Diabetic foot
Definition- what is a diabetic foot?
A diabetic foot is the term used to describe very specific symptoms and symptoms that occur as part of a diabetes disease. These are the consequences of excessively high blood sugar levels, which cause damage to blood vessels and nerves. Diabetic foot syndrome is characterized by poorly healing injuries to the foot, from which chronic wounds can easily develop. Regular check-ups by the doctor are necessary to prevent this. In addition to wound care on the foot, blood sugar control is the most important component of therapy.
Also read the article on the topic: Consequences of diabetes

causes
The combination of the complications of a diabetes disease should be mentioned as the cause of the diabetic foot. Especially with poorly adjusted blood sugar levels and other risk factors for poor wound healing such as smoking or being overweight, diabetic foot syndrome can occur. After 5-10 years with excessively high blood sugar levels, there is significant damage to the blood vessels on the legs, so that the feet are no longer well supplied with blood.
In addition, the sugar in the blood damages the nerves, so that the sensation in the foot decreases. This means that the patient is no longer aware of the injuries and in some cases does not even notice that there is a wound on the foot. This can also occur with peripheral arterial disease, a condition in which limescale deposits block the arteries in the legs and prevent blood flow to the feet. If this arterial disease and diabetes with foot syndrome occur together, the outlook for the disease progression on the foot is very poor.
Also provide information on the topic: peripheral arterial disease
Risk factors
There are certain risk factors that can promote the development of a diabetic foot and make it worse. Basically the problem consists of the loss of sensitivity in the foot due to damage to the nerves and a reduced blood flow. All factors that reduce blood circulation, such as smoking, obesity, a lipid metabolism disorder or lack of exercise, thus increase the incidence of diabetic feet.
Poor foot hygiene and care can also lead to wounds. Badly fitting shoes also promote pressure points and reduced blood circulation in the foot.
diagnosis
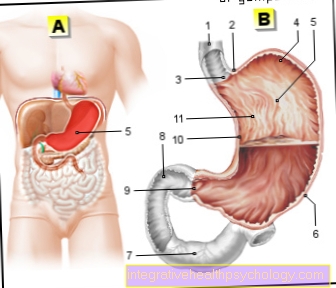
The basis for the development of a diabetic foot is a patient's disease of diabetes mellitus, usually type 2. In order to make the diagnosis, the diabetes itself must be confirmed by laboratory tests and the long-term blood sugar level, the HbA1c, checked at regular intervals become. A detailed examination of the feet must be carried out with consideration of the skin, temperature and gross malpositions of the feet, abnormal gait and looking for the foot pulses. A characteristic of the diabetic foot with damage to the nerves is a reduced sensitivity, vibration, temperature and pain.
Further information on the subject can be found at: Type 2 diabetes mellitus
Tuning fork test
The tuning fork test is a routine examination as part of the regular check-up for diabetic foot syndrome. But it is also used for other clinical pictures that are associated with a reduced feeling in the foot.With the tuning fork test you want to find out whether and how strong the vibration sensation and the deep sensitivity are still present.
The patient lies or sits on the examination couch and the examiner strikes the tuning fork. Then it is placed either on the inner ankle or the metatarsophalangeal joint of the big toe. The patient indicates when he can no longer feel anything and at precisely that point in time the intensity of the vibration is read off on a scale.
What are the symptoms of a diabetic foot?
People suffering from diabetes mellitus should definitely take part in preventive examinations at regular, small intervals. It is also important for a patient to know what symptoms to look out for. In the context of diabetic foot syndrome, for example, there may be a disruption of pain perception or temperature perception. Affected patients then actually feel less pain and cold or warmth on their feet. In contrast, patients can also experience increased pain sensitivity with nocturnal pain attacks.
Damage to the nerves in the foot can also be manifested by tingling sensations, or the feeling that patients describe as if ants were walking over your feet or as if you were being stung by a thousand needles. Some symptoms of diabetic foot can also be seen on the skin. This often leads to extremely dry skin on the foot. Pressure points with an unusual reddening are also noticeable and the feet sometimes swell.
Ulcer / ulcer
A dreaded complication of diabetic foot syndrome is the so-called neuropathic ulcer, also called the malum perforans. A neuropathic ulcer is an ulcer that occurs when the nerves are damaged. Reduced pain perception and sensitivity can easily turn small injuries into complex wounds. This can also lead to phlegmon, i.e. a deep, purulent inflammation of the foot tissue. To make matters worse, the blood circulation in the foot is often reduced, so it is better not to have surgical scraping performed.
Read more on the topic: Ulcer
Stages
The course of the disease of the diabetic foot can be divided into different phases. These phases, which are also called the Wagner-Armstrong stages, are a possible form of classification. These describe the severity of a wound and also consider whether there is an inflammation or a circulatory disorder.
The description of the wound ranges from 0-5, with 0 representing no injury and 5 representing the worst condition, spread over the entire foot. A letter is added to each number in this classification if in case A only the wound is present. Or in case B there is also an infection. C is used if a circulatory disorder in the foot is detected. And if there is an infection and a circulatory disorder, this is explained with the letter D. Thanks to this uniform staging, the process can be adequately described and documented even when the shift changes or the nursing staff changes. The correct therapy and the further course of wound treatment can then be adjusted according to the respective stage.
therapy
The treatment of the diabetic foot is directly related to the therapy of the diabetes disease itself. A decline in the findings on the foot can only be expected if the blood sugar control is also successful. For this purpose, the blood sugar value must be measured regularly, depending on the diabetes therapy concept. The long-term blood sugar value, the HbA1c, is also an important control value for an optimal setting. The next important step is the regular control of the feet in the mirror by the patient and then also by the treating doctor.
The earlier the injury or wound was recognized, the easier it is to take action against it. Preventive measures such as medical foot care, orthopedic shoe insoles, daily foot care and special attention to possible injuries are also very advisable. In the case of a wound, it must then be treated by a doctor or a wound nurse at short intervals. Therapy with antibiotics or the removal of inflamed and damaged tissue may also be necessary. If the blood supply to the foot is poor, surgical intervention with tissue removal is not recommended, as the injury can then become even bigger.
For more information, see:
- Therapy of diabetes
- Toe amputation
When is an amputation necessary?
If an inflamed wound or ulcer on the foot can no longer be treated and the condition of the diabetic foot cannot be brought under control, an amputation may be necessary in the worst case. If there is only diabetic damage to the nerves, the probability is higher that only individual bones and pieces of tissue have to be removed, but not part of the leg has to be amputated. However, if there is also a reduced blood flow to the leg, this means that wounds can heal very poorly and bacteria are more difficult to fight.
This article might also interest you: Causes of an amputation
Course of disease
The course of the disease of the diabetic foot is different for each patient. Usually an initially insignificant small injury to the foot or a skin defect with pressure points leads to a rapidly progressing inflammation of the wound. It is therefore important that the patient checks his or her foot for wounds in the mirror every day and that he regularly goes to the doctor for check-ups.
Once a wound has developed, the patient often has to take care of it for months and have good wound care carried out. Unfortunately, this can drag on for years and even become chronic.
forecast
The prognosis of the diabetic foot can be significantly improved with the cooperation of the patient. If the blood sugar levels remain poor and the nerves are damaged, the course of the disease can worsen significantly. Additional illnesses and poor general conditions, such as shoes that are too tight, also play a role in the overall picture of the illness. In most patients, the ulcers heal after a few months. In every 10th patient, however, the wounds on the foot can no longer be brought under control.