Cortisone in pregnancy - how dangerous is it?
introduction
Cortisone is a naturally occurring glucocorticoid in the body that is produced in the adrenal gland. It is increasingly released during stress and strain and leads to an increased supply of energy reserves as well as an inhibition of the immune system and inflammatory reactions.
The various synthetically produced glucocorticoid preparations (colloquially referred to as cortisone) can be administered in the form of tablets as well as ointments or sprays and are widely used in medicine. Glucocorticoids are often used in the therapy of bronchial asthma, rheumatic diseases, many inflammations in the ENT area and in the skin area. Continuing the therapy during pregnancy is often essential.
Read more on the subject at: Effects of cortisone

Who Needs Cortisone During Pregnancy?
Glucocorticoids are the best studied anti-inflammatory drugs during pregnancy. All in all, according to study results, it can be stated that treatment with glucocorticoids during pregnancy With the correct dosage and use, there is very little risk to mother and baby consists.
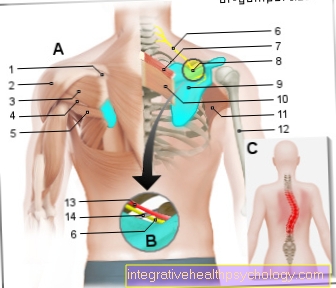
Glucocorticoids can be used for many different conditions during pregnancy. Especially for Treatment of asthmatic and rheumatic diseases as well as for Avoidance of transplant rejection Continuing therapy is often essential. The inhibition of the immune system in the context of autoimmune diseases is also possible with glucocorticoids. In addition, the Therapy of skin diseases (e.g. atopic dermatitis, eczema, etc.) often during pregnancy. Alternative medication can only be used in rare cases. For the treatment of the various diseases during pregnancy, there are often specially developed schemes in which dosage should be continued.
Stopping cortisone therapy often poses a greater risk to the pregnancy and the baby than continuing treatment.
How does cortisone affect my child?
The effect of the various glucocorticoids on the child depends on the preparation used and how it is taken. Basically, cortisone effects similar to adults when it enters the baby's circulation. When using ointments and sprays, in contrast to therapy with tablets, only small amounts of cortisone enter the mother's circulation and consequently the child's circulation.
The most commonly used glucocorticoid supplements Prednisone and prednisolone only have a very weak effect on the child's body. This is due to the fact that these preparations are largely inactivated in the placenta (placenta) area. Only about 20% of the amount of cortisone in the mother's blood reaches the child's bloodstream. Possible effects on the development of the child are therefore only with a very high dosage (more than 15 to 20 mg a day) and with long-term use to fear.
In addition, glucocorticoid preparations are commonly used Dexamethasone and betamethasone. Compared to the preparations mentioned above, these are not inactivated in the placenta area and reach the bloodstream in high doses of the child. For this reason, they are used for rare indications during pregnancy. On the one hand they find Use for threatened premature births or very early labor.
The preparations are injected in high doses in the last third of pregnancy. They cause the child to develop more quickly, which significantly increases the probability of survival in the case of premature births. It is above all that cortisone-dependent maturation of the lungs crucial at the end of pregnancy. In addition, study results have shown that this therapy leads to less occurrence of cerebral haemorrhages and neurological failures in premature births.
On the other hand, the preparations for Avoidance of congenital cardiac arrhythmias injected (congenital AV block). In the context of isolated rheumatic diseases in the mother, there is a risk that the development of the conduction of excitation in the baby's heart can be disturbed. Treatment with dexamethasone and betamethasone can significantly reduce this risk.
Side effects for my child

The possible side effects that can occur during treatment with glucocorticoids are strongly dependent on the dosage, the type (tablet, ointment, spray) and the duration of use. It should be noted that the individual glucocorticoids have different strengths (potency). Side effects are to be feared especially with long-term therapy with high-dose glucocorticoids in the form of tablets. Nevertheless, the occurrence of side effects is very rare.
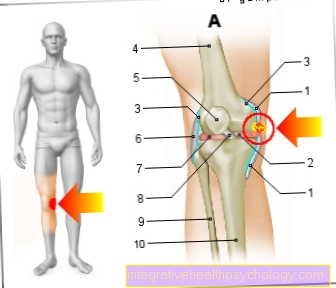
During the first trimester of pregnancy, high-dose, long-term therapy (more than 15 to 20 mg per day) carries the risk of developmental disorders for the child. The increased occurrence of cleft lip and palate when taken between the 8th and 11th week of pregnancy is discussed. In addition, there can be indirect risks for the child, as the very high doses favor gestational diabetes, high blood pressure or eclampsia.
Read more on the subject at: Pregnancy Hypertension - Is It Dangerous?
During the second and third trimester of pregnancy, there is a risk of growth disorders and premature births with high-dose, long-term therapy. Insufficiently low sugar levels in the baby's blood as well as low blood pressure and electrolyte disorders can also occur in exceptional cases. In addition, at the end of a pregnancy there is a risk of adrenal insufficiency, as the high glucocorticoid levels inhibit the natural production of cortisone in the child's body.
Risks to my child
With low-dose and short-term therapy with glucocorticoids there are few risks for the baby. When taken between the 8th and 11th week of pregnancy, study results have a slightly increased risk of cleft lip and palate while the overall rate of malformations is normal. It should be noted that increased cortisone levels are only one of many contributing triggers. In addition, there is a risk of premature birth and growth disorders with cortisone therapy. A continuation of a high-dose glucocorticoid therapy should therefore always be discussed with the attending physician regularly checked with an ultrasound device become.
Dosage of cortisone in pregnancy
Different dosages are used depending on the disease being treated. In many diseases, low daily doses of between 1 and 10 mg are possible. The dosage of long-term therapy is given with the unit prednisolone equivalent - it indicates the strength of the active ingredient in comparison to the common prednisolone.
During pregnancy, continued glucocorticoid therapy at low doses (less than 10 mg) is possible without risk. Even a single injection of very high doses (up to 100 mg) does not have to be dispensed with in emergencies and in the case of acute attacks of an illness. In the case of high-dose long-term therapy (more than 15 to 20 mg per day over a long period of time), the treatment should be discussed with the attending physician and the child's development should be regularly monitored with the help of an ultrasound device.
Alternatives to cortisone
Compared to many other drugs are available for glucocorticoids no or few preparations as an alternative to disposal. The strong anti-inflammatory effect is not achieved with the help of herbal products. In addition, other drugs that inhibit the immune system usually have a significantly higher side effect profile. If necessary, a different daily division of the intake of the medication can lead to a constantly lower effective level.
To continue cortisone therapy during pregnancy, you should therefore take prednisone or prednisolone. Due to inactivation in the placenta, only a very small amount of the active ingredient reaches the child's bloodstream.
Application forms of cortisone in pregnancy
Can I use a cortisone cream or ointment during pregnancy?
When using a cortisone ointment or cortisone cream, there is only one very little risk to the child. With a locally limited application, only a very small proportion of the active ingredient enters the mother's blood through the protective barriers of the skin. When using ointments or creams that contain prednisone or prednisolone, this proportion is also largely inactivated in the placenta. Therapy with cortisone cream or ointment can therefore usually be continued during pregnancy. A Consultation with the attending physician is always required anyway.
Can I use a cortisone spray during pregnancy?
The cortisone spray used in the context of asthma diseases can also be used during pregnancy. Similar to the use of ointments and creams, the glucocorticoid amount of the spray gets in only to a small extent in the mother's and child's circulation. For safety reasons, it may still be advisable to use another non-cortisone spray. Therefore, further use during pregnancy must always be clarified with the attending physician.
What about cortisone and the desire to have children?
Taking cortisone when trying to have children is controversial. The glucocorticoid is said to have a slightly supporting effect in the implantation of the fertilized egg cell. The mechanism of action and the effectiveness are not clear despite the implementation of several studies. A possible suppression of the release of hormones and messenger substances by the immune system is suspected to be the cause.
Still it is Administration of cortisone is not indicated in all women wishing to have children. In the case of hormone-related miscarriages or an already damaged uterus, taking cortisone to support pregnancy can be discussed with the attending physician. Regular monitoring of potentially possible side effects is necessary during this intake.
Cortisone for lung maturation
During normal pregnancy, cortisone is produced in the adrenal glands in the last few weeks of pregnancy. This formed cortisone contributes to Maturation of the lungs and prepares the child for the first breaths after birth. Cortisone acts as a kind accelerating factor in the development of the lungswhich often do not fully mature until the last few days before giving birth.
Because of this, cortisone can too can be used in the event of a premature birth or premature laborto support the not yet fully formed lungs in their development.
Does cortisone lead to increased stretch marks during pregnancy?
Stretch marks (stretch marks) can appear for many different reasons. A Overstretching of the connective tissue of the skin (e.g. in the event of rapid weight loss or during pregnancy) can lead to irreversible cracks in the subcutaneous tissue. These are expressed by reddish blue stripes that turn increasingly white over time.
In addition to these natural reasons for the development of stretch marks, the use of some medications can also contribute to the development. Among other things Regular use of cortisone can increase the development. In this case, preventive skin care is helpful.