Inflammation of the testicles
introduction
An inflammation of the testicle, also called orchitis, is caused in the majority of cases by bacteria or viruses. Testicular inflammation is almost always accompanied by inflammation of the epididymis (epididymitis). The clinical picture is then called the clinical picture of an epidymorchitis. Inflammation of the testicle usually occurs on one side, pain can vary in severity. However, swelling and general symptoms of a viral or bacterial infection are mandatory.
You may also be interested in this topic: What are the causes of testicular inflammation?
Causes of Inflamed Testicles
Viral causes
Inflammation of the testicle is usually caused by viruses, such as the paramyxoviruses, which also cause mumps. Most often, testicular inflammation occurs as part of the mumps disease, typically 4-7 days after the parotid gland becomes inflamed. But varicella viruses, Coxsackie viruses, and echo viruses can also cause orchitis. They reach the testicles uniformly via the bloodstream and spread there.
We are well aware of varicella, they come from the herpesvirus family and cause chickenpox - usually in childhood. Pfeiffer's glandular fever and the Ebstein Barr Virus (EBV, or infectious mononucleosis) can also cause inflammation of the testicle. The infections mentioned are viral infections that are caused by viruses.
Bacterial causes
Of course, orchitis can also have bacterial causes: the bacteria usually spread upwards via the urinary and seminal passages and thus reach the testicles. Due to the anatomical proximity, the epididymis is almost always affected. The spectrum of pathogens in orchitis is similar to that of a normal urinary tract infection. It ranges from chlamydia, neisseria, klebsiae, pseudomonads to staphylococci, streptococci, E. coli bacteria and brucellae. Some well-known diseases that can also be caused by these pathogens are gonorrhoeae and syphilis. In principle, sexually active men are more often affected by inflammation of the testicles, since the triggering factor can often be sexually transmitted diseases such as those mentioned above.
External injuries
However, orchitis does not always have to be primarily caused by viruses or bacteria; external injuries - i.e. trauma - can also open a gateway for pathogens that then colonize the wound. Epididymitis can also spread to the testicles, as both are very close to each other and have a large contact area.
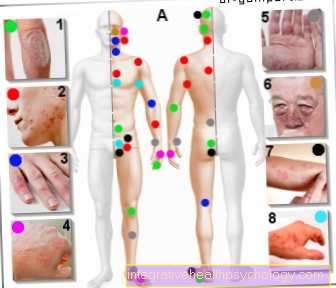
Symptoms
Typical symptoms are pain and swelling of the scrotum and testicle.
Usually the symptoms only occur on one side, and the second testicle may also be affected as the disease progresses. Orchitis usually occurs as a result of an underlying disease, such as glandular fever, so that its symptoms predominate for the time being.
After 1-2 days, however, there is pain, which can vary from an uncomfortable pulling in the testicle to a very strong sensation of pain. The pain usually goes away within a week. Beyond that, however, the symptoms of the underlying disease usually remain.
These include fever, chills, fatigue, muscle aches, headaches, and nausea.
The swelling can be very prominent and is typical of inflammation.In addition to swelling, redness, pain, impaired function, and warmth are general signs of inflammation.
The testicle is very sensitive to touch during this phase.
Read more about this under:
- Swollen testicles - what's behind it?
- I recognize epididymitis by these symptoms
- Scrotum
treatment
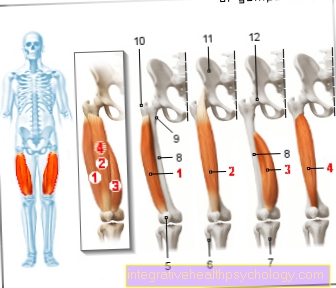
Treatment is first symptomatic by removing the testicle chilled will, and if applicable held up by a bag becomes. This promotes the drainage of the tissue fluid from the scrotum and accelerates the swelling. The cooling prevents any further flow of fluid into the scrotum and relieves some of the pain.
Can also be supportive NSAID-class pain relievers be taken, i.e. non-steroidal anti-inflammatory drugs. This group includes, among others Ibuprofen, and Paracetamol.
If there is an unchecked influx of tissue fluid into the scrotum, there is a risk that testicles, epididymis, etc. Spermatic cords pinched off - after all, the testicles and the scrotum have only limited flexibility. If this is the case, must operational Make an incision on the testicle to relieve the pressure. This incision does not impair the function of the testicle or epididymis, but is placed very superficially on the tough connective tissue capsule.
In addition, of course, plays the Treatment of the underlying disease an essential role. Usually this is already diagnosed, if not, a diagnostic exclusion of other diseases must be made, since inflammation of the testicle alone occurs rather rarely.
The swelling and pain in the testicles decrease again within a week, and faster with appropriate therapy. However, there is one bacterial cause before, must Antibiotics be taken. These only work against bacteria, but not against viruses. No broad spectrum antibiotics are given, but a pathogen determination is carried out first and then specially tailored antibiosis are prescribed. Although broad-spectrum antibiotics would also show their effect, efforts are always made to find an antibiotic that fits as closely as possible in order to have another antibiotic on hand in the event of pathogen resistance. The antibiosis is used for Taken for at least 7-10 days, even after the symptoms have subsided. This is important, as otherwise the pathogen may germinate again.
diagnosis
The diagnosis is made by palpation of the testicle. Swelling, tenderness, and pain suggest inflammation. Also the History of origin is important for the doctor: Did the pain come on suddenly or over the course of weeks? If the symptoms point towards inflammation of the testicle, further diagnostic tools are needed. So can a Ultrasound of the testicle to represent. For this purpose, an ultrasound head is simply placed on the testicle using contact gel, and the structures of the testicles and epididymis are shown. Already here you can Recognize swellings as accumulations of fluid very well, and make a diagnosis quickly and easily. The next steps are then Examination of the blood, and the urine for any pathogens. The pathogen is searched for in the laboratory and usually takes no longer than 1-2 days. Once the pathogen has been found, either an appropriate antibiotic can be administered or at least conclusions can be drawn about the nature of the viral disease. Appropriate treatment follows immediately after the diagnosis and is usually carried out in an inpatient setting.
Inflammation of the testicle in the child, toddler and baby
Diseases are always particularly problematic in toddlers, as verbal communication between parents and child is not yet possible. So it cannot be explained to the baby that it is only a temporary condition that will surely pass soon. Small children therefore need special care and attention from their parents. The immune system of children is not fully developed until the age of 10, which is why they are much more susceptible to bacterial and viral infections. The spectrum of pathogens can also vary. So will inflammation of the testicle in children much more often from salmonella, or Pneumococci caused than by the spectrum of pathogens from which adults are affected. Children are also affected by classic childhood diseases such as mumps. A good third of all children infected with mumps develop inflammation of the testicle. Also after the mumps-measles-rubella vaccination (MMR for short), orchitis developed in individual cases. In young children, it is important to palpate and inspect the body thoroughly. Inflammation of the testicles may not be the first thing you think about when a baby cries. That is why a detailed inspection is necessary. Frequent crying due to the pain, a swollen scrotum, which should be noticed when changing diapers at the latest, and fever as a result of infection are symptoms that should be presented to the hospital. Non-treatment can lead to the complete loss of function of the testicle. It is also associated with severe pain and the risk of systemic spread.