multiple sclerosis
definition
MS, disseminated encephalomyelitis, disseminated sclerosis, multiplex sclerosis, polysclerosis
English: multiple sclerosis
introduction
Multiple sclerosis falls under the diseases of Immune system, more precisely it is an inflammatory one Autoimmune disease. It is a reaction to the body's own nervous tissue, which is usually mediated by a certain type of inflammatory cells in the blood, the T lymphocytes.
Multiple sclerosis is a disease that causes the Nervous system affects people. The annoy of the human body lose their insulating layer. This significantly reduces the routing speed with which information is transported.

Epidemiology
In Germany about 1 in 400 inhabitants are affected. It is assumed that there are more than 200,000 sick people in Germany today. The disease is most common in people between the ages of 20 and 40. The ratio women: men is 2: 1.
MS (Multiple Sclerosis) is a disease of the Caucasian population. In Europe there are comparatively many sick people, whereas you can hardly find anyone with this disease near the equator.
It is astonishing, however, that from the age of 15 you take the probability of developing MS (multiple sclerosis) with you if you want to live in the tropics.
Before the age of 15, one adapts to the probability of the disease in the respective region. If you emigrate to a tropical country before your 15th birthday, the likelihood of developing MS (multiple sclerosis) is negligible.
Signs of MS
The first symptoms to appear will vary from patient to patient. The most common sensation disorders are the arms or legs (see also: Arm falls asleep). These come on suddenly and are usually the only limitation for the patient.
Visual disturbances, caused by inflammation of the optic nerve, are often the first symptom. Here, a loss of vision can be perceived in the center of the field of vision, a clouded view or the seeing of double images.
Read more on the topic: Optic nerve inflammation in MS
Another early symptom can be the appearance of disorders of muscle function. Paralysis, weakness and coordination disorders can be counted here. In addition, general tiredness and concentration problems can occur at the beginning of the illness.
Which of these symptoms occurs at the beginning depends on the first affected area in the central nervous system. If multiple sclerosis begins, for example, with inflammation or the breakdown of the insulating myelin sheaths that surround the optic nerve, the first thing the patient will notice is visual disturbances. If other parts of the brain are affected, the disease manifests itself through other symptoms.
The age of the patients in whom the early symptoms appear is between 15 and 40 years. In this stage of the disease, symptoms usually appear in phases. At the beginning, the deficits usually recede completely, whereas in the further course of multiple sclerosis, permanent neurological damage must be expected.
However, all of these first signs are not necessarily associated with the onset of multiple sclerosis. There are many other medical conditions that can lead to these symptoms. These other diseases must first be eliminated before a diagnosis of MS can be made.
Read more on the subject at: Differential diagnoses of multiple sclerosis
The so-called Expanded Disbility Status Scale (EDSS) is used to evaluate these signs that indicate the disease. Here, the patient's limitations are evaluated in various areas and the severity of the current impairments can be determined.
Symptoms
Basically, MS (multiple sclerosis) can cause all imaginable neurological or psychiatric complaints. It all depends on which areas of the central nervous system are affected.
The most common weakness is around 40%. It is also one of the first symptoms of MS.
Sensitivity disorders are also frequently observed. There can be increased or decreased sensitivity. If the sense of position is affected, gait disorders, known as ataxia, occur.
The extinguished abdominal skin reflex is probably the most important parameter in sensitivity disorders. In this case, the patient no longer feels the brushing of the abdominal wall with a somewhat pointed object. In a healthy person, this wiping over the nerve connection to the brain would cause the abdominal muscles to contract.
The optic nerve can also be affected by the demyelinating of the nerves. The visual disturbances caused by this can occur on one or both sides and range from blurred vision to blindness.
Read more on the topic: Optic nerve inflammation in multiple sclerosis and Eye pain
The motor tracts in the spinal cord are also mostly affected. The symptoms range from flaccid paralysis, spastic paralysis and increased reflexes to impaired fine motor skills.
Also read: Numbness in the arm
If the cerebellum is affected, there is an unsteady gait known as ataxia. An intention tremor is also not uncommon. This is where the patient's hands tremble as soon as they turn their attention to a certain object that they want to grab. Affected people have considerable difficulty drinking from a cup without spilling most of the contents. This trembling does not exist in rest!
Bladder dysfunction and rectal dysfunction are arguably the most uncomfortable complaints. The bladder and rectum are no longer subject to the voluntary control of the patient and empty themselves.
Read more about Bladder and rectum disorder
Dementia, inadequate euphoria (e.g. laughing at a funeral), depression and emotional lability are among the mental disorders (see also mental disorder).
Caution is advised in the event of physical or psychological stress, as this can worsen the symptoms. High temperatures are also said to worsen the symptoms.
You might also be interested in: Thumb twitching- possible symptom of MS?
Tendonitis and phlebitis in MS
The main symptoms of multiple sclerosis are paresthesia, tingling or numbness, mood swings and impaired mobility, due to the thinning of the nerve tracts. Inflammation of the tendons of various muscles or inflammation of venous valves in the area of the leg blood vessels can also always occur. However, these two symptoms tend to be rarer and are much less common in combination. The main reason why multiple sclerosis can lead to inflammation of the blood vessels and / or tendons is primarily the unregulated movement of the arms and legs caused by MS. In the early stages there is practically no inflammation of the tendons and veins (corresponds to the statistical normal occurrence in the population). With increasing immobility, however, there is also an increasing number of incorrect loads with the resulting overuse of muscles and tendons. Frequent resting of the legs and the reduced exercise capacity can also lead to inflammation of the leg veins.
causes
The cause of multiple sclerosis / encephalitis disseminata is controversial because it has not yet been adequately researched. There are several options up for debate:
- It is about a Autoimmune disease. The body fights its own nerve envelope proteins.
- A genetic component may also play a role. Indicative is the fact that in about 10 percent of cases a familial accumulation consists.
- Also one Viral infectionwhich slowly leads to the development of MS is being considered. The viruses could be measles -, Rabies - (rabies) or Paramyxo viruses act.
The pathological (pathological) mechanisms that characterize the disease, on the other hand, are well described:
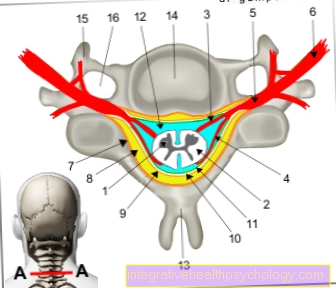
Around the nerve cords, which in turn consist of many thin nerve fibers, there is usually a protein sheath. This serves to protect the annoy, but it also increases the routing speed. Thanks to this shell of proteins (myelin), the so-called myelin sheath (myelin sheath), signals can be passed on very quickly. This transport of information happens in two directions. On the one hand, commands are sent from the brain to the muscles, for example, in order to carry out a voluntary movement. On the other hand, feelings (pointed, dull) or temperature (cold, warm) can also go in the other direction brain be directed to be consciously perceived here.
In the clinical picture of multiple sclerosis, the cause of the disease is demolished so far: the protein shell around the nerves slowly dissolves - the white matter in the brain perishes.
This demarking occurs in spots. The myelin-forming cells are replaced by nerve fibers. These areas are considered to be scarred (sclerosed).
Are the Protein shells Once the nerves degenerate, the nerve conduction velocity decreases sharply. Due to the very long nerve tracts (e.g. for foot) also mean a complete loss of functionality.
These are particularly often affected
- Cerebellum
- Brain stem
- Optic nerve and
- the spinal cord.
in the Spinal cord nerve tracts are particularly affected, which play an important role in voluntary muscle movement.
diagnosis

To the Diagnosis of MS (Multiple Sclerosis) Anamnesis, physical examinations, possibly a Lumbar puncture and an MRI is necessary. During the neurological examination, in some cases a extinguished abdominal skin reflex can be determined.
It used to belong to Computed Tomography Of the head (cCT) to routine examinations if multiple sclerosis is suspected.
MRI for multiple sclerosis
The MRI of the brain is the first choice examination method for one multiple sclerosis to diagnose.
The inflammatory foci are more visible here than in CT (computed tomography). The MRI (Magnetic resonance imaging) can be run in different sequences. In the resulting images of one of them, old lesions, i.e. scars, are easier to see.
These are typically next to the Cavities (ventricles) of the brain, which with Nerve fluid (liquor) are filled.
Other typical locations at multiple sclerosis are near the cerebral cortex or in the connecting structure between the two halves of the brain (the so-called bar).
This is the most valuable imaging diagnosis for multiple sclerosis MRI of the head With an MRI of the brain, inflammatory foci in the brain or spinal cord can be reliably detected. By administering contrast media, the radiologist can distinguish fresh foci (e.g. in acute episodes) from old foci (e.g. due to scar) in the nerve tissue in the MRI. Thanks to the improvements in MRI techniques, diagnostics have also become much better, especially in follow-up checks.
With the other recording technique of the MRI (magnetic resonance imaging) of the head, additional Administration of contrast medium especially the new lesions shown. They absorb the contrast agent that is injected into the patient through the vein and represent inflammatory processes.
Further diagnostic options
In order to test the functionality of the brain and its individual parts, functional tests can be carried out on various sensory systems. Here you can test whether visual or hearing impressions are still reaching the brain and how it reacts to them.
Sensitivity (feeling of touch and / or pain) and motor skills (movement of limbs through magnetic stimulation of brain regions) are also checked in this way. As expected, the potentials obtained appear with a delay.
When collecting nerve water (med .: liquor) in the context of so-called liquor diagnostics, the following findings are characteristic: clear liquid, many white blood cells, a lot of protein and an increased number of cells. If there is MS, one expects an independent production of antibodies in the nerve water. These can then also be verified.
You can find out more about the withdrawal of brain water under our topic: CSF diagnostics.
The diagnosis of MS is clear if:
- at least 2 demyelinating foci can be detected in CCT (computed tomography of the skull) / MRT (magnetic resonance tomography) and
- there is a characteristic CSF finding from CSF diagnostics AND
- at least 2 relapses or progressive symptoms for at least a year
Multiple sclerosis is still likely if only two of the three criteria mentioned are present. After only one The thrust experienced up to now is shifting from “definitely” to “likely”.
Therapy for multiple sclerosis
In most cases, therapy for multiple sclerosis should be medication.
However, multiple sclerosis therapy is not designed to cure the disease, but rather to minimize the patient's symptoms.Especially during an acute flare-up, multiple sclerosis therapy consists of minimizing the flare-up and thus keeping the effects as low as possible.
Treatment with corticosteroids is an option during an acute episode. These are drugs that suppress the immune system and inflammation, thus minimizing symptoms.
Furthermore, plasmapheresis can also be performed as a therapy for multiple sclerosis in an acute episode. The liquid components of the blood (plasma) and replaced with plasma from a donor.
In addition to acute therapy for multiple sclerosis, the disease should also be treated permanently and preventively in order to minimize relapses and reduce the severity.
An interferon-beta preparation is often used as a therapy for multiple sclerosis, which ensures that the immune system does not react excessively to the disease.
Also Glatiramer acetate, Dimethyl fumarate (Tecfidera®) and Teriflunomide are now used as a so-called basic therapy for multiple sclerosis, especially when therapy with interferon-beta is not an option.
Especially those Fumaric acid According to recent studies, (Tecfidera®) has proven to be particularly good at reducing thrust
In general, however, a patient may not respond well to any of the above drugs. In this case, the doctor can suggest what is known as second-line therapy for multiple sclerosis. Medicines are used here, which also serve as basic therapy.
These include the drugs:
- Natalizumab
- Fingolimod
- Alemtuzumab
- Mitoxantrone
and - Cyclophosphamide.
In addition to the actual therapy for multiple sclerosis, it is also always important to treat the accompanying symptoms. Some patients experience severe pain during an episode, while the illness makes other patients depressed. It is important to respond to the individual needs of each patient and to adapt the therapy for multiple sclerosis to the patient. This can mean that in addition to drug therapy, pain therapy, physiotherapy or psychotherapy may be required.
Read more on the topic: Therapy for multiple sclerosis
The use of muscle relaxants can also reduce the symptoms. Read more about this under: Muscle relaxants
Multiple Sclerosis Diet
Whether diet can have a positive effect on multiple sclerosis is a very controversial topic in medical circles.
Nevertheless, the diet can help in multiple sclerosis to have a positive influence on the course of the disease.
Since multiple sclerosis is an inflammatory disease of the nervous system, a balanced diet can be helpful around the so-called oxidative stressthat is caused by the inflammation, and thus improve the symptoms of multiple sclerosis through diet.
What is especially important, however, is the fact that multiple sclerosis leads to a variety of symptoms, which can be very positively influenced by a balanced diet.
Thus, nutrition may not help directly in multiple sclerosis, but it can be an important support to alleviate the accompanying symptoms and enable the patient to live as symptom-free as possible. For example, many patients suffer from severe fatigue.
By a balanced, low-calorie diet With lots of fruit, vegetables and fiber, tiredness can be reduced as the body does not have to constantly deal with the absorption of fatty substances. In general, it is important to be very careful when consuming fats. The diet can actually make multiple sclerosis worse or better. Inflammation products arise from a substance that is absorbed from fats in food, namely the so-called Arachidonic acid.
Egg yolks, meat, offal, fish, butter and skin contain a lot of arachidonic acid and can thus promote the inflammation that occurs in multiple sclerosis. On the other hand, if a patient avoids these substances, inflammation can also be minimized. Thus, nutrition is definitely important in multiple sclerosis, even if it is only of minor importance.
Furthermore, patients can ensure that they consume sufficient omega-3 fatty acids, which are contained in fish or fish oil capsules, for example. These have an inhibiting effect on the inflammation and thus favor a mild course of the disease. Overall, various diets, especially for multiple sclerosis, have been designed, for example the Diet according to Dr. Grim reaper. These are based on the fact that patients with multiple sclerosis should closely monitor their diet and should avoid the above-mentioned fat suppliers if possible. However, a balanced diet with healthy fats is usually sufficient and no special diet is required to reduce the symptoms of multiple sclerosis.
forecast
The forecast depends on the course form. Cheap is a rapid onset and an age below 35 years, as well as sensory and visual disturbances, which however completely regress again.
Unfavorable For the prognosis, an age over 40 years, paralysis and unsteady gait are the first complaints.
After the onset of the disease, life expectancy with unfavorable forms is usually only 25 to 30 years, but even favorable forms can remain unchanged.
Gradient forms
The course of the Multiple sclerosis can be different:
- Thrust-shaped
In 70% of the cases the course is chronic, but regresses between the attacks, so that free intervals of different lengths (1 month, 1 - 2 years, 15 years) arise. - Relapsing progressive
These are relapses without complete regression. The new thrust arises at the bottom of the interval in which the disease is less pronounced. So the relapses get worse every time. - Chronically progressive
The symptoms increase more and more without receding.
Course of multiple sclerosis
Multiple sclerosis is a chronic, incurable disease.
This means that the course of multiple sclerosis can be influenced by medication and suitable therapy, but the patient has to live with the disease for a lifetime.
Overall, the course of multiple sclerosis can be relapsing, which means that there are long times in which the patient does not even notice that he has the disease. On the other hand there is the chronically progressive (progressive) Progressive form.
The disease usually begins with recurring attacks and then at some point turns into a chronic disease. If there is another acute attack, the patient has the various typical symptoms of multiple sclerosis.
The course of multiple sclerosis is very different for each patient.
The disease usually begins at a very young age, and patients are often around 20-30 years old. The initial course of multiple sclerosis is usually relapsing, with an attack lasting from a few days to several weeks. The repeated occurrence of the attacks is also very individual.
There are usually months between the individual attacks, whereby the course of the multiple sclerosis attacks can be positively influenced by adequate therapy. This can then mean that a patient is symptom-free for years, until another episode occurs.
This course of multiple sclerosis is the classic course and occurs in about 80% of all patients in stages. However, in 20% of all patients there is a chronically progressive (progressive) Course. In this course of multiple sclerosis, there are no recurring attacks but the patient suffers the entire time from the symptoms of multiple sclerosis, which then get worse and worse.
In general, the course of multiple sclerosis can be well influenced by drugs, but it cannot be stopped. Thus, after years of illness, physical impairments and disabilities often arise later. Overall, it is assumed that patients without treatment do not have severe disabilities after 15 years, since the course of multiple sclerosis is positively influenced in patients with adequate therapy, the negative effects of the disease can be delayed very far.
Read more about this: Course of multiple sclerosis
prophylaxis
It is impossible to prevent multiple sclerosis (MS) from developing because the cause has not yet been clearly identified. However, you can prevent situations that can trigger flare-ups.
Triggers can be:
- stress
- mental or physical stress
- or high temperatures.