Eczema between the toes
Definition
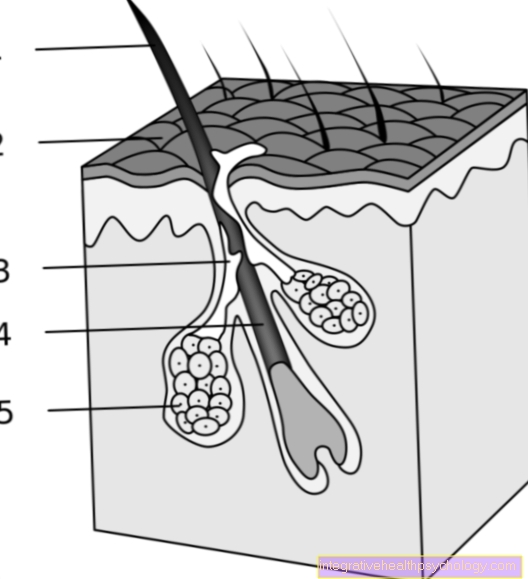
Eczema is basically an inflammatory, but initially non-contagious skin reaction that occurs again and again, triggered by certain noxae (toxins). The eczema goes through different stages, which can be divided into acute, subacute and chronic. An attacked and not intact skin surface or a reduced immune system make people particularly susceptible to eczema between the toes and, in the worst case, can serve as an entry point for bacterial pathogens. How eczema manifests itself in individual cases and what can be done about it is explained below.
Read a lot of interesting information in our main article: Eczema

Symptoms of eczema between the toes
Eczema between the toes can be limited to the spaces between the toes as well as spreading to other skin areas on the foot. In the acute phase, small vesicles, nodules, reddening and swelling appear on the skin, which in some cases can be noticed by itching or slight pain due to the inflammatory reaction.
In the subacute phase, crusts or small skin injuries arise on the bottom of the burst or receding skin vesicles, which are caused by the loss of the top layer of skin.
This can be followed by a chronic phase of eczema. The focus here is primarily on flaking and thickening of the skin with the formation of a corneal layer, usually accompanied by reddening of the skin. Despite the relatively uniform phases of eczema between the toes, depending on the cause, this can also have various accompanying symptoms, such as itching, pain, oozing, bacterial infection, etc. In addition, this eczema can only occur once as a result of a contact reaction or it can always heal and flare up again.
In the case of a bacterial superinfection of the eczema, this can manifest itself as yellow crusts, overheating and pain. In worse cases, the skin barrier is so damaged by the eczema that germs can spread to the entire lower leg and form an erysipelago
causes
In most cases, eczema between the toes always proceeds in the same way, but the causes can vary in nature.
- Pollutants
Pollutants can act on the skin from outside, which irritate the skin between the toes and dry it out, for example alkaline substances, excessive heat or cold or sweat. Eczema can easily develop without appropriate measures such as moisturizing or sweat-reducing measures. In addition, certain substances, such as nickel, can cause an allergic skin reaction, which then presents itself as eczema and, compared to the substances mentioned above, is not strictly limited to the site of action.
- Athlete's foot
- Atopic dermatitis
People with atopic dermatitis are more likely to develop eczema.
Read more on the topic: Eczema on the foot
Therapy for eczema between the toes
In the acute phase of eczema, i.e. when the blisters and nodules on the skin and the reddening are in the foreground, it is recommended to use moist compresses, for example with antiseptics or black tea, or a shaking mixture. Both application methods aim to dry out the blisters and soothe the skin.
In the subacute phase, a mixed emulsion can be used, which is supposed to supply the sensitive skin between the toes with moisture and a protective layer of fat. Normally this is applied twice a day and if necessary, if the skin appears very dry and cracked. Because at the end of the treatment, the eczema between the toes should have completely receded and the skin should be intact again so that there is no infection with germs.
In the case of chronic eczema, it is an advantage to choose an ointment with a high fat content so that the existing horny layer can be better penetrated. Depending on the severity of the eczema, a glucocorticoid such as cortisone can be applied to the skin using the mixed emulsion or ointment. The dosage of the cortisone should best be done by a dermatologist, who will adapt it to the eczema and explain exactly how to handle cortisone and the duration of use. As an alternative to glucocorticoids, local immunosuppressants can now also be used, which, however, also require special handling due to their side effects. When treating eczema, accompanying symptoms such as pain or the like can of course also be treated so that a noticeable improvement occurs as quickly as possible.
diagnosis
In order to be able to make the diagnosis of eczema, you need some information from the person affected, which explains the occurrence of this eczema between the toes and you have to get an idea of the skin appearance in order to be able to classify it further. So stand at the beginning Medical history and inspection on the plan. For example, you can ask whether certain substances have acted on this area that could have caused allergic or toxic contact eczema. Whether new detergent or care products have been used or whether you wear shoes for a long time that are barely breathable can help.
In people with atopic dermatitis, which classically have eczema in the flexor joints, the clinical picture can explain the tendency to develop eczema between the toes. Since athlete's foot can also cause eczema, a frequent infestation should be clarified. In addition, you should make sure that no further eczema or any other skin condition develops on other areas of the skin, which should also be taken into account. Therefore, one should not only look at the feet and the spaces between the toes, but ideally the entire skin. Normally, the anamnesis and close examination of the skin is sufficient for the diagnosis. However, if there is a suspicion that a athlete's foot or an allergen is behind the eczema, further measures can be taken, such as a so-called Patch test if an allergy is suspected or the Examination of a small sample of skin on a mushroom.
forecast
After successfully treating eczema between the toes, the prognosis depends in some ways on the cause. But if you avoid the eczema-causing substances and cares for the skin between the toes, the prognosis is good. The eczema heals usually without a scar out.
prophylaxis
To prevent eczema between the toes, care should be taken to keep the skin in place always intact is and is there no moisture, like sweat, accumulates so that the skin barrier retains its function and no pathogens such as fungi or bacteria can penetrate. For dry, cracked skin becomes a application of moisturizing creams recommended. Is the foot rather wet, it would be well appropriate breathable footwear to choose and to rid the feet of it regularly.
Dyshidroic eczema
Dyshidroic eczema is a skin change that can occur primarily on the hands and feet. It used to be assumed that the cause of this eczema was a disorder of the sweat glands, hence the name came about (hidrosis refers to the formation of sweat, so dyshidrosis is a disturbed sweat formation). Nowadays, however, we know that eczema is triggered by allergic, toxic or atopic (e.g. in the context of neurodermatitis) causes and that increased sweat production is more of a symptom.
Dyshidroic eczema is characterized by reddened skin on which numerous plump blisters can be found that are filled with clear to slightly yellowish liquid. The skin is sensitive and usually itchy. It can also lead to an additional infection with bacteria and fungi, which worsen the clinical picture. The diagnosis of dyshidroic eczema is primarily made through a clinical examination, and tests for allergies and atopy can also be carried out.
Therapeutically, cortisone-containing ointments and local UV-A rays can be used to remedy mild forms; systemic steroids in the form of tablets may be necessary for severe forms
Eczema or skin fungus
Distinguishing between skin fungus and eczema is usually not easy, but there are some features that can help differentiate. Both diseases have in common that the affected skin between the toes is often very sensitive and it hurts and itches when touched lightly. Small skin tears are also possible with both diseases. The eczema usually shows itself with a reddening of the skin; when infected with skin fungi, a rather gray-white scaling is often seen.
The skin often looks a little puffy here. With eczema, depending on the cause, there may be small, plump blisters. These contain, for example, clear liquid. This is rather atypical for skin fungus between the toes and is more likely to be visible in the case of an additional infection with bacteria. In the case of eczema in the context of allergies or neurodermatitis, other areas (e.g. the flexors of the arms and legs) are often affected. This is usually not the case with athlete's foot, as well as the spaces between the toes, usually only other parts of the foot are affected. Often there are white, scaly cracks on the cornea of the heel. The top of the foot is usually left out. In order to clearly differentiate between athlete's foot and eczema, however, you should see your family doctor or dermatologist. This can better assess this with his experience and at the same time prescribe the necessary therapy!




.jpg)















-mit-ten-(titanic-elastic-nail)-oder-sten.jpg)