The shin splints
synonym
Medial tibial stress syndrome, periostitis, shinsplints, ventral or dorsal tibial edge syndrome, functional compartment syndrome

definition
At a Shin splints it is a chronic pain syndrome in the area of one or more fascial compartments of the lower leg due to disproportions between muscles and fascia that arise during exercise.
Diagnosis of tibial splint syndrome
An indication of a tibial splint syndrome is the information provided by the patient that the symptoms begin after a running distance of approx. 500 m and are still present after the exercise. The physical examination reveals a swollen skin or muscle in the middle and lower 2/3 of the tibia. The pain usually gets worse when you apply pressure. Both of these symptoms appear especially after previous physical exertion.
If the shin splints are severe, abnormal sensations in the skin in the area of the shin can also be detected. In most cases, the corresponding complaints are then expressed by the patient on request. With a tuning fork you can then also show the indicated discomfort.
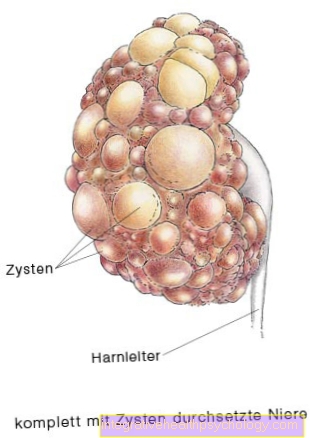
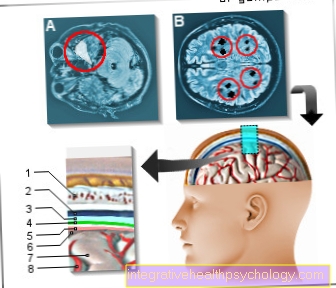
Imaging methods are also used for diagnostics, but these only address other causes of the complaints, such as Rule out osteoarthritis or stress fractures. Conventional X-rays are used for imaging (Exclusion of a fracture) or an MRI for use.
While X-rays can mainly see bone involvement, magnetic resonance imaging (MRI) can also make edematous swellings of the muscle visible. If necessary a scintigraphy of the skeleton can also be performed. This shows an increase in storage, especially after a long tibial syndrome, which can be interpreted for inflammatory processes in the area of the muscle. Neurological examinations such as Investigations of the nerve conduction velocity (NLG) are only used in extreme and difficult processes. The safest way to diagnose shin splints is to measure the pressure in the muscle compartment on the one hand before exercise and on the other hand after exercise.

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Symptoms of Shin Splint Syndrome

symptoms of the Shin splints Pain is mainly possible, initially when moving, later also when resting.
The painful nature of a tibial splint syndrome is described as drawing to burning or stabbing. Sometimes it is located in the area of the place of origin, sometimes it is passed on to the hip or to the foot.
Due to the excessive pressure in the affected compartments, the skin is elastic over the affected area. The skin tension can also cause pain. In some cases, patients also complain of sensitivity disorders in the area of the tight skin.
In advanced stages, discomfort occurs not only when moving, but also at rest. The excessive pressure on the muscles and the necrosis that may arise can also lead to functional restrictions in certain muscle movements. Necrotizing muscle regions can also lead to a general systemic inflammatory reaction with high levels of inflammation fever and Exhaustion, possibly also to a Blood poisoning (sepsis) to lead.
Causes and forms of shin splints
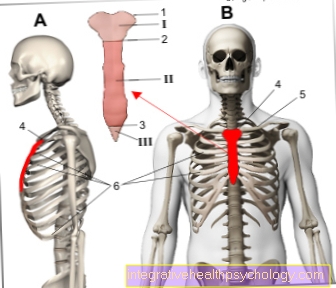
The muscles of the lower leg run in boxes, which are also known as compartments.
Each muscle is enclosed by a thin but extremely stable skin, the muscle fascia. A shin splint syndrome occurs when the muscles of the lower leg increase through training and there is an increased pressure ratio in one or more boxes.
A corresponding training effect occurs primarily during muscle training, but also through sports and the associated muscle movements. If the muscle increases and the pressure in a compartment rises as a result, the muscle may be insufficiently supplied with oxygen-rich blood, as the vessels supplying the muscle are increasingly compressed and allow less blood to pass through.
The blood that builds up in the vessels now causes increased pressure.
This leads to the leakage of fluid from the vessels and thus to the formation of edema around the vessels. This in turn increases the pressure in and around the muscle. A vicious circle begins. This can lead to the death of muscle cells - so-called necroses. The muscles of the so-called deep medial compartment are particularly often affected by tibial splint syndrome. These include the tibialis posterior muscle, flexortorum longus muscle and flexor hallucis longus muscle. These muscles serve to tension the foot longitudinally and transversely and form the arch of the foot. Excessive running, especially on hard surfaces, can lead to a pronounced compartment syndrome and massive discomfort.
Read about this too: Tendinitis of the tibialis posterior tendon
Duration
The individual Duration of complaints shin splints can vary widely. Depending on the degree of the disease as well localization and root cause the symptoms can last anywhere from a few hours to several weeks. Typical are pains that always occur at the beginning of the training and improve in the course of this. The longer a shin splints lasts and is not treated, the more consistently the pain is perceived. Especially when the skileg If the disease does not occur, the duration of the illness can be significantly increased. An individually tailored therapy can help to shorten the course of the disease. A timely visit to one doctor right at the beginning of the symptoms is essential for a rapid healing of the disease.
Should be using conservative methods of treatment The disease cannot be cured for a long time, a operative treatment be considered.
During muscular training, the muscle can take up to 15 times its original volume. Especially when the muscles are trained quickly, the muscle fascia around the muscle cannot adapt to it as quickly - a compartment syndrome (Shin splints) arises.
Besides the general Weight training The following sports techniques in particular are considered to be beneficial factors for shin splint syndrome:
When changing the floor covering, both in spring and in autumn, the muscle groups can become overburdened, and intensive training on hard surfaces is also beneficial Shin splintsFurthermore, intensive running training with repetitive jumping and landing maneuvers as well as excessive forefoot loads. In addition, malpositions of the feet with simultaneous training can promote a shin splint syndrome. The misalignments include external rotation and Pronation. If the sports training is increased abruptly or the training regime is changed, if a frequent shoe change is made or spike shoes are used, shin splints can occur much more frequently.
therapy
In the treatment of shin splint syndrome is one conservative from one operational Differentiate therapy.
With conservative therapy, the sports leading to the symptoms should first be stopped for a long time and the leg should be spared.
Alternatively, do sports, such as swim or To go biking (Stepping on the pedal with the heel). To reduce the swelling of the Leg can cooling compresses be put on. Medicinally, anti-inflammatory drugs can be administered in the form of ointments or tablets.
If there is no improvement, you can try a cortisone solution (Cortisone) into the muscle compartment.In addition, a conservative treatment approach can be tried through physiotherapy, in which the periosteum is exercised with gentle but steady pressure.
Surgical therapy is always induced if there is no improvement in conservative treatment attempts or if the pressure conditions increase so much that the supply of the muscles with oxygen-rich blood is endangered. During the surgical procedure, the fascia of the affected muscle is split in order to reduce the dangerous pressure. The procedure can either be carried out as an open operation, but is also increasingly being carried out in endoscopic procedures. Sport can be practiced approx. 4 weeks later. The chances of success are good. About 60-100% of the patients are symptom-free after the procedure.
Taping
Sports tapes or Kinesio tapes are used for a wide variety of diseases that cause the Musculoskeletal system affecting people. When pain is in the foreground of the Symptoms the treating physician is very often asked by the affected persons about the possibility of applying a tape bandage. In general, it should be noted that taping in most diseases, as well as in shin splints, is a very controversial therapy option represents. At severe discomfortcaused by shin splints should other therapy options are in the foreground and the tape can be used as an additional treatment method. As a rule, use will not cause damage if the prescribed and recommended therapy is carried out at the same time. Since individual cases are known in which the use of the tape in an existing shin splint syndrome brought improvement, it is certainly possible to try out this option.
Tape can help with shin splints if it is known individual running style the emergence of the syndrome co-favored. Especially with one Running style with noticeable pronation In the rolling movement there is a risk of a tibial splint syndrome. By applying a tape bandage, the irritated muscles in certain circumstances stabilized and the Running style improved become. Whether the bandage makes sense individually and leads to an improvement in the symptoms should be discussed with a specialist Orthopedists or Sports medic be discussed. He or she can best assess the severity of the disease and the potential therapeutic success that can be achieved with the tape and give a recommendation.
Read more about this topic at: Kinesio tape
bandage
At a Bandage for the shinhow to treat one Shin splints is used, it is a piece of cloth that is wrapped around the affected shin. The bandages are relative stable and are usually intended for Sports injuries help to stabilize the affected structures. It is recommended to use the correct amount of bandage to ensure that the bandage is neither too tight nor too far around the shin and can achieve the desired effects in the treatment of the shin splints. As with a shin splints no joint involvement is present is a Stabilization usually not necessary.
Still, a bandage can help reduce the symptoms of the syndrome somewhat. This is especially the one caused by the bandage Heat development and one with it improved blood circulation attributed.
Although a bandage can help reduce the symptoms, this should not be used as an opportunity to continue to strain the shin. Because the bandage in no way the root cause Can treat shin splints, irritation of the structures should be avoided even when using the bandage. A clarification by one doctor is recommended when symptoms begin to develop so that the disease progresses as favorably as possible. The sole treatment of the tibial splint syndrome with a bandage without consulting a doctor and a possible further stress on the structures of the Lower leg can to serious consequences lead and should be avoided. Are specialists in the treatment of shin splint syndrome Specialists in orthopedics and medical professionals who specialize in the treatment of sports disorders. They can best assess the individual sense of using the bandage and at the same time explain further therapy options.
ointment

The therapy with a ointment can be assigned to the conservative approach to treating this condition. The ointments are on the painful area and are intended to help relieve symptoms of the condition. A causal therapy The use of ointments can be used for shin splints Not Tobe offered. The cause of the emergence of the complaints is relatively deep below the skin which is why the active ingredient of the ointment usually cannot penetrate from the skin to there. Most of the active ingredients found in ointments are used by the Lymphatic system absorbed and distributed over this in the body until it can act in the desired place in a diluted form.
The Painkiller Diclofenac can using an ointment local are used and is often used in the therapy of shin splints. Pain can be effectively treated by applying the ointment. Another option to treat the symptoms with an ointment is with the help of a Warming ointment. These ointments increase blood flow to the skin and can often provide some relief from the pain caused by tibial splint syndrome.
The application of Cortisone ointments becomes not recommended and does not belong to the therapy of the disease. The desired anti-inflammatory effect cannot be achieved through the local application of the active ingredient. However, the agent can be used in special cases intramuscular be injected.
Massages
Massage as a physiotherapeutic measure can effectively alleviate the symptoms of tibial splint syndrome.
Massages are especially useful when the pain does not come from the muscles, but from the periosteum. With the help of a special massage technique, the pressure load on affected structures, such as the periosteum, is reduced.
One possible type of massage is ice massage. This is particularly helpful in the acute stage, as the cold can relieve the symptoms of inflammation. To do this, you can wrap several ice cubes in a washcloth or towel, for example, and use them to carefully massage a particularly painful area.
In general, it is advisable to massage the painful area yourself. In this case one speaks of a so-called "trigger point massage". Fascia rolls can also be used. When used correctly, they release tension and allow muscles to relax. They also have a beneficial effect on the regeneration of the muscles.
Regular massage of the tibia and fibula muscles is more important in preventing tibial splint syndrome than in treating it.
Muscular-related complaints can be treated more effectively with stretching exercises.
Can you operate on a tibial splint syndrome?
A tibial splint can in principle be treated surgically if conservative treatment approaches are no longer successful.
However, there is still no well-founded surgical method for such a chronic shin splint syndrome.
If a compartment syndrome is the cause of the tibial splint syndrome, the cause of the symptoms of the tibial splint syndrome can also be treated during the surgical treatment of the compartment syndrome. A compartment syndrome is an increase in the volume of the tibia and fibula muscles with a resulting increase in pressure in the individual muscle boxes.
This can lead to irritation of the periosteum and severe pain. Compartment syndrome can take on serious proportions as soon as the increased pressure threatens to prevent blood flow. In such a case, a relieving operation with splitting of the muscle fascia must be performed. Accordingly, a tibial splint can be operated on in this special case.
Can chronic shin splints be curable?
The word chronic implies that the symptoms are no longer temporary but permanent.
Healing in the chronic stage is therefore much more time-consuming and difficult. Therefore, those affected must recognize the first signs of a tibial splint syndrome in good time and take the right therapeutic measures promptly to counteract chronification.
In general, however, this syndrome is a chronic and therefore recurring clinical picture. There is no complete cure, but acute complaints can be relieved effectively and in the long term, so that those affected are symptom-free for the moment. A recurrence is possible at any time.
Long-distance runners are particularly prone to this condition. A strong and sustained strain on the tibia and fibula muscles on a hard surface provokes a recurring shin splints. Whether a chronic tibial splint syndrome can be cured depends largely on the discipline of those affected to adhere to preventive measures and to avoid chronic overloading of the tibia and fibula muscles.
Effective prevention
In order to prevent shin splints, on the one hand the level of training should be adapted to the level of training. This is to prevent athletes from overstressing themselves, which could lead to tibial splint syndrome.
On the other hand, any improper stress while running should be compensated for. The shoes used should be adapted to the flooring and running spikes should be avoided. A corresponding warm-up program should be carried out before every training session.
In general, different approaches exist to effectively prevent the development of tibial splint syndrome. It is important to avoid the personal causes for the potential development of the disease. A disproportionately fast growth of the muscles that lie above, next to or behind the shinbone can trigger a shinbone syndrome. For this reason, it is important to adapt the individual training workload to the current training status. By slowly building up the muscles, the syndrome can be prevented even with forced training.
A risk factor for the development of the disease occurs particularly in running. Incorrect rolling behavior of the foot can lead to the development of a shin splints. People who perform what is known as pronation when rolling are particularly at risk. A treadmill analysis should be carried out if necessary, in order to be able to analyze the running behavior, especially if complaints of the shinbone occur frequently. If there is actually a critical running movement, you can try to correct it with various aids. The use of insoles in particular can help to change the way you unwind. The use of a tape, which is stuck to the skin of the lower leg, helps in individual cases to correct the running behavior.
Athletes should make sure that the shoes they use have sufficient cushioning. This can lose its function after extensive use, which is why running shoes should be replaced after a while to prevent shin splints. The technique with which certain sports are performed is also important in preventing the syndrome. In addition to the correct rolling behavior during running, other athletes who run a lot should also pay attention to the running movement and have it examined if necessary.
In general, it is important to take a break from exercising as soon as the first signs of shin splint syndrome appear in order to protect the damaged structures and achieve healing. When sports can be restarted individually without expecting the symptoms to worsen, depends on the therapy carried out. In individual cases, the attending physician can give recommendations as to which sport is suitable as a compensation and when the originally performed sport can be resumed.
Prevent with stretching exercises
Stretching as a prophylactic measure before and after exercise is essential to prevent shin splints from developing in the first place.
As a preventive measure, stretching should be taken to heart by long-distance runners in particular, as they are considered to be predisposed athletes for tibial splint syndrome. However, if those affected already suffer from shin splints, stretching can also be used as a therapeutic measure.
In the case of manifest shin splints, those affected should have spared their shins for a sufficient period of time before starting the stretching exercises. Only then are stretching exercises helpful.
The focus of the stretching exercises are the muscles around the tibia and fibula, as they are considered to be the trigger for pain. In general, the aim of stretching exercises is on the one hand to warm up the muscles before an exercise and to stretch them before. On the other hand, existing muscular tensions must be released. It is important that those affected choose the right stretching exercises and do them correctly. An instruction from an experienced physiotherapist can therefore be useful.
Summary
The so-called Shin splints there is a disproportion between muscle volume, mostly in the lower extremities, and the available space. The muscles of the lower extremities run in muscle boxes and are covered by a thin but stable muscle shell (Fascia) surround.
If the Muscles there is a lack of space for the muscle in the fascia. The resulting pressure means that the blood in the muscle can no longer circulate properly. This can lead to insufficient supply and necrosis of the muscle. The increased pressure also leads to stress on the supplying nerves, which triggers the initial symptoms - a pulling, burning pressure pain.
A tibial splint syndrome can be suspected diagnostically if the patients report the said pain after a distance of approx. 500 m and this persists despite the rest afterwards.
Furthermore, there is usually an elastically taut skin over the corresponding lodge area. For further diagnosis, imaging methods can be used, which can primarily diagnose other diseases that cause pain. Mention should be made here of the X-ray (to rule out fractures), the MRI (to rule out muscular causes).
Also a Ultrasonic can be done to see inflammatory fluid in and around the muscle. Swelling of the muscle can also sometimes be seen with the ultrasound. A tibial splint syndrome can be treated conservatively on the one hand Immobilization, cooling and application of medicinal or physical anti-inflammatory measures, on the other hand, an open or minimally invasive surgery may become necessary, in which a transection of the affected muscle fascia is performed so that the pressure in it sings and the muscle can stretch again. After surgery, 60-100% of patients remain symptom-free.