibiotics?
Antibiotics are drugs that can be used against inflammation caused by bacteria. Depending on the cause of appendicitis, the use of antibiotics can be useful. Clogging of the appendage with excrement stones, kinks or foreign objects such as fruit pits can lead to bacterial inflammation in the appendix. In mild cases of appendicitis, it can make sense to give the affected person antibiotics to fight the infection. In this situation, the operational risks would be eliminated.
In complicated cases, in which a breakthrough and thus a life-threatening peritonitis threatens, the appendix should be surgically removed. Antibiotics can also be used after an appendix has been removed, for example for wound infections.
Which antibiotics are used?
Depending on which bacterial pathogen is responsible for the inflammation, different antibiotics can be used. Beta-lactam antibiotics, which prevent the bacteria from building up the cell wall, are usually used. Amoxicillin is often given together with clavulanic acid. The antibiotic cefotaxime can also be used. As soon as symptoms arise, the person concerned should consult a doctor and the decision whether and, if so, which antibiotic should be used, should then lie with the doctor.
Read more on the topic: Side effects of antibiotics
Home remedies
If appendicitis is present, the appendix should definitely be surgically removed, as there is a risk of life-threatening peritonitis. However, there are various home remedies to relieve the symptoms of appendicitis. For example, castor oil stimulates digestion and can be taken in the case of constipation or placed on the stomach as an envelope. Ginger tea and garlic have anti-inflammatory properties and can help relieve the pain and nausea associated with appendicitis. Lemon and mint can also stimulate digestion and reduce pain.
Appendicitis in the child
Appendicitis in children is of great importance as the majority of the observed cases occur in children and adolescents. Every year around 28,000 children up to the age of 15 visit a hospital in Germany because of appendicitis, 38% of all appendectic removals are made by the group of 5 to 19 year olds.
As a rule, children under two years of age do not become ill, boys are more often affected than girls.
However, diagnosis is often more difficult in children than in adults. On the one hand, this has to do with the fact that a child complains more often of stomach pains, which are usually harmless. Parents can therefore dismiss the child's pain as a banality when having more serious problems.
On the other hand, a child cannot communicate in as differentiated a way as older people. However, the type and occurrence of the pain are important indicators of suspected appendicitis.
However, you will quickly notice whether it is normal abdominal pain or whether the child is writhing in pain.
If the pain remains for more than three hours and gets worse, you should have the matter clarified due to the frequency of this disease in the child.
Other typical signs of appendicitis in children are extreme sensitivity to touch and refusal to eat. Even if a child plays less than normal, this can be interpreted as a sign of appendicitis.
Curled walking and lying down is observed in children to relax the tense and sore abdominal wall. This immune tension does not occur, for example, in gastrointestinal infections.
Fever is often added. In toddlers, the symptoms may be less severe, making diagnosis even more difficult.
In any case, it is important to always monitor the child's abdominal pain and to pay attention to the child's behavior.
Treatment always consists of an operation in which the appendix is removed. Nowadays, in contrast to the open surgery that was common in the past, the minimally invasive "Keyhole surgery" applied.
Appendicitis can be treated well with just a small incision, usually on the navel without a scar that will be visible later.
Also read: These are the symptoms I can tell if the child has cervical inflammation
Is appendicitis contagious?
Appendicitis is not contagious. The bacterial inflammation in the appendix can be caused by laying it with feces or foreign bodies such as fruit pips, as well as kinking or pressure from the outside. However, the infection is limited to the appendix and cannot be transmitted from person to person.