Inflammation of the facial nerves
introduction
Inflammation of a facial nerve is usually a very painful affair that requires prompt treatment. Inflammation of a nerve in general is called neuritis, the occurring Nerve pain also as neuralgia designated. Neuralgia can also be caused by non-inflammatory processes. In the case of inflammation, various Facial nerves to be affected. Depending on the area that the nerves supply (innervate) with pain and tactile sensations, the pain occurs in different regions and can provide information about the localization of the inflammation.

Can stress be a cause?
The causes of inflammation of the facial nerve are manifold. Usually, stress isn't the only cause. But physical and psychological stress can trigger pain attacks and other complaints. Stress can make symptoms worse.
This can be explained by various mechanisms that take place in our body during stress reactions. Stress causes the release of various hormones and substances. These act as messenger substances in our body. These messenger substances lead to various processes in our body. The cells communicate via these messenger substances. Among other things, there are changes in various vessels. Subsequently, substance P is likely to be released as part of an inflammation of the facial nerve. Substance P activates the pain receptors. The sensory perception of pain is transmitted to the brain.
In addition, vascular changes caused by stress can compress branches of the facial nerve. In this way the symptoms can be triggered.
In addition, nerve branches can be damaged by compression. The damage to the nerve in turn leads to the pain center in the brain being over-activated. Sodium channels are increasingly being built into the brain. This leads to a faster and more sensitive pain perception.
In addition, the severe pain attacks trigger psychological stress. As a result, more substances and hormones are released which promote irritation of the branches of the facial nerve. Colloquially, a vicious circle arises. This is also called vicious circle in technical terms.
You can find more information on symptoms of stress here.
causes
There are many reasons why a facial nerve can become inflamed. Neuritis is often associated with previous damage to the nerve tissue. This can happen, for example, through constant pressure on the nerve tissue, which can be triggered by tissue changes or tumors.
Toxic neuritis, as the name suggests, is caused by poisons (toxins). Relevant are not only pollutants coming from outside (e.g. heavy metals), but also metabolic toxins, such as those caused by diabetes mellitus or chronic alcoholism.
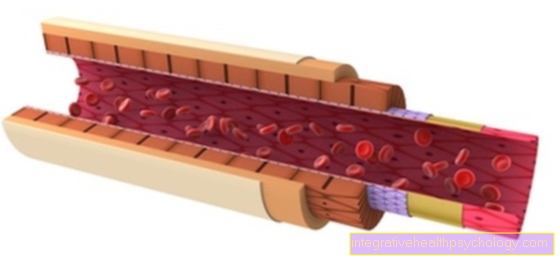
If the nerve is subjected to mechanical stress, for example if it is severed, torn or crushed, this can result in traumatic nerve inflammation. Often the cause is the contact between a blood vessel in the brain and the nerve. The conduction pathways rub against each other and the protective sheath (myelin sheath) of the nerve is worn out - irritation and false stimulation occur, for example the pain fibers.
Another source of inflammation can be multiple sclerosis. In this chronic inflammatory disease of the central nervous system (CNS), the myelin sheaths are attacked and dissolve. While the causes mentioned above are not transferrable, neuritis as a result of infection with bacteria, viruses or other microorganisms can also be dangerous for contact persons. A variety of pathogens can affect the CNS and cause inflammation in the facial nerve.
Read more on the topic: Shingles of the eye
Symptoms and facial neuralgia
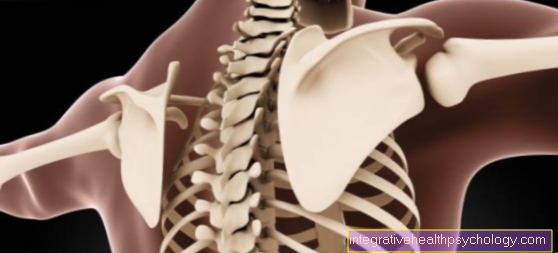
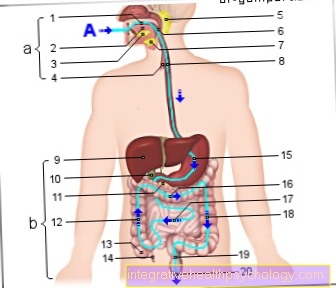
Inflammation can affect various facial nerves. There are 12 so-called cranial nerves. These are so named because they are directly connected to the brain and have no contact with the spinal cord. Only two of these nerves contain sensitive nerve fibers - fibers that can sense touch and pain - the trigeminal nerve and the glossopharyngeal nerve.
The trigeminal nerve ("triple nerve") divides into three main branches that supply the face (with eyes, nose and mouth), the teeth and the front two-thirds of the tongue. These are the ophthalmic nerve ("eyeball nerve"), the maxillary nerve (upper jaw nerve) and the mandibular nerve ("lower jaw nerve").
The glossopharyngeal nerve, the second sensitive cranial nerve, supplies the middle ear and throat, as well as the back third of the tongue with nerve branches that are sensitive to touch and pain. In addition, sensors that measure and influence blood pressure are connected to the brain via a branch of the glossopharyngeal nerve. If these nerves are inflamed, it can happen that information is misdirected. The nerves are irritated and send false pain signals, for example. This is called neuralgia.
Find out more about the topic here: Nerve inflammation on the face.
Pain associated with neuralgia
The symptom of pain associated with inflammation of the facial nerve can be differentiated in several ways. A distinction must be made between acute pain and chronic pain.
The acute pain arises due to an acute trigger. The acute pain has a protective function and is a warning signal. It correlates with the trigger.
That means if the blow or injury or inflammation to the face is severe, the pain is severe too. If the damage is minor, the acute pain that can be triggered is also relatively minor.
If the pain is chronic, it is independent of the trigger. They have no protective function.
Furthermore, one can determine the qualities of the facial pain in order to find out whether the nerves, muscles and / or bones in the face are affected. The quality of pain in the face can also be divided into deep and surface pain.
The deep pain here usually refers to pain emanating from the facial muscles and facial bones.
Surface pain on the face occurs when the skin of the face is injured. Here one differentiates the 1st from the 2nd pain. The first pain is usually described as bright and easy to localize. The second pain has a dull pain character and is difficult to distinguish. This quality of pain is also often described in terms of deep pain.
Read more about pain therapy.
The different qualities arise due to the different nerve fibers that guide the pain. Neuropathic pain can develop as the facial nerve becomes inflamed. That means that the pain comes from the nerve cell, the neuron. This leads to hyperactivity of the pain perception system in the brain. Neuropathic pain is described as burning, electrifying, very strong, and often devastating.
Trigeminal neuralgia
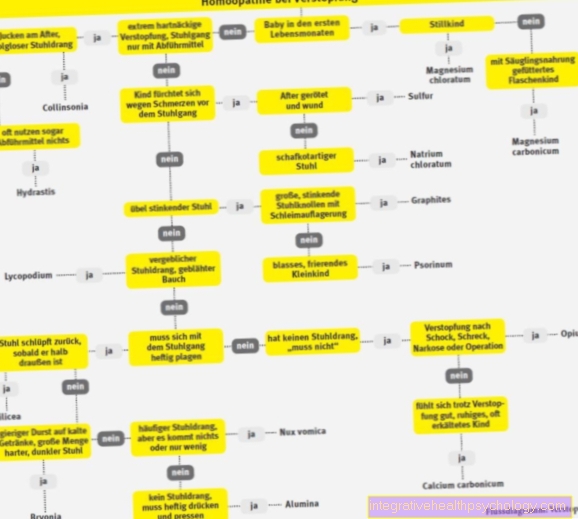
When the trigeminal nerve becomes inflamed, neuralgia can occur. This can be divided into two forms. If the cause of the nerve pain is unknown, it is called idiopathic neuralgia. If the cause is known, one speaks of symptomatic neuralgia.
In trigeminal neuralgia, the jaw branches of the nerve are most often affected, but usually only on one side. The branch of the eye is affected in the case of symptomatic neuralgia, for example caused by masses.
Trigeminal neuralgia is described as a lightning-fast, electrifying, burning, extremely strong, stabbing pain in the supply area of one or more trigeminal nerve branches. The pain counts as neuropathic pain. The pain attacks can occur spontaneously. But they can also be triggered by certain triggers such as chewing, speaking, swallowing, brushing your teeth or the like.
In classic trigeminal neuralgia, the cause is mostly unknown. It is also called idiopathic trigeminal neuralgia. However, the underlying mechanism, the so-called pathomechanism, has been researched in part. The research is still ongoing. It is believed that the pathomechanism is related to a "vascular-nerve conflict". This means that a vessel compresses one or more nerve branches of the facial nerve. Probably this is the A. cerebelli superior.
This is usually due to a degenerative change in the blood vessel. This can then lead to permanent irritation of the facial nerve. The pulsating branch of the vessel can pinch the nerve. In the long run, the isolation of the trigeminal nerve can be damaged. This isolation is also known as the myelin sheath. If this is damaged or missing, there may be direct contact between sensitive fibers that transmit pain. This can lead to the pain attacks that are characteristic of trigeminal neuralgia.
The attacks are repeated several times a day (up to 100 times and more). Those affected are often so plagued by their pain that a significant psychological impairment up to depression or suicidal thoughts can be observed.
Read more about trigeminal neuralgia.
Irritation of the facial nerves
In classic trigeminal neuralgia, the pain attacks begin spontaneously, without external irritation. In the process, external stimuli can trigger the pain attacks. In advanced trigeminal neuralgia, there are different triggers. These can be chewing, speaking, swallowing, drinking, brushing teeth, cold drafts, facial movements or touching.
This can severely limit the quality of life of those affected and put a lot of strain on them emotionally. Because depending on the trigger, patients can only partially predict, control or prevent the triggering of a pain attack. This is the reason why many affected people no longer leave their homes or homes. Also, some patients avoid washing and shaving that area of their face as these activities can cause irritation to the facial nerve.
The level of suffering with classic trigeminal neuralgia is very high. In the course of the illness, mood changes can occur accordingly. Unfortunately, these reactive, resulting fears and depressive moods are often wrongly regarded as the "cause" of the disease.
Duration
The pain attacks of classic trigeminal neuralgia are typically short-lived. They rarely exceed 2 minutes. Often the symptoms only appear sporadically. Symptoms can be free for weeks or months. However, these attacks can also occur up to about 100 times a day.
Persistent pain does not usually occur. There is a relative freedom from symptoms between the pain attacks. Since the pain is often described as "devastating", those affected also suffer between attacks. Fears of the next attack of pain can arise.
Depending on the cause, the pain attacks can occur from a few days to many months or even persistently for years if left untreated. In some cases an atypical facial pain occurs that does not correspond to the described pain character and duration.
Read more on the subject at: Duration of an inflammation of the nerves - what you should be aware of!
Paralysis
Temporary paralysis can occur if corresponding motor nerve fibers of the face are severely irritated or damaged. This can happen during a migraine attack, for example. Therefore, among other things, migraines can lead to brief facial paralysis. Since paralysis usually affects only one half of the face, temporary facial paralysis is often mistaken for a stroke. Because even a stroke can lead to paralysis on one side of the face. A stroke usually occurs, but not with the pain described.
Nevertheless, as a precaution, action should always be taken quickly, even if there is a slight suspicion of a stroke. An emergency doctor should be informed as soon as possible.
In some cases, inflammation of the facial nerve branches can also lead to persistent paralysis. A neurologist can best determine whether the paralysis is temporary or permanent. They can also find out the cause and initiate appropriate treatment. In the case of persistent paralysis of the face, speech therapy and / or occupational therapy treatments are usually advisable. Depending on the motor nerve branch failure in the face, speaking and / or swallowing can also be difficult.
Twitches
In the context of a classic trigeminal neuralgia, an uncontrollable twitching of the facial muscles in the affected area often occurs in the midst of a pain attack. One speaks here of clonic-tonic movements of the muscles.
After the pain attack, the affected area is no longer excitable for seconds to minutes. This means that shortly after an attack of pain, another attack cannot be triggered again directly by sensitive stimuli.
Nasociliary neuralgia (Charlin syndrome)
The nasociliary nerve ("nose-eyelash nerve") is a side branch of the ophtalmic nerve (1st main branch of the trigeminal nerve) and its branches supply the eye and nose with sensitive parts. If there is neuralgia due to the inflammation of the nasociliary nerve, unilateral pain occurs in the corner of the eye. Depending on the intensity, these can pull into the eye socket or the bridge of the nose. In addition, it can happen that there is increased tearing and multiple inflammations in the eye, that the nose swells or the skin becomes red. In nasociliary neuralgia, too, the pain attacks are triggered by a slight stimulation of the nerve - be it through touch or through movements while speaking or chewing.
Glossopharyngeal neuralgia
Glossopharyngeal inflammatory neuralgia is a rarely occurring pain picture. Typical for neuralgia are very strong, sharp attacks of pain. The pain area is mainly limited to the hypopharynx, the lower throat. The back third of the tongue, the tonsils (tonsils) and sometimes also the ear hurt, triggered by movements such as speaking, chewing and swallowing or coughing. Since the glossopharyngeal nerve also influences the heart, its inflammation can lead to a slowed heart rate and, in the worst case, to cardiac arrest.
Auriculotemporal neuralgia (Frey syndrome)
The auriculotemporal nerve ("ear-temple nerve") is a side branch of the mandibular nerve (3rd main branch of the trigeminal nerve). It guides the touch and pain sensations of the ear, the auditory canal, the eardrum and the skin in the area of the temple. The auriculotemporal nerve also has a connection to nerves that supply the parotid gland. If the nerve tissue is damaged by trauma, surgery or inflammation, or if the parotid has to be removed (resection), auriculo temporalis neuralgia can occur.
You can find more about desem syndrome on our page for Frey syndrome
For example, after an operation on the parotid gland, various complaints can occur. Only the symptoms that affect the facial nerves are described here.
As part of complications, irritation or injury to the facial nerve can lead to numbness and paralysis of the operated face. The symptoms can be temporary or long-lasting.
If the parotid gland has been completely removed, throat sweating can result. This means that those affected sweat in the cheek area after eating. In addition, reddening of the skin, a feeling of swelling, tingling and burning pain in the cheek area can be triggered. By injuring parasympathetic facial nerve fibers, these can come into contact with the sympathetic sweat glands of the skin of the cheek. Both use the messenger substance acetylcholine, via which the cells communicate with one another. This can lead to the symptoms described above. This phenomenon is also known as Frey's syndrome or auriculotemporal syndrome, gustatory hyperhidrosis or gustatory sweating.
To treat the relatively special clinical picture of Frey syndrome, the patient is injected with botulinum toxin A, which paralyzes and thus inactivates the corresponding sweat glands.
In addition, surgery on the parotid gland can also damage facial nerve branches. This damage can result in restrictions in the facial muscles. The corner of the mouth hanging on one side is often evident. Depending on the damage to the branches, there may also be an inability to close the eyelid.
Sluder neuralgia
Sluder neuralgia is an attempt to explain some idiopathic facial neuralgia. The nerve fibers of the nerve node “pterygopalatine ganglion” are supposed to falsely stimulate fibers of the trigeminal nerve, which runs adjacent to its main branches. Inflammation could lead to damage to the nerve tissue that would allow such an interaction.
Atypical facial pain
Atypical facial pain does not have the character of neuralgia. There is constant dull pain, mostly of unclear origin. Similar to trigeminal neuralgia, the patients suffer from the psychological stress that arises from the pain symptoms and increasingly show mental illnesses such as depression, obsessive-compulsive disorder or anxiety disorders. The stimulation of the pain fibers through a previous inflammation with subsequent scarring of the tissue is possible, but the psyche of the patient often plays a major role in this clinical picture.
Toothache in neuralgia
If the upper or lower nerve branches on the face are affected, misinterpreted toothache is more common. The nerve branch of the upper jaw is used in technical language Ramus maxillaris called. The nerve branch of the lower jaw is called Ramus mandibularis designated.
If the Ramus maxillaris is affected, the pain can spread to the teeth of the upper jaw, upper lip, nostrils, nasal mucosa, and roof of the mouth. If the Ramus mandibularis Damage can lead to pain in the lower lip, tongue and toothache in the lower jaw.
Those affected often clench their jaws reflexively in the pain attack. Due to the attack-like, typical pain character, actual toothache can be distinguished.
You can read more about toothache here.
Is Neuralgia Contagious?
Generally speaking, neuralgia is not contagious. Inflammation of the facial nerve can have several causes. Shingles of the face and other infections can develop into neuralgia.
If there is temporary irritation of the facial nerves due to a cold, the cold is contagious. Shingles on the face, for example, can also be contagious for people who have not yet had chickenpox. As a result, these people can develop chickenpox.
But inflammation of the facial nerve branches or classic trigeminal neuralgia are not contagious according to current knowledge.
therapy
The focus of the treatment should be the relief of the nerve and the removal of the source of irritation. Only then can the nerve tissue regenerate and flatten the inflammation. The two main approaches here are drug therapy and surgery. In terms of medication, anticonvulsants such as Carbamazepin® or Valproat® are used. They contain active ingredients that are also used in the therapy of epilepsy and slow down the transmission in the nerve cells. This lowers the stimulus threshold and the stimulation of the pain fibers stops. Anticonvulsants are usually well tolerated, but can also cause side effects such as tiredness or dizziness. The more effective Phenytoin® should be used for acute painful conditions.
Antidepressants can provide relief for atypical facial pain, but an inflammatory cause of the disease is unlikely. Taking pain medication is not an option with long-term therapy. There is a risk of dependence and often the development of tolerance weakens the effect of the medication.
There are several options intraoperatively. First, a long-term local anesthetic (narcotic) can be injected into the nerve or nerve node. If the procedure remains ineffective, the nerve can either be relieved or blocked entirely. If there is a superficial brain tumor, surgical removal is always recommended. An overlying vessel can be prevented from continuing to compress the nerve tissue by implanted muscle cushions (Jannetta's operation). A permanent blockage of the nerve is only possible through destruction. In operations where the skull does not have to be opened, the nerve tissue can be effectively destroyed by heat, by chemical substances such as glycerine or by pressure, in the balloon compression procedure. As a last resort, the nerve can be surgically severed, losing any function.
If the cause is an infection by microorganisms, an appropriate drug must be prescribed, for example an antibiotic.
forecast
The Chances of recovery are depending on the cause of the inflammation to be classified differently. If the disease is due to a pathogen, the counter-therapy can provide complete relief. With surgical interventions, depending on the procedure, there is a 90-98% probability of being able to live painlessly afterwards. However, 10-30% of patients develop pain syndrome again over the years.

.jpg)