Epileptical attack
synonym
Seizure
definition
A epileptical attack is a temporary malfunction of nerve cells Of the whole Brain or parts of it. This is typical of a seizure sudden onset the dysfunction that is caused by, for example Muscle twitching, but also through sensitive symptoms how tingle can express.
The epileptic seizure is clinically divided into its seizure form and can unique or extremely rare occur and then will Casual fit called. For example, children who cramp from an infection have an occasional seizure.
It is also important to say that an epileptic seizure is not the same as a diagnosis of epilepsy, since the seizure is merely a symptom.
You can find more about epilepsy here: epilepsy.

frequency
The epileptic seizure does not occur infrequently, it even does fairly common occurrence.
Especially Children with rapidly rising fever have a seizure more easily.
Up to the age of 80 had about 10% of the population for example one or more epileptic seizures, but a maximum of 0.5-0.6% of the population suffer from epilepsy.
Basically every person can have one or more seizures, as every brain has the ability to generate an epileptic seizure. Especially if a Acutely damaged brain will, or certain risk factors seizures occur more easily.
These factors include:
- Poisoning
- severe infectious diseases
- Lack of oxygen
- Drop in blood sugar
- accidental brain injury
- sleep deprivation
- Alcohol consumption as well as alcohol withdrawal
- Drugs
- Meningitis.
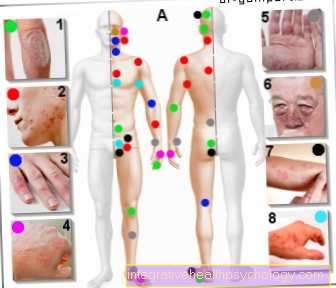
Symptoms
As already mentioned, epileptic seizures can affect small areas of the brain or all neurons (= nerve cells) in the brain.
The symptoms are just as varied:
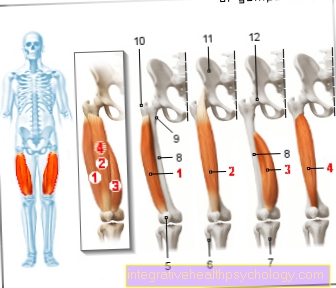
- Motor disorders such as muscle twitching in a single muscle group such as the biceps and upper arm muscles can occur.
- Likewise, sensory signs (affecting the senses) can also show up during a seizure, such as a strange, inexplicable smell.
- For a brief moment, other people affected seem trodden away or fiddling with their item of clothing.
Usually an epileptic seizure does not last longer than two minutes. Some are responsive or slightly cloudy during the seizure, while others appear to be completely unconscious. Most of the time, those affected are still a bit dazed after their seizure and need a little time to collect themselves. If someone has seizures more frequently, the type of seizure can often be determined, which means that their seizures usually always proceed in the same way.
Classic, generalized, epileptic seizures can also present themselves very differently, but are always associated with a disturbance of consciousness. This means that the person concerned is not conscious and can usually not react adequately, for example, to being spoken to. In retrospect, there are usually no more memories of the seizure. In addition, the entire muscles suddenly relax (atonic phase), which results in a fall in which the person concerned cannot catch himself and can therefore seriously injure himself.
A tonic phase often takes place at the beginning of an epileptic seizure, which means that the entire muscles of the affected person are maximally tensed. Arms and legs are usually hyperextended. Other components of the seizures are jerky, unsystematic muscle twitches (so-called Myoclonia), especially the arms and legs. These can change into rhythmic muscle twitching (clonic phase). After the actual attack, one speaks of one postictal phase in which sufferers are asleep or confused.
A true epileptic seizure usually stops breathing, causing the person's lips and face to turn blue during the seizure. The eyes are usually open during an attack.
An important term to be associated with seizure patterns is the term aura.
Some seizures begin with a typical aura. The one about to have a seizure notices strange sensations such as:
- Visual disturbances
- tingle
- Hallucinations
- a strange feeling in the stomach
- the feeling of floating
- Difficulty concentrating
- strange smell or taste impressions.
Certain aura forms can be used to find the cause or the area of the brain in which an epileptic seizure is generated.
Seizure forms
The International League Against Epilepsy (ILAE) classified the various seizure patterns and epilepsies.
Therapy then follows according to this classification.
Characteristic for partial seizures is that they consist of one very specific area in the brain come. For example, this location can be a Brain scar caused by trauma. Since the Often times, use imaging techniques such as an MRI or CT scan to pinpoint the location of the seizure leaves, this is often called focal seizure described.
Furthermore there is focal seizures, which spread over the whole brain in the process. These are divided into a separate category into which the secondary generalized seizures.
The third classification remains generalized seizures left over, which spread to the entire brain from the start. A reason for this type of epilepsy is rarely found. Most of the time, people also suffer from a loss of consciousness.
The ILAE shared the seizure patterns additionally in subgroups on. The most important are listed again here:
Both partial seizures is between complex and simple seizures distinguished. The big difference here is that the simple-partial seizure with full awareness plays and people often an aura to have. Both complex-partial seizures is this Consciousness mostly clouded and people are often not responsive, wandering aimlessly, smacking their lips or making faces.
Both generalized seizures there are several subgroups:
Absence:
That's how you describe a short pause in consciousness. Those affected are typical as if frozen, busy and completely absent. Most of the time the absence only lasts few seconds to a maximum of half a minute. Afterwards, those affected simply continue with their work as if nothing had happened. This type of seizure is often with School children detectable.Myoclonic seizures:
when fully conscious it suddenly comes to Twitching of individual muscles or muscle groups for example in the foot, leg or trunk. They just last few seconds and end abruptly.Tonic seizures:
they are mostly just short events. It is a abrupt spasms of muscleswithout a rhythmic twitch. In addition, there is clouding of consciousness and falls.Clonic seizures:
the up to several minutes persistent seizures are a rhythmic contraction of muscle groups. People often fell and could injure themselves as a result.Tonic-clonic seizures:
is also known as Grand Mal seizure designated. Often this one goes Aura aheadthat through a acute loss of consciousness is terminated. Usually it comes to a so-called Initial scream at the beginning of the tonic-clonic seizure and to Fall. First the Grand Mal starts with a one half-minute cramping of the whole bodythat by a just as long rhythmic twitching is alternated. During the seizure the person concerned often wets himself, bites his tongue sideways or educates Foam at the mouth. After such a grand time sleep the people often because they are still very dizzy. Most of them wake up completely disoriented and confused. The person cannot actually remember the seizure.
Status epilepticus
A Status epilepticus is referred to as such if a The seizure lasts longer than ten minutes or if there is one Series of seizures exist, between which there is no complete recovery more can take place. In addition, the series must last longer than half an hour. The status epilepticus is a life threatening event and it must an ambulance immediately be called.
Causes of Epileptic Seizure
The exact cellular (related to the cell) Disruptionscausing an epileptic seizure not yet fully understood. A sudden discharge of neurons on the covering of the gray cells plays a major role. That means the important channelsused for the transportation of sodium, potassium and calcium are responsible have one Malfunction (Dysfunction). These dysfunctional channels cause you Deficiency of the inhibitory neurotransmitter GABA (Gamma Amino Butter Acid), which has a preventive effect on seizures.
In addition to the lack of those transmitters, there appears to be one Excess of the neuron-activating transmitter substances glutamate and aspartate. They are substances that promote seizures. Besides these factors you can also genetic malformations or from external influences (Blood sugar drop, severe infection, etc.) can be a reason for an epileptic fit to develop.
What are the typical triggers?
Epileptic fits and other seizures can be caused by a variety of triggers (Trigger) to be triggered. Those affected are often more susceptible to seizures (increased epileptogenicity, lower seizure threshold) for a variety of reasons, but the triggers listed here can also trigger seizures, so-called occasional seizures, in healthy people.
People with increased susceptibility and epileptic diseases are more often affected. Under certain circumstances, however, the susceptibility is only increased in relation to certain triggers. The most common cause in adulthood is alcohol withdrawal, the most common cause in childhood is fever.
In addition to alcohol withdrawal, there are other substance-dependent triggers such as drug withdrawal, the use of drugs (especially ecstasy and cocaine), as well as certain drugs that can cause seizures as part of side effects (e.g. penicillin, neuroleptics, amitriptyline (antidepressant)). In addition to fever, other illnesses can also trigger seizures, such as eclampsia in pregnant women, an electrolyte shift in the blood (e.g. in kidney diseases) and a massive, non-physiological decrease in blood sugar (hypoglycemia, especially due to insulin overdoses).
In addition, certain situations, especially in people with increased susceptibility, can trigger epileptic seizures, including sleep deprivation, excessive physical exertion and stroboscopic light (rapid change from light to dark).
Stress as a trigger
Stress alone can cause seizures. In general, these are not epileptic, but non-epileptic, psychogenic or dissociative seizures, mostly in the context of a serious psychosomatic illness.
In people with epilepsy, the frequency of epileptic seizures can be increased during periods of severe psychological stress.
Alcohol as a trigger
Alcohol itself does not trigger epileptic seizures, but rather withdrawal from alcohol. Alcoholic people are particularly affected by this. The attack occurs when the alcohol consumption is reduced rapidly after a long period of regular consumption. Usually these are the classic epileptic seizures (tonic-clonic) and only rarely about focal seizures of all kinds.
Three to four seizures usually occur within the first 24 hours after the last alcohol consumption. This is one of the reasons why alcohol withdrawal should be done in a qualified clinic. Here the seizures can be prevented with the help of medication. After a single attack of alcohol withdrawal, no antiepileptic therapy is necessary due to the good prognosis.
Brain tumor as a trigger
An epileptic seizure can always occur in the form of a so-called symptomatic seizure as a symptom of a brain tumor. The tumor presses on other parts of the brain, which can become more excited, which can lead to epileptic seizures.
An imaging diagnosis in the form of an MRI (magnetic resonance tomography, nuclear spin) can provide clarity here. From the outside, these seizures cannot necessarily be distinguished from other epileptic seizures.
Read more on the topic: Brain tumor
Epileptic seizure after a cerebral haemorrhage or stroke
If epileptic seizures occur after a stroke or cerebral hemorrhage, it is referred to as symptomatic epilepsy. Due to the brain cells that have died as a result of the stroke, various areas of the brain can become overexcited. If these are stimulated by typical triggers such as flickering light, a massive electrical discharge of the affected brain cells occurs (Neurons) and thus to an epileptic seizure.
An epileptic seizure can also occur spontaneously, i.e. without a recognizable trigger. This form of symptomatic epilepsy can be difficult to treat with medication. A specialist in the form of a specialized neurologist should be consulted. With treatment, the risk of recurring seizures is approximately 65% within two years.
Epileptic fit while sleeping
Epileptic seizures can also occur during sleep. In general, these can be perceived as such by the affected person or partner, but especially when the affected person sleeps alone, the seizures can be difficult to diagnose.
Typical warning signs are sore muscles without explanation and a tongue bite. These are usually associated with increased tiredness and sleepiness. In order to get to the bottom of the matter, an examination in the sleep laboratory should be carried out in a qualified clinic (Polysomnography). For this, the person concerned spends the night in the hospital. She is under constant observation and cardiac currents (EKG) and brain waves (EEG) supervised. Usually such a diagnosis can be made.
Epileptic seizure in the child
Epileptic seizures and seizures in children and babies can have a variety of causes.In addition to spontaneous seizures without an identifiable cause and usually without repetition and disease value, febrile seizures are the most common form of seizures in children. Typically febrile seizures occur in children between the ages of six months and five years. If febrile seizures occur outside of this time window, it is referred to as a complicated febrile seizure and a detailed diagnosis should definitely follow (for example in a children's hospital).
Febrile convulsions occur when the fever is high or when the fever rises or falls rapidly. About three to four percent of all children will develop a febrile seizure in their lifetime. A pediatrician should always be consulted afterwards. However, a febrile seizure is not an epileptic attack and normally does not harm the child's brain. It comes about due to the immaturity of the not yet fully grown brain, which does not react properly to the fever. If you have a febrile seizure for the first time, you should still go to a pediatrician or a hospital as soon as possible; the emergency services can also be notified immediately.
Other epileptic convulsions in childhood can arise as a symptom of certain epileptic diseases. Most of these diseases have a good prognosis if properly treated. In rare cases, a seizure can also be a symptom of a brain tumor, which is rare in children but more common than in adults. In any case, every seizure should be followed by a diagnosis by a pediatric neurologist, as is available in most children's hospitals.
You might also be interested in these topics:
- Febrile seizure
- Epilepsy in the child
Diagnosis
The diagnosis of an epileptic seizure always includes an initial consultation in which the doctor will ask certain questions:
- When was the time of occurrence?
- Where was the attack?
- Was there a recognizable trigger?
- What signs were seen by outsiders during the seizure?
- Did you have typical aura symptoms (taste, smell, tingling, etc.)?
Since many other clinical pictures could come into question, a detailed physical examination must be carried out. Circulatory disorders and metabolic diseases, but also depression, anxiety or migraines can manifest themselves in a similar way to an epileptic seizure.
Imaging diagnostics must also be performed for a purely physical examination. Here the EEG (electroencephalogram) play a crucial role. With the EEG, important causes for the development of convulsions can often be filtered out. However, one must not forget that in many cases the EEG can be completely normal during an attack
Another important examination is the EKG, as a cardiac arrhythmia should be excluded as a cause of a circulatory collapse.
In addition, a blood test should be carried out. The main focus here is on liver and kidney values, blood electrolytes and blood sugar. After a seizure, the enzyme creatine kinase is often elevated, which is why this value is often examined.
A lumbar puncture is also used from time to time as a diagnostic tool, since brain inflammation (Encephalitis) can cause epileptic fits.
Further imaging of the brain using MRI is used to rule out or secure an epileptic seizure. Especially when certain risk factors such as circulatory disorders or other injuries in the brain show up that make epileptic seizures more likely.
First aid in an epileptic fit
Now, when you see someone having an epileptic seizure, you need to stay calm first, as the seizure usually ends after two to three minutes. The space around the convulsive person should be cleared as freely as possible (for example, put away chairs) so that the convulsive person does not get injured. The ambulance service should then be called immediately (112).
Under no circumstances should the head be supported or the convulsing person be held, as this increases the likelihood of injuries for both the convulsing person and the helper massively. Most people are unconscious after the seizure. You should check whether you are breathing and then you should be brought into the stable lateral position. Regular checks should also be made to ensure that the person is still breathing while waiting for the ambulance service.
If breathing stops, cardiopulmonary resuscitation should be initiated. If possible, it is also good to look at the clock when the seizure begins in order to be able to give a good estimate of the duration of the seizure afterwards. Without a watch, even experienced people tend to overestimate the duration of a seizure significantly.
There are also emergency medication, but these are only used for an attack that lasts longer than five minutes. A benzodiazepine that is administered rectally (through the anus) or through the nose or mouth is an option.
Read more on the topic: Tavor Expedit
Medicines used to treat epileptic seizures
There are a variety of anti-epileptic drugs that are used depending on the cause of the seizure. Advice from a specialized neurologist is essential here. Advice on specific situations must also be given. For example, some of the drugs must not be taken during pregnancy as they can harm the unborn child (for example: valproate and carbamazepine).
Many of the drugs also put a lot of strain on the liver (for example: valproate), and alcohol consumption may have to be reduced accordingly.
Read more on the topic: Drugs for epilepsy
What are the consequences of an epileptic fit?
The consequences of a single epileptic seizure are usually not very serious. In addition to the social consequences (driving ban), acute injuries can occur. In addition to bruises and tongue bites, broken bones can also occur, as well as concussions and the like due to the fall at the beginning of the attack. In addition, most people feel exhausted after an attack. In addition, there may be temporary symptoms such as depressive mood, speech disorders, paralysis and forgetfulness.
If you have frequent attacks, you are more likely to develop depression than the healthy population. Single seizures do not cause brain damage. Whether there is permanent damage or a reduction in life expectancy depends largely on the cause of the epilepsy.
With some epileptic seizures, there is a risk of the person going into a status epilepticus, which is a particularly long-lasting and severe epileptic seizure. This increases the likelihood of serious consequences because the brain is not supplied with oxygen for a long time.
How can I prevent an epileptic fit?
Only when an epileptic disease is diagnosed does it make sense to take preventive measures. The most important is the correct intake of anti-epileptic medication. Here you should be in close contact with the doctor in order to adapt the medication so that on the one hand as few seizures as possible occur and on the other hand as few side effects as possible.
Furthermore, possible prophylactic triggers should be avoided.
Driving ban after an epileptic seizure
For reasons of intrinsic safety and the safety of fellow human beings, people are deprived of their driver's license after a seizure in accordance with legal requirements. A distinction is made between the normal car driver's license (group 1) and the truck driver's license and persons in passenger transport (group 2). In the event of a first seizure without evidence that epilepsy is present (occasional seizure), the driver's license is withdrawn for six months (group 1) or two years (group 2) in the event of an unprovoked seizure, and for three (group 1) or for symptomatic or provoked seizures six months (group 2).
The driver's license will be returned after this time, provided there was no further seizure. In the case of epilepsy, the driver's license can be returned after one year of seizure-free status (whether with or without therapy) (group 1). Group two can only get their driving license back in the case of epilepsy if there have been no seizures for five years without treatment; normally a change of occupation is necessary.
In the event of persistent seizures, the driving license cannot be returned. An exception are seizures that do not impair the ability to drive, such as seizures that only occur while sleeping.